Acute respiratory distress syndrome (ARDS) is responsible for the primary cause of death of patients with novel coronavirus disease 2019 (COVID-19) [1]. For severe ARDS patients, endotracheal intubation and mechanical ventilation are the standard treatment in an intensive care unit (ICU). Early and relatively long prone positioning (P.P.) has been proved effective in decreasing ARDS patients' mortality [2]. this report aimed to assess whether the prone position ventilation is associated with improved oxygenation and decreased morbidity for the patients with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
This retrospective, single-center study was conducted among the patients with SARS-CoV-2 admitted to the intensive care unit (ICU) of Huoshenshan Hospital in Wuhan, China. The institutional ethics review board has approved our study. Due to the present study's observational design and impaired consciousness of included patients, the written informed consent was waived. Inclusion criteria were (1) laboratory and CT-confirmed COVID-19; (2) aged 18–75 years; (3) endotracheal intubation and mechanical ventilation for severe ARDS (Berlin definition) for less than 48 h; (4) were under continuous infusion of sedatives. The main exclusion criteria were prolonged P.P. intolerance.
Forty patients who received mechanical ventilation in the prone position were included between Feb 9 to Apr 10, 2020.29 were males (72.5%); the Mean age was 70.7 years (54–89 years)0.23 patients were included in the supine group, while 17 patients were included in the prone group ( Table 1 ). The baseline characteristics of the two groups showed no significant difference. Fever (77.5%), cough (77.5%), dyspnoea (65%), and fatigue (75%). Myalgias (40%) were the common symptoms of included SARS-CoV-2 patient.
Table 1.
Baseline characteristics of included patients in the study.
| Characteristics | Supine group (N = 23) | Prone group (N = 17) | P Value |
|---|---|---|---|
| Age-yr., Md (range) | 72(54–89) | 69(56–87) | 0.217 |
| Male -no. (%) | 18(78.3) | 11(64.7) | 0.343 |
| Symptom onset to hospitalization-d, Md (range) | 13(4–61) | 14(5–46) | 0.742 |
| Coexisting conditions-no. (%) | |||
| Smoking | 2(8.7) | 1(5.9) | 1.000 |
| Hypertension | 11(47.8) | 6(35.3) | 0.860 |
| Diabetes | 8(34.8) | 4(23.5) | 0.675 |
| Coronary artery disease | 2(8.7) | 2(11.8) | 0.831 |
| COPD | 2(8.7) | 1(5.9) | 0.785 |
| Chronic kidney disease | 2(8.7) | 1(5.9) | 0.785 |
| Cancer | 1(4.3) | 3(17.6) | 0.393 |
| APACHE-II Score, Md(range) | 16(8–25) | 15(8–38) | 0.857 |
| ARDS level (Berlin definition) no. (%) | 0.516 | ||
| Mild | 2(8.7) | 0(0) | |
| Moderate | 7(30.4) | 5(29.4) | |
| Severe | 14(60.9) | 12(70.6) |
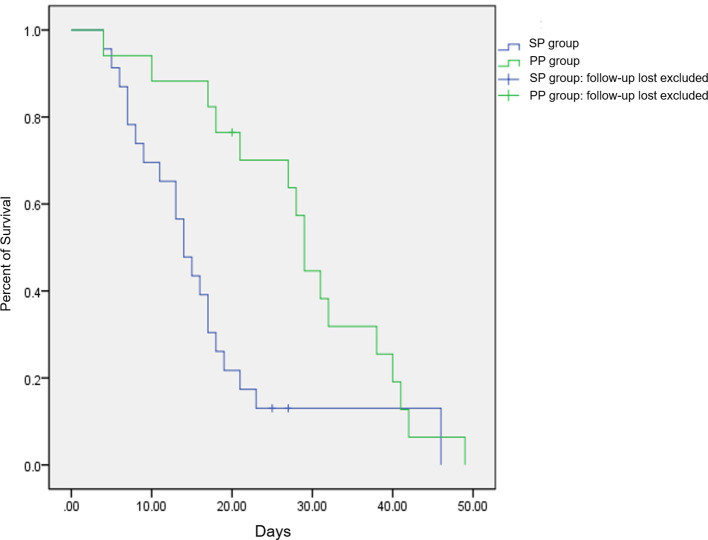
14-day mortality was 25% in 40 critically ill COVID19 patients who received intubated and mechanically ventilated. Among those who died within 14-day ICU admission, only 2 (11.8%) received long-term P.P. treatment, while 12 (52.2%) were maintained in a supine position, with a significant difference (x2 = 8.008, P = 0.005). Moreover, the patients who received P.P. therapy extended the median survival time (d, 95% CI) to the S.P. group (29(27.1–30.9) vs. 14(10.9–17.1), P = 0.005) with an HR as 0.37 (95%CI 0.18–0.76, P = 0.007) (Fig. 1 ). After adjusting for gender and age, the multiple Cox regression analysis of risk factors affecting survival outcome by forward stepwise regression has demonstrated the survival outcome was significantly adversely associated with severe ARDS level by Berlin definition (P = 0.002, HR = 1.956, 95%CI 1.227–2.973) and beneficially associated with P.P. therapy (P = 0.002, HR = 0.282, 95%CI 0.126–0.630). The factors of age, gender, time of symptom onset to hospitalization, smoking history, and APACHE-II score weren't significantly related to our included ARDS patients' survival outcome shown by multivariate Cox regression analysis.
Fig. 1.
Kaplan–Meier survival estimates during the 50 days following enrollment of the Covid-19 patients in the prone position (P.P., n = 17) or supine position (S.P., n = 23). Compared with the S.P. group, the P.P. therapy significantly improved the detailing overall survival rates in Kaplan–Meier survival curve (HR = 0.37(0.18–0.76), P = 0.007).
In this retrospective controlled study, we found a significant benefit associated with P.P. therapy and survival outcome by multivariate Cox regression analysis. Besides, the two groups survival outcome is also adversely associated with severe ARDS level, indicating Berlin definition as an effective index for critically ill COVID19 patient's prognosis. As high mortality from COVID-19-induced ARDS has been repeatedly reported [3], our 28-day ICU mortality of the P.P. group who were on mechanical ventilation was 35.3%, which is much lower than the S.P. group but nearly twice of the PROSEVA study [2] (Fig. 1).
Acute respiratory failure was still the main cause of death for intubated and mechanical ventilation COVID19 patients [4]. Older age (70.7 (54–89)), hypertension (17(42.5%)), higher APACHE-II score (15.6(8–38)), and severe ARDS level of Berlin definition (16(40%)) were strongly related to such a high intubated ventilation rate and mortality in our cohort ( Table 1 ), which was consistent with the previous reports highlighting the dismal impact of premorbid conditions and multiorgan damage on the most severe COVID-19 patients [5]. According to our data, No ARDS patient with a stabilized hemodynamics in the P.P. group couldn't endure 12 consecutive hours of prone positioning. ECMO should be applied when these measures have failed to maintain the hemodynamics and oxygen supply-demand balance, used in 5% of critically ARDS in our cohort (one from the P.P. group, one from the S.P. group).
This report's major strength is the controlled study of PP-treated intubated and mechanically ventilated COVID-19 patients from Huoshenshan hospital in Wuhan, China. We acknowledge several limitations to our study. First, the trends of SpO2, PaO2:FiO2, and breathe rate were not reported in this letter. According to the previous reports, persistent P.P. therapy could ameliorate ARDS patients' survival outcomes though improve those deoxygenation indexes. Moreover, this retrospective study was conducted in the single-center, with small sample size.
In conclusion, through a controlled study, we showed that prolonged prone position is a feasible and safe treatment to extend the survival time of intubated and mechanically ventilated COVID-19 patients.
References
- 1.Cummings M.J., Baldwin M.R., Abrams D., Jacobson S.D., Meyer B.J., Balough E.M., et al. Epidemiology, clinical course, and outcomes of critically ill adults with COVID-19 in New York City: a prospective cohort study. Lancet. 2020;395(10239):1763–1770. doi: 10.1016/s0140-6736(20)31189-2. Epub 2020/05/23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guérin C., Reignier J., Richard J.C., Beuret P., Gacouin A., Boulain T., et al. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med. 2013;368(23):2159–2168. doi: 10.1056/NEJMoa1214103. Epub 2013/05/22. [DOI] [PubMed] [Google Scholar]
- 3.Yang X., Yu Y., Xu J., Shu H., Xia J., Liu H., et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med. 2020;8(5):475–481. doi: 10.1016/s2213-2600(20)30079-5. Epub 2020/02/28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Piroth L., Cottenet J., Mariet A.S., Bonniaud P., Blot M., Tubert-Bitter P., et al. Comparison of the characteristics, morbidity, and mortality of COVID-19 and seasonal influenza: a nationwide, population-based retrospective cohort study. Lancet Respir Med. 2021;9(3):251–259. doi: 10.1016/s2213-2600(20)30527-0. Epub 2020/12/21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Krishnan S., Patel K., Desai R., Sule A., Paik P., Miller A., et al. Clinical comorbidities, characteristics, and outcomes of mechanically ventilated patients in the State of Michigan with SARS-CoV-2 pneumonia. J Clin Anesth. 2020;67:110005. doi: 10.1016/j.jclinane.2020.110005. Epub 2020/07/25. [DOI] [PMC free article] [PubMed] [Google Scholar]