Abstract
Aims
Timely referrals for transplantation and left ventricular assist device (LVAD) play a key role in favourable outcomes in patients with advanced heart failure (HF). The purpose of the Catheter Ablation for atrial fibrillation in patientS with end‐sTage heart faiLure and Eligibility for Heart Transplantation (CASTLE‐HTx) trial is to test the hypothesis that atrial fibrillation (AF) ablation has beneficial effects on mortality and morbidity during ‘waiting time’ for heart transplantation (HTx) or to prolong the time span until LVAD implantation.
Methods and Results
CASTLE‐HTx is a randomized evaluation of ablative treatment of AF in patients with severe left ventricular dysfunction who are candidates and eligible for HTx. The primary endpoint is the composite of all‐cause mortality, worsening of HF requiring a high urgent transplantation, or LVAD implantation. The secondary study endpoints are all‐cause mortality, cardiovascular mortality, cerebrovascular accidents, worsening of HF requiring unplanned hospitalization, AF burden reduction, unplanned hospitalization due to cardiovascular reason, all‐cause hospitalization, quality of life, number of delivered implantable cardioverter defibrillator therapies, time to first implantable cardioverter defibrillator therapy, number of device‐detected ventricular tachycardia/ventricular fibrillation episodes, left ventricular function, exercise tolerance, and percentage of right ventricular pacing. Ventricular myocardial tissue will be obtained from patients who will undergo LVAD implantation or HTx to assess the effect of catheter ablation on human HF myocardium. CASTLE‐HTx will randomize 194 patients over a minimum time period of 2 years.
Conclusions
CASTLE‐HTx will determine if AF ablation has beneficial effects on mortality in patients with end‐stage HF who are eligible for HTx.
Keywords: atrial fibrillation, catheter ablation, heart failure, heart transplantation
Introduction
Accumulated evidence shows that patients with heart failure (HF) and atrial fibrillation (AF) benefit from catheter ablation in terms of hard endpoints. 1 , 2 , 3 AF is a progressive disease that is not only a consequence of structural, haemodynamic, and electrophysiological remodelling but also a cause of the same processes. It has been demonstrated that there is significant overlap between the risk factors and pathophysiological mechanisms of AF and HF. 4 Today, approaches to treat patients suffering from AF and HF depend mainly on which specialists are treating the patients. Electrophysiologists are more in favour of restoring and maintaining sinus rhythm, while the HF specialists tend to focus on alleviating acute symptoms independent from the underlying dominant heart rhythm. 5 Of note, the current data support substantial benefit for catheter ablation of AF in patients suffering from HF with reduced ejection fraction. 1 Advancements in ablation technologies and increased operator experience have drastically improved the safety profile of AF ablation in HF. Presumably, permanent conversion from AF to sinus rhythm could help to improve cardiac output, exercise tolerance, and quality of life (QoL). However, patients with end‐stage HF eligible or listed for heart transplantations (HTx) represent a special cohort, because these patients have been excluded from all major trials over the recent years, 6 , 7 leaving them without recommendations and without evidence for optimal treatment strategies for both AF and HF management. In addition, current major trials explicitly exclude patients eligible or listed for HTx, which not only leaves application of the established HF guideline uncertain in this group, 8 but also withholds many of the novel advances in HF therapy in this advanced diseased cohort. Today, it remains unclear whether recent beneficial achievements from CASTLE‐AF, 1 CABANA, 2 and CAMERA‐MRI 3 are transferable and applicable in this rarely investigated patient cohort. Therefore, the purpose of the Catheter Ablation for atrial fibrillation in patientS with end‐sTage heart faiLure and Eligible for Heart Transplantation (CASTLE‐HTx; NCT 04649801) trial is to test the hypothesis that AF ablation has beneficial effects on mortality and morbidity during the ‘waiting time’ for HTx eligibility or to prolong the time span until necessity for implantation of a ventricular assist device. 9
Methods
This is a prospective, randomized, controlled clinical trial. The study will be conducted in an open‐label design. Data collection and management will be carried out locally at our site (Herz‐ und Diabeteszentrum NRW, Bad Oeynhausen, Germany). All serious adverse events will be reported and classified. This study has been approved by our institutional review board (Ref. 2020‐678) and is in line with the Declaration of Helsinki.
Objective
The primary objective of the CASTLE‐HTx study is to evaluate the effects of catheter‐based ablation of AF in patients eligible for HTx on the composite endpoint of ‘all‐cause mortality, transplantation, or implantation of a ventricular assist device’.
Primary endpoint
The primary endpoint is the composite of all‐cause mortality, worsening of HF requiring a high urgent transplantation, or implantation of a ventricular assist device (as bridge to transplantation therapy).
Secondary endpoints
The secondary study endpoints are all‐cause mortality, cardiovascular mortality, cerebrovascular accidents, AF burden reduction, worsening of HF requiring unplanned hospitalization, unplanned hospitalization due to cardiovascular reason, all‐cause hospitalization, QoL, number of delivered implantable cardioverter defibrillator (ICD) therapies (shock and ATP), time to first ICD therapy, number of device‐detected ventricular tachycardia/ventricular fibrillation episodes, AF burden, AF‐free interval, left ventricular (LV) function, exercise tolerance, and percentage of right ventricular (RV) pacing.
Screening and enrolment
All patients with a history of AF (paroxysmal or persistent) and end‐stage HF who present for evaluation for HTx at our institution fulfilling current International Society for Heart and Lung Transplantation (ISHLT) HTx listing criteria 7 will be screened for eligibility of enrolment into this trial (Table 1 ). For the purpose of this study, the following definitions will be used: paroxysmal AF is defined as AF that terminates spontaneously or with intervention within 7 days of onset. Persistent AF is defined as AF that is continuously sustained beyond 7 days, including episodes terminated by cardioversion (drugs or electrical cardioversion) after ≥7 days. Included within the category of persistent AF is ‘longstanding persistent AF’, which is defined as continuous AF of >1 year duration. 10 Documentation of AF can be obtained by electrocardiogram, Holter, loop recorder, ICD memory, or any other suitable device. Previous antiarrhythmic drug therapy is not an exclusion criterion. The novel European Society of Cardiology guidelines for the management of patients with AF provides a IIa recommendation for AF ablation in patients with HF. 10
Table 1.
Inclusion and exclusion criteria
| Inclusion criteria |
| (1) Symptomatic paroxysmal or persistent AF (paroxysmal: ≥2 symptomatic or one documented AF episode lasting 30 s or more in the last 3 months; persistent: ≥1 documented episode in the last 3 months) |
| (2) Eligible for heart transplantation due to end‐stage heart failure |
| (3) LV dysfunction with left ventricular ejection fraction ≤35% (measured in the last 6 weeks prior to enrolment) |
| (4) NYHA class ≥II |
| (5) Indication for ICD therapy due to primary prevention |
| (6) Dual‐chamber ICD with home monitoring capabilities already implanted |
| (7) The patient is willing and able to comply with the protocol and has provided written informed consent |
| (8) Sufficient GPRS network coverage in the patient's area |
| (9) Age ≥18 years |
| Exclusion criteria |
| (1) Documented left atrial diameter >6 cm (parasternal long‐axis view) |
| (2) Contraindication for chronic anticoagulation therapy or heparin |
| (3) Previous left heart ablation procedure for atrial fibrillation |
| (4) Acute coronary syndrome, cardiac surgery, angioplasty, or cerebrovascular accident within 2 months prior to enrolment |
| (5) Untreated hypothyroidism or hyperthyroidism |
| (6) Enrolment in another investigational drug or device study |
| (7) Woman currently pregnant, breastfeeding, or not using reliable contraceptive measures during fertility age |
| (8) Mental or physical inability to participate in the study |
| (9) Listed as ‘high urgent’ for heart transplantation |
| (10) Cardiac assist device implanted |
| (11) Planned cardiovascular intervention |
| (12) Life expectancy ≤12 months |
| (13) Uncontrolled hypertension |
| (14) Requirement for dialysis due to end‐stage renal failure |
AF, atrial fibrillation; GPRS, General Packet Radio Service; ICD, implantable cardioverter defibrillator; LV, left ventricular; NYHA, New York Heart Association.
Study conduct
Following verification of the inclusion and exclusion criteria and documentation of the demographic data and medical history, the investigational site will plan the date for enrolment and baseline testing within the next 4 weeks. In case of randomization to the ablation arm, the investigational site will also plan the date of the ablation procedure, which will be performed as soon as possible after baseline evaluation. Figure 1 illustrates the study flow chart. A composite endpoint has been chosen for the single‐centre design of this study and for the significantly higher number of patients required to specifically investigate mortality.
Figure 1.
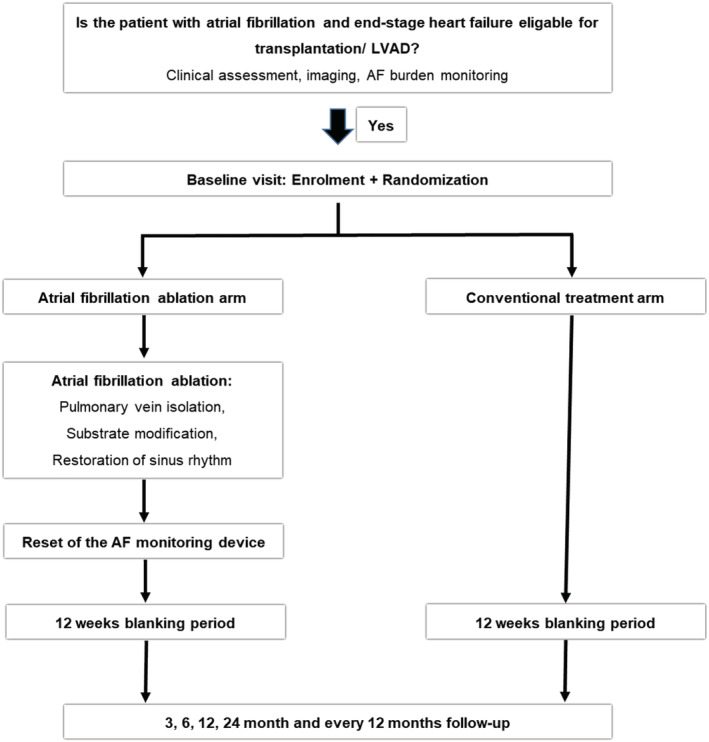
Study conduct—flow chart. AF, atrial fibrillation; LVAD, left ventricular assist device.
Baseline testing
At baseline testing, exclusion criteria (Table 1 ) will be re‐evaluated with presence of current ISHLT HTx listing criteria (Table 2 ). 7 If exclusion criteria are not met, the patient will be enrolled after providing written informed consent and baseline evaluation will be performed. Echocardiographic measurements will be performed in agreement with the institutional standard operating procedures; the following parameters will be assessed: right and left atrial diameter, RV/LV fractional shortening, RV/LV ejection fraction, RV/LV end‐systolic diameter, RV/LV end‐diastolic diameter and volumes, and RV/LV strain analysis. Each patient will perform a 6 min walk test. ICD/CRT‐D data will be recorded and stored, followed by memory reset at the end of the session.
Table 2.
Indications for listing for heart transplantation in accordance with ISHLT 2016 criteria 7
| Cardiopulmonary stress testing to guide transplant listing: a maximal cardiopulmonary exercise test is defined as one with a respiratory exchange ratio (RER) of 1.05 and achievement of an anaerobic threshold on optimal pharmacological therapy (Class I, level of evidence: B) |
| In patients intolerant of a beta‐blocker, a cut‐off for peak oxygen consumption (VO2) of 14 mL/kg/min should be used to guide listing (Class I, level of evidence: B) |
| In the presence of a beta‐blocker, a cut‐off for peak VO2 of 12 mL/kg/min should be used to guide listing (Class I, level of evidence: B) |
| In young patients (<50 years) and women, it is reasonable to consider using alternate standards in conjunction with peak VO2 to guide listing, including per cent of predicted (50%) peak VO2 (Class IIa, level of evidence: B) |
| In the presence of a sub‐maximal cardiopulmonary exercise test (RER 1.05), use of ventilation equivalent of carbon dioxide (VE/VCO2) slope of >35 as a determinant in listing for transplantation may be considered (Class IIb, level of evidence: C) |
| In obese [body mass index (BMI) >30 kg/m2] patients, adjusting peak VO2 to lean body mass may be considered. A lean body mass‐adjusted peak VO2 of 19 mL/kg/min can serve as an optimal threshold to guide prognosis (Class IIb, level of evidence: B) |
| Listing patients based solely on the criterion of a peak VO2 measurement should not be performed (Class III, level of evidence: C) |
| Use of heart failure prognosis scores: heart failure prognosis scores should be performed along with cardiopulmonary exercise test to determine prognosis and guide listing for transplantation for ambulatory patients. An estimated 1 year survival as calculated by the Seattle Heart Failure Model (SHFM) of 80% or a Heart Failure Survival Score (HFSS) in the high/medium‐risk range should be considered as reasonable cut points for listing (Class IIb, level of evidence: C) |
| Listing patients solely on the criteria of heart failure survival prognostic scores should not be performed (Class III, level of evidence: C) |
| Role of diagnostic right heart catheterization (RHC): RHC should be performed on all adult candidates in preparation for listing for cardiac transplantation and periodically until transplantation (Class 1, level of evidence: C). Periodic RHC is not advocated for routine surveillance in children (Class III, level of evidence: C) |
| RHC should be performed at 3 to 6 month intervals in listed patients, especially in the presence of reversible pulmonary hypertension or worsening of heart failure symptoms (Class I, level of evidence: C) |
| A vasodilator challenge should be administered when the pulmonary artery systolic pressure is >50 mmHg and either the transpulmonary gradient is >15 or the pulmonary vascular resistance (PVR) is >3 Wood units while maintaining a systolic arterial blood pressure >85 mmHg (Class I, level of evidence: C) |
| When an acute vasodilator challenge is unsuccessful, hospitalization with continuous haemodynamic monitoring should be performed, as often the PVR will decline after 24 to 48 h of treatment consisting of diuretics, inotropes, and vasoactive agents such as inhaled nitric oxide (Class I, level of evidence: C) |
| If medical therapy fails to achieve acceptable haemodynamics and if the left ventricle cannot be effectively unloaded with mechanical adjuncts, including an intra‐aortic balloon pump (IABP) and/or left ventricular assist device (LVAD), it is reasonable to conclude that the pulmonary hypertension is irreversible. After LVAD, re‐evaluation of haemodynamics should be performed after 3 to 6 months to ascertain reversibility of pulmonary hypertension (Class IIA, level of evidence: C) |
| Carefully selected patients 4–70 years of age may be considered for cardiac transplantation (Class IIb, level of evidence: C) |
| Pre‐transplant body mass index (BMI) >35 kg/m2 is associated with a worse outcome after cardiac transplantation. For such obese patients, it is reasonable to recommend weight loss to achieve a BMI of <35 kg/m2 before listing for cardiac transplantation (Class IIa, level of evidence: C) |
| Pre‐existing neoplasms are diverse, and many are treatable with excision, radiotherapy, or chemotherapy to induce cure or remission. In these patients needing cardiac transplantation, collaboration with oncology specialists should occur to stratify each patient as to their risk of tumour recurrence. Cardiac transplantation should be considered when tumour recurrence is low based on tumour type, response to therapy, and negative metastatic work‐up. The specific amount of time to wait to transplant after neoplasm remission will depend on the aforementioned factors, and no arbitrary time period for observation should be used (Class I, level of evidence: C) |
| Diabetes with end‐organ damage (other than non‐proliferative retinopathy) or persistent poor glycaemic control [glycosylated haemoglobin (HbA1c) >7.5% or 58 mmol/mol] despite optimal effort is a relative contraindication for transplant (Class IIa, level of evidence: C) |
| Renal function should be assessed using estimated glomerular filtration rate (eGFR) or creatinine clearance under optimal medical therapy. Evidence of abnormal renal function should prompt further investigation, including renal ultrasonography, estimation of proteinuria, and evaluation for renal arterial disease, to exclude intrinsic renal disease. It is reasonable to consider the presence of irreversible renal dysfunction (eGFR <30 mL/min/1.73 m2) as a relative contraindication for heart transplantation alone (Class IIa, level of evidence: C) |
| Clinically severe symptomatic cerebrovascular disease may be considered a contraindication to transplantation. Peripheral vascular disease may be considered a relative contraindication for transplantation when its presence limits rehabilitation and revascularization is not a viable option (Class IIb, level of evidence: C) |
| Assessment of frailty (3 of 5 possible symptoms, including unintentional weight loss of >10 lbs within the past year, muscle loss, fatigue, slow walking speed, and low levels of physical activity) could be considered when assessing candidacy (Class IIb, level of evidence: C) |
| Use of mechanical circulatory support should be considered for patients with potentially reversible or treatable co‐morbidities, such as cancer, obesity, renal failure, tobacco use, and pharmacologically irreversible pulmonary hypertension, with subsequent re‐evaluation to establish candidacy (Class IIb, level of evidence: C) |
| Tobacco use: education on the importance of tobacco cessation and reduction in environmental or second‐hand exposure should be performed before the transplant and continue throughout the pre‐transplant and post‐transplant periods (Class I, level of evidence: C) |
| It is reasonable to consider active tobacco smoking as a relative contraindication to transplantation. Active tobacco smoking during the previous 6 months is a risk factor for poor outcomes after transplantation (Class IIa, level of evidence: C) |
| A structured rehabilitative programme may be considered for patients with a recent (24 month) history of alcohol abuse if transplantation is being considered (Class IIb, level of evidence: C) |
| Patients who remain active substance abusers (including alcohol) should not receive heart transplantation (Class III, level of evidence: C) |
| Psychosocial assessment should be performed before listing for transplantation. Evaluation should include an assessment of the patient's ability to give informed consent and comply with instruction, including drug therapy, as well as assessment of the support systems in place at home or in the community (Class I, level of evidence: C) |
| Any patient for whom social supports are deemed insufficient to achieve compliant care in the outpatient setting may be regarded as having a relative contraindication to transplant. The benefit of heart transplantation in patients with severe cognitive–behavioural disabilities or dementia (e.g. self‐injurious behaviour and inability to ever understand and cooperate with medical care) has not been established and has the potential for harm, and therefore, heart transplantation cannot be recommended for this subgroup of patients (Class IIa, level of evidence: C) |
| Poor compliance with drug regimens is a risk factor for graft rejection and mortality. Patients who have demonstrated an inability to comply with drug therapy on multiple occasions should not receive transplantation (Class III, level of evidence: C) |
| Listed patients in an outpatient, ambulatory, non‐inotropic therapy‐dependent state should be continually evaluated for maximal pharmacological and device therapy, including implantable cardioverter defibrillator (ICD) or biventricular pacing, when appropriate. Such patients must be re‐evaluated at 3 to 6 month intervals with cardiopulmonary exercise testing and heart failure survival prognostic scores to assess their response to therapy and, if they have improved significantly, should be considered for delisting (Class I, level of evidence: C) |
| Higher prioritization for highly sensitized patients may be considered due to difficulty obtaining a donor, causing excessive waiting times and an increase in waiting list mortality (Class IIb, level of evidence: C) |
| Retransplantation is indicated for those patients who develop significant CAV with refractory cardiac allograft dysfunction, without evidence of ongoing rejection (Class IIa, level of evidence: C) |
CAV, cardiac allograft vasculopathy.
Ablation procedure
Subjects will undergo ablation as soon as possible after baseline evaluation. Before ablation, presence of left atrial thrombus formation has to be ruled out. In case of presence of thrombi, the procedure will be postponed until thrombi will be dissolved, but not longer than 4 weeks. If, after that period, thrombi are still present, the ablation will be performed using a cerebral protection device.
The aim of AF ablation is to achieve isolation of all four pulmonary veins (PVs) and to restore sinus rhythm. The anticoagulation regimen will be prescribed as follows: AF ablation will be performed on uninterrupted vitamin K antagonist aiming at a target international normalized ratio of 2.0–3.0. In patients on direct oral anticoagulants, anticoagulation will be stopped 12–24 h before the procedure and reinitiated 4 h after ablation (after testing for pericardial effusion). A total of 3 months after successful ablation and in the absence of any recurrence of AF, antiarrhythmic drugs should be discontinued. Rare short‐lasting episodes (<30 s) recorded in the early post‐blanking period will be considered as insignificant. A spiral computed tomography scan can be indicated to evaluate the presence of PV stenosis after catheter ablation. The ablation system (three‐dimensional mapping and radiofrequency‐guided or cryoballoon‐guided ablation) selection is left to the discretion of the investigator, but the investigator must have performed at least 50 AF ablation procedures, comprising PV isolation, with the same approach. The ablation will be classified as acutely successful if (i) all four PVs are isolated and (ii) sinus rhythm is restored (if not already present). Isolation of the PVs will be proven by identifying the presence or absence of local PV potentials in the vein during sinus rhythm or pacing, typically from the distal coronary sinus, at a slow rate (vein entry). Isolations will be documented by short strips of PV intracardiac electrograms. Sinus rhythm can be restored also by means of electrical cardioversion. If required, any additional lesion in the left as well as in the right atrium, including coronary sinus, superior vena cava, and inferior vena cava, is permitted. A ‘PVI‐only ablation’ approach vs. ‘PVI + additional ablation’ will be subject of a subgroup analysis. In case of unsuccessful ablation, a second attempt will be made within 3 months. If after the second attempt the outcome is also failure, atrioventricular node ablation will be performed. Any time during the course of the study, additional ablations may be performed if the subject has recurrence(s) of AF except during the 12 weeks of blanking period following either the initial ablation or a chronic redo.
Conventional treatment
Subjects assigned to the conventional arm will be treated according to the European Society of Cardiology 2016 guideline for management of chronic heart failure in the adults 8 and the European Society of Cardiology 2020 guidelines for management of patients with atrial fibrillation. 10 Efforts to maintain sinus rhythm in this study arm are recommended. In case of rate control strategy, although no standard method for assessment of heart rate control has been established, criteria for rate control vary with patient age but usually involve achieving ventricular rates between 60 and 80 b.p.m. at rest and between 90 and 115 b.p.m. during moderate exercise. Anticoagulation will be initiated, if not already started, and maintained throughout the study.
Follow‐up
If available, home monitoring will be activated in the implanted ICD/CRT device or implantable cardiac monitor for continuous measurements of the AF burden on a daily basis. The investigator will promptly be informed in case of recurrence of AF. In case that home monitoring is not possible, the mean AF burden data will be collected from the interrogation of the implantable defibrillators at each visit. In case of recurrences outside the post‐ablation blanking period, it is recommended to perform additional ablation(s), unless clinically contraindicated. Antiarrhythmic drug therapy for rhythm control will also be allowed in case of AF recurrence after ablation. At 3, 6, 12, 24, and 36 months after baseline, all patients will undergo a regular follow‐up (FU) visit. Patients completing the multiples of 12 months while the study is still ongoing will have additional FU visits, which will be equal to all the other planned visits. FU windows will be ±14 days for the 3 and 6 month visits and ±30 days for the remaining others. Echocardiographic measurements will be performed as described previously. After the end of the study, the patients may be contacted by phone to assess their vital status.
Moreover, patients are routinely followed for their HTx listing criteria and status, 7 and re‐evaluation of HF therapy will be adjusted in the course of follow‐up. 11 In addition to that these patients are routinely re‐evaluated for severity of HF, symptoms and secondary organ dysfunction and indication for implantation of ventricular assist devices are regularly reassessed at every patient visit. 12 , 13
Quality of life questionnaires and symptom diary
Prior to the FU examinations, each patient will be asked to complete a QoL questionnaire (Minnesota Living with Heart Failure ), at baseline and at all planned FU visits. The Minnesota Living with Heart Failure Questionnaire is a well‐validated and highly disease‐specific measurement tool. 14 A symptom diary will be used to assess the relationship between recurrences of AF and symptoms. At enrolment, every patient receives a diary to record typical HF and AF symptoms, such as chest pain, dizziness, breathlessness, swollen feet or ankles, fatigue or weakness, nausea, palpitations, sleep disorders, and racing heart. Furthermore, visits to a general practitioner and to a hospital will also be recorded. On the day of the symptomatic episode, the patient is asked to document the type and severity of symptom(s) and to state if there was contact to the general practitioner and/or a hospital visit. The patient is asked to bring the diary at every planned FU visits, which will be examined by the investigator to detect any unreported adverse events and/or hospitalizations.
Statistical methodology
Analysis
Primary analyses
Descriptive statistics will be reported for all clinical and demographic parameters. The main analysis will be based on the intention‐to‐treat population, defined based on the intention‐to‐treat principle. The aim of this study is to demonstrate that ablated patients have a lower risk for the composite endpoint consisting of all‐cause mortality, worsening of HF, and the requirement for implantation of a ventricular assist device. Therefore, we will perform a log‐rank test with a one‐sided significance level of 2.5%. Furthermore, we will conduct a Cox proportional hazard regression analysis focusing on treatment groups including all clinical parameters as covariates to adjust for confounding. Anyone involved in data analysis is blinded from the randomization result.
Secondary analyses
Secondary endpoints will be analysed with appropriate statistical methods depending on scales, including ranking methods for the evaluation of ordinal data. All P‐values and confidence intervals from sensitivity or secondary analyses as well as from subgroup analyses will be regarded as non‐confirmatory and exploratory analyses. Missing values will be—if appropriate—imputed using multiple imputation strategies. All analyses will be performed using validated statistical software.
Interims analysis to report on safety issues such as periprocedural stroke and bleeding are implemented.
Sample size calculation
A hazard ratio (HR) of 0.75 is considered as clinically relevant comparing the ablated patients with the conventional treatment arm. However, it is expected that the HR is 0.5. A log‐rank test detected an HR of 0.5 at one‐sided 2.5% significance level with 80% of power, an accrual time of 12 months, a follow‐up time of 36 months, and an assumed drop‐out rate of 15% in both groups, when the sample size is 97 per treatment arm. In total, 194 patients are required for this prospective randomized analysis. The sample size calculation was computed using the statistical software R Version 3.6.1. We expect low drop‐out rates for the high psychological strain in this advanced diseased patient cohort.
Definition and detection of recurrence of atrial fibrillation
For the purposes of this study, any sustained episode of AF lasting 30 s or more is classified as recurrence. The investigator, or a nominated person at the institution, will obtain all the details of the episode, including the duration. All episodes lasting 30 s or more occurring outside the blanking period of 12 weeks will be reported to the investigator, who will decide whether to plan a redo ablation or not. Recurrences within the blanking period will be named ‘early recurrences’; they will be collected but will not trigger any action.
Definition and detection of burden of atrial fibrillation
Multiple episodes of AF, all lasting <30 s, will not be classified as a recurrence. However, such episodes may have a clinically significant impact requiring intervention. The sum of the durations of all such episodes (eventually also comprising episodes that could have been longer than 30 s) within the day, expressed as a percentage with respect to 24 h, is defined as AF burden.
Translational tissue analysis from bench to bedside—and back
Ventricular myocardial tissue will be obtained from patients who will undergo LV assist device (LVAD) implantation or HTx. In all tissue specimens, myocardial contractility experiments will be conducted to assess the effect of catheter ablation on multicellular human HF myocardium in comparison with specimen from non‐ablated patients. We will perform contractility experiments using in toto‐isolated isometrically twitching ventricular trabeculae from human hearts explanted from patients with end‐stage HF. 15 , 16 In addition, intracellular Ca2+ imaging and action potential recordings using the patch‐clamp technique will be performed as described previously by our group. 16 , 17 , 18 , 19 Moreover, to investigate the effect of AF on myocardial function ex vivo, we will apply an AF‐like arrhythmic but normofrequent electrical stimulation of cultured isolated cardiomyocytes and muscle strips. All previously mentioned techniques will be used to characterize the contractile and electrical phenotype after 24 h of arrhythmic field stimulation. Translational experiments will be conducted at Regensburg University Medical Center.
Discussion
Catheter ablation has been demonstrated to be superior over antiarrhythmic drug therapy for both restoration and maintenance of sinus rhythm. 1 In the CASTLE‐AF trial, catheter ablation demonstrated superiority over pharmacological management in patients with AF and HF. 1 However, end‐stage HF differs from other stages of the condition due to a worse prognosis, often related to structural LV remodelling and low cardiac output. In patients with end‐stage HF, transplantation and LVAD implantation prolong patients' life and improve its quality. 9 , 13 The individual decision pathway focusing on eligibility for HTx as well as LVAD implantation starts with confirmation of end‐stage HF, continues with ruling out contraindications, and finally ends with selecting the right path in terms of individualized therapy.
More and more evidence has accumulated demonstrating that patients with HF and AF benefit, in terms of hard endpoints, from invasive rhythm control by catheter ablation. 1 , 2 , 3 These observations led to the suggestion that there might be a substantial degree of AF‐induced structural LV remodelling in HF patients and even in those without LV dysfunction. In this context, recent data demonstrated that sinus rhythm after successful AF ablation resulted in reverse LV remodelling and improvement of the LV function as well as HF symptoms. 1 , 20 , 21 , 22 Irrespective of these findings, open questions remain regarding selection of adequate patients and validity of the findings in patients with terminal HF and severely impaired LV function. As mentioned earlier, patients with end‐stage HF eligible or listed for HTx represent a separate and highly specialized cohort, as these patients have been excluded from all major and guideline relevant clinical trials. 6 , 7 Consequently, these patients suffer from a lack of recommendations and evidence for optimal treatment strategies for both AF and HF management.
In addition to that not only patient selection but also patient re‐evaluation remains challenging, 23 because HF patients may have presented to a centre and evaluation at presentation came to the conclusion that it was too early for either LVAD implantation or listing for HTx. 7 , 11 Patients with end‐stage HF can often rapidly deteriorate in their symptoms and experience acute worsening of their condition resulting in an urgent need for LVAD implantation due to haemodynamic instability. 9 , 13 In context with the difficulties in identifying patients that are at risk for frequent deterioration, AF and tachycardia‐induced cardiomyopathy may contribute to rapid haemodynamic decline. Therefore, this trial is designed to address AF as a risk factor of HF deterioration.
Importantly, we would like to emphasize that patient participation in this trial does not imply any therapy withholding on therapeutic attempts that patients would receive for their HF therapy otherwise. This trial is designed to fill the current scientific gap on patients that are eligible for HTx but stable enough to require immediate intervention. No patient in this trial will be penalized from listing for HTx or gaining immediate HTx through incorporation of AF ablation, which would not be ethically justifiable either. All patients will receive current optimal and guideline‐derived medical and device therapy for their individual HF status, 8 but for those ‘in between’, this trial has been designed to provide data on influence of AF ablation resulting in rhythm control in patients with elevated stages of HF.
The CASTLE‐HTx trial is a prospective open‐label randomized trial to evaluate the clinical and cellular effects of catheter‐based ablation of AF in patients eligible for HTx for the composite endpoint of all‐cause mortality, transplantation, or implantation of a ventricular assist device as well as a significant AF burden reduction. Patient enrolment will start in January 2021 and is expected to end in December 2022. The outcome of the trial should define the value of AF ablation in patients suffering from AF and end‐stage HF.
Conflict of interest
None declared.
Funding
We acknowledge the support by the DFG Open Access Publication Funds of the Ruhr‐Universität Bochum.
Acknowledgement
Open access funding enabled and organized by Projekt DEAL.
Sohns, C. , Marrouche, N. F. , Costard‐Jäckle, A. , Sossalla, S. , Bergau, L. , Schramm, R. , Fuchs, U. , Omran, H. , Rubarth, K. , Dumitrescu, D. , Konietschke, F. , Rudolph, V. , Gummert, J. , Sommer, P. , and Fox, H. (2021) Catheter ablation for atrial fibrillation in patients with end‐stage heart failure and eligibility for heart transplantation. ESC Heart Failure, 8: 1666–1674. 10.1002/ehf2.13150.
References
- 1. Marrouche NF, Brachmann J, Andresen D, Siebels J, Boersma L, Jordaens L, Merkely B, Pokushalov E, Sanders P, Proff J, Schunkert H, Christ H, Vogt J, Bansch D, Investigators C‐A. Catheter ablation for atrial fibrillation with heart failure. N Engl J Med 2018; 378: 417–427. [DOI] [PubMed] [Google Scholar]
- 2. Packer DL, Mark DB, Robb RA, Monahan KH, Bahnson TD, Poole JE, Noseworthy PA, Rosenberg YD, Jeffries N, Mitchell LB, Flaker GC, Pokushalov E, Romanov A, Bunch TJ, Noelker G, Ardashev A, Revishvili A, Wilber DJ, Cappato R, Kuck KH, Hindricks G, Davies DW, Kowey PR, Naccarelli GV, Reiffel JA, Piccini JP, Silverstein AP, Al‐Khalidi HR, Lee KL, Investigators C. Effect of catheter ablation vs antiarrhythmic drug therapy on mortality, stroke, bleeding, and cardiac arrest among patients with atrial fibrillation: the CABANA randomized clinical trial. JAMA 2019; 321: 1261–1274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Prabhu S, Taylor AJ, Costello BT, Kaye DM, McLellan AJA, Voskoboinik A, Sugumar H, Lockwood SM, Stokes MB, Pathik B, Nalliah CJ, Wong GR, Azzopardi SM, Gutman SJ, Lee G, Layland J, Mariani JA, Ling LH, Kalman JM, Kistler PM. Catheter ablation versus medical rate control in atrial fibrillation and systolic dysfunction: the CAMERA‐MRI study. J Am Coll Cardiol 2017; 70: 1949–1961. [DOI] [PubMed] [Google Scholar]
- 4. Ling LH, Kistler PM, Kalman JM, Schilling RJ, Hunter RJ. Comorbidity of atrial fibrillation and heart failure. Nat Rev Cardiol 2016; 13: 131–147. [DOI] [PubMed] [Google Scholar]
- 5. Feldmann C, Ertl G, Angermann CE. Holistic therapy of chronic heart failure. Internist (Berl) 2014; 55: 676–686. [DOI] [PubMed] [Google Scholar]
- 6. Jessup M, Drazner MH, Book W, Cleveland JC, Jr., Dauber I, Farkas S, Ginwalla M, Katz JN, Kirkwood P, Kittleson MM, Marine JE, Mather P, Morris AA, Polk DM, Sakr A, Schlendorf KH, Vorovich EE. 2017 ACC/AHA/HFSA/ISHLT/ACP advanced training statement on advanced heart failure and transplant cardiology (revision of the ACCF/AHA/ACP/HFSA/ISHLT 2010 clinical competence statement on management of patients with advanced heart failure and cardiac transplant): a report of the ACC Competency Management Committee. J Am Coll Cardiol 2017; 69:2977–3001. [DOI] [PubMed] [Google Scholar]
- 7. Mehra MR, Canter CE, Hannan MM, Semigran MJ, Uber PA, Baran DA, Danziger‐Isakov L, Kirklin JK, Kirk R, Kushwaha SS, Lund LH, Potena L, Ross HJ, Taylor DO, Verschuuren EAM, Zuckermann A, International Society for Heart Lung Transplantation (ISHLT) Infectious Diseases, Pediatric and Heart Failure and Transplantation Councils . The 2016 International Society for Heart Lung Transplantation listing criteria for heart transplantation: a 10‐year update. J Heart Lung Transplant 2016; 35: 1–23. [DOI] [PubMed] [Google Scholar]
- 8. Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JGF, Coats AJS, Falk V, Gonzalez‐Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GMC, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P, Group ESCSD . 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 2016; 37:2129–2200. [DOI] [PubMed] [Google Scholar]
- 9. Gummert JF, Haverich A, Schmitto JD, Potapov E, Schramm R, Falk V. Permanent implantable cardiac support systems. Dtsch Arztebl Int 2019; 116: 843–848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Hindricks G, Potpara T, Dagres N, Arbelo E, Bax JJ, Blomstrom‐Lundqvist C, Boriani G, Castella M, Dan GA, Dilaveris PE, Fauchier L, Filippatos G, Kalman JM, La Meir M, Lane DA, Lebeau JP, Lettino M, Lip GYH, Pinto FJ, Thomas GN, Valgimigli M, Van Gelder IC, Van Putte BP, Watkins CL, Group ESCSD . 2020 ESC guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association of Cardio‐Thoracic Surgery (EACTS). Eur Heart J 2020; ehaa612. [DOI] [PubMed] [Google Scholar]
- 11. Gummert JF. Heart transplantation in Bad Oeynhausen, Germany: the heart transplant program at the Heart and Diabetes Center Bad Oeynhausen, University Hospital, Ruhr—University Bochum University, Germany. Eur Heart J 2017; 38: 3411–3413. [DOI] [PubMed] [Google Scholar]
- 12. Ibrahim M, Arafat S, Rojas SV, Schramm R, Gummert JF, Morshuis M, Fox H. Facilitating heart transplantability in an end‐stage heart failure patient with brain abscess and infected left ventricle assist device—a unique case report. Int J Surg Case Rep 2020; 71: 213–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Schramm R, Zittermann A, Morshuis M, Schoenbrodt M, von Roessing E, von Dossow V, Koster A, Fox H, Hakim‐Meibodi K, Gummert JF. Comparing short‐term outcome after implantation of the HeartWare® HVAD® and the Abbott® HeartMate 3® . ESC Heart Fail 2020; 7: 908–914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Kelkar AA, Spertus J, Pang P, Pierson RF, Cody RJ, Pina IL, Hernandez A, Butler J. Utility of patient‐reported outcome instruments in heart failure. JACC Heart Fail 2016; 4: 165–175. [DOI] [PubMed] [Google Scholar]
- 15. Sossalla S, Wagner S, Rasenack EC, Ruff H, Weber SL, Schondube FA, Tirilomis T, Tenderich G, Hasenfuss G, Belardinelli L, Maier LS. Ranolazine improves diastolic dysfunction in isolated myocardium from failing human hearts—role of late sodium current and intracellular ion accumulation. J Mol Cell Cardiol 2008; 45: 32–43. [DOI] [PubMed] [Google Scholar]
- 16. Sossalla S, Fluschnik N, Schotola H, Ort KR, Neef S, Schulte T, Wittkopper K, Renner A, Schmitto JD, Gummert J, El‐Armouche A, Hasenfuss G, Maier LS. Inhibition of elevated Ca2+/calmodulin‐dependent protein kinase II improves contractility in human failing myocardium. Circ Res 2010; 107: 1150–1161. [DOI] [PubMed] [Google Scholar]
- 17. Fischer TH, Herting J, Tirilomis T, Renner A, Neef S, Toischer K, Ellenberger D, Forster A, Schmitto JD, Gummert J, Schondube FA, Hasenfuss G, Maier LS, Sossalla S. Ca2+/calmodulin‐dependent protein kinase II and protein kinase A differentially regulate sarcoplasmic reticulum Ca2+ leak in human cardiac pathology. Circulation 2013; 128: 970–981. [DOI] [PubMed] [Google Scholar]
- 18. Hamdani N, Bishu KG, von Frieling‐Salewsky M, Redfield MM, Linke WA. Deranged myofilament phosphorylation and function in experimental heart failure with preserved ejection fraction. Cardiovasc Res 2013; 97: 464–471. [DOI] [PubMed] [Google Scholar]
- 19. Hamdani N, Krysiak J, Kreusser MM, Neef S, Dos Remedios CG, Maier LS, Kruger M, Backs J, Linke WA. Crucial role for Ca2+/calmodulin‐dependent protein kinase‐II in regulating diastolic stress of normal and failing hearts via titin phosphorylation. Circ Res 2013; 112: 664–674. [DOI] [PubMed] [Google Scholar]
- 20. Kowallick JT, Staab W, Schuster A, Backhaus SJ, Weber‐Kruger M, Bauer L, Sohns C, Lotz J, Hasenfuss G, Luthje L, Zabel M, Bergau L. Reverse left ventricular structural remodeling after catheter ablation of atrial fibrillation in patients with preserved left ventricular function: insights from cardiovascular magnetic resonance native T1 mapping. Heart Rhythm 2019; 16: 424–432. [DOI] [PubMed] [Google Scholar]
- 21. Sugumar H, Prabhu S, Voskoboinik A, Young S, Gutman SJ, Wong GR, Parameswaran R, Nalliah CJ, Lee G, McLellan AJ, Taylor AJ, Ling LH, Kalman JM, Kistler PM. Atrial remodeling following catheter ablation for atrial fibrillation‐mediated cardiomyopathy: long‐term follow‐up of CAMERA‐MRI study. JACC Clin Electrophysiol 2019; 5: 681–688. [DOI] [PubMed] [Google Scholar]
- 22. Sohns C, Zintl K, Zhao Y, Dagher L, Andresen D, Siebels J, Wegscheider K, Sehner S, Boersma L, Merkely B, Pokushalov E, Sanders P, Schunkert H, Bansch D, Mahnkopf C, Brachmann J, Marrouche NF. Impact of left ventricular function and heart failure symptoms on outcomes post ablation of atrial fibrillation in heart failure: CASTLE‐AF trial. Circ Arrhythm Electrophysiol 2020; 13: e008461. [DOI] [PubMed] [Google Scholar]
- 23. Szymczyk T, Sauzet O, Paluszkiewicz LJ, Costard‐Jackle A, Potratz M, Rudolph V, Gummert JF, Fox H. Non‐invasive assessment of central venous pressure in heart failure: a systematic prospective comparison of echocardiography and Swan‐Ganz catheter. Int J Cardiovasc Imaging 2020; 36: 1821–1829. [DOI] [PMC free article] [PubMed] [Google Scholar]


