Figure 3.
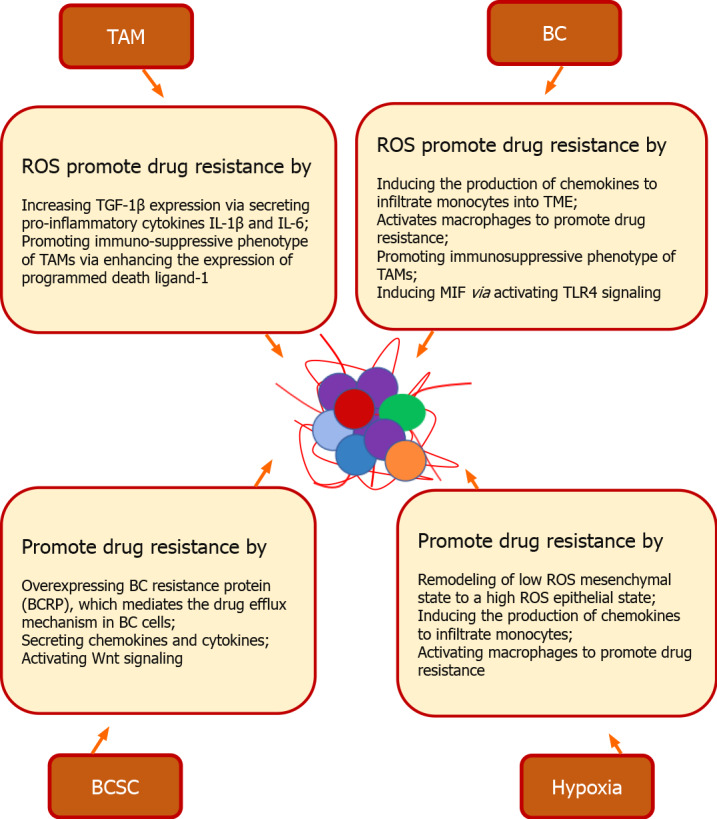
Cancer stem cell and redox mediated drug resistance in breast cancer. In breast tumor microenvironment (TME), a fine orchestration between breast cancer (BC) stem cells (BCSC) and TME cells promotes drug resistance. BCSC promote drug resistance by overexpressing BC resistance protein, which mediates the drug efflux mechanism in BC cells. Stem cells derived from bone marrow, adipose tissue, and fibroblast enhances the drug resistance by activating developmental pathways via secreting chemokines and cytokines. Wnt signaling of BCSC along with glutathione overexpressing genes mediates resistance. Hypoxic TME promotes drug resistance by remodeling of cells from a low reactive oxygen species (ROS) mesenchymal state to a high ROS epithelial state. High ROS from cancer cells induces the production of chemokines to infiltrate monocytes into TME and activates macrophages to promote drug resistance. ROS also induces drug resistance by promoting the immunosuppressive phenotype of tumor-associated macrophages via enhancing the expression of programmed death ligand-1 via NF-κB (nuclear factor-κappa beta) signaling. Multinucleated cells promote drug resistance by increasing the secretion of vascular endothelial growth factor and macrophage migration inhibitory factor (MIF) via RAS/MAPK pathway-dependent hypoxia-inducible factor-1α. Macrophage derived ROS induces drug resistance by increasing transforming growth factor 1β expression via secreting pro-inflammatory cytokines interleukin (IL)-1β and IL-6. ROS also facilitates drug resistance by inducing MIF via promoting phosphorylation of ERK. via activating TLR4 (toll-like receptor 4) signaling. TAM: Tumor-associated macrophage; BC: Breast cancer; ROS: Reactive oxygen species; TGF: Transforming growth factor; IL: Interleukin; TME: Tumor microenvironment; MIF: Macrophage migration inhibitory factor; TLR: Toll-like receptor; BCSC: Breast cancer stem cell.
