Abstract
Resilience has conventionally focused on an individual’s ability to overcome adversity. Recent research expands on this definition, making resilience a multi-dimensional construct. Native Hawaiians experience health disparities compared to the general population of Hawai’i. Despite the pressing need to address health disparities, minimal research examines resilience factors that serve as buffers for adverse experiences of Native Hawaiians. The purpose of this study was to estimate psychometric properties of scales that measured resilience-based factors through multiple levels using higher-order confirmatory factor analyses (CFA) and ascertain if this construct of resilience mediated or moderated adversity experienced by a sample of Native Hawaiians. Participants included 125 adults who participated in the Hawaiian Homestead Health Survey. Based on higher-order CFA, resilience comprised internal assets measured by hope, satisfaction with life, and environmental mastery, and external resources measured by social support and Native Hawaiian cultural identity. Results of the structural equation models were consistent with literature focusing on resiliency and health. Findings emphasized the importance of enhancing resilience by considering strengths and resources on the individual, interpersonal, and community levels. Findings also demonstrated the need to address adversity factors directly, with a specific need of addressing socio-economic status factors. According to structural equation models, resilience slightly mediated and moderated the effect of adversity related to socio-economic status. These findings have implications for future research exploring resilience as a mediator or moderator of adversity among Native Hawaiians and emphasize a multi-faceted construct of resilience to promote better health outcomes.
Keywords: models, Native Hawaiian, psychometrics, resilience
Introduction
Native Hawaiians, or Kanaka Maoli, are the Indigenous people of Hawai’i and comprise 23.3% of the popula-tion in Hawai’i.1 Native Hawaiians have the shortest life expectancy and experience considerable health disparities compared to other major ethnic groups and the general population of Hawai’i.2–4 For instance, Native Hawaiians are disproportionately affected by almost every category of medical disease, including chronic health conditions, such as heart disease, can-cer, and diabetes.3 For many conditions, Native Hawaiians experience mortality at a younger age than other major ethnic groups in Hawai’i.5 Despite the pressing need to address health disparities experienced by Native Hawaiians, minimal research takes a strengths-based approach, which examines resilience factors that serve as buffers for adverse experiences of health for Native Hawaiians.
Strengths-based approaches to health promotion research seek to foster a person’s resilience versus simply targeting deficits.5,6 Resilience has been conventionally defined as an individual’s traits and abilities to overcome adversity.7 Recent research on resilience expands on this definition to include indicators on multiple levels, thereby making the concept of resilience multi-dimensional.8–10 For instance, a review published in 200511 identified five psychosocial classifications of resilience factors, including positive emotions, cognitive flexibility, meaning, social support, and active coping. The multi-dimensional concept of resilience aligns with Native Hawaiian conceptualizations of wellbeing that emphasize the importance of maintaining balanced relationships with ‘āina (land, nature, or environment), kānaka (interpersonal relationships), and akua (spirituality).12
While various measures of resilience exist, a large majority of these scales focus on the individual level and a person’s ability to overcome difficulty and recover from a stressful event in life.13,14 One of the most prominent measures of resilience, the Resilience Scale, has been psychometrically tested and validated in numerous populations as a measure of a person’s ability to bounce back from adverse experiences.13,14 However, items from the Resilience Scale primarily measure individual internal assets such as meaningful life (purpose), perseverance, self-reliance, equanimity, and existential aloneness. Similarly, the Brief Resilience Scale (BRS) has been assessed as a unidimensional construct of individual personal characteristics that help a person recover from adversity.15
Extending this, some researchers have examined coping resources as a resilience construct but have focused on social support as the primary coping resource.9 While the bulk of the literature has focused on social support as a primary coping resource, limited research has explored other coping resources that may serve as resilience-enhancing factors. For instance, research focusing on Indigenous Peoples has made strong connections between Indigenous perspectives of resilience and cultural identity as a protective factor.16,17 In alignment with other Indigenous holistic perspectives of health, and based on Native Hawaiian viewpoints of health, an individual maintains lōkahi by achieving balance among the mind, body, spirit, and world. A sense of lōkahi may serve as a protective factor for Native Hawaiians by increasing their sense of physical, spiritual, social, and emotional sense of wellbeing. Therefore, researchers should consider internal assets and external coping resources, including culture and identity, when examining resilience of Indigenous Peoples.16,17
Individuals who experience poverty and a lower level of socio-economic status (SES) are at higher risk of adversity due to reduced finances, poorer living or environmental conditions, and limited access and availability of resources.18,19 Health status is directly related to social determinants of health, i.e., the conditions in which people are born into and live in that influence health outcomes.18,19 Native Hawaiians experience lower SES compared to other major ethnic groups in Hawai’i. According to the U.S. Census Bureau, about 14.4% of Native Hawaiians live below the poverty rate20 compared to 9.6% of the general population of Hawai’i.21 Only 24% have earned a bachelor’s degree or higher, compared to 31% of the general population.21
Perceived discrimination is another source of adversity for Native Hawaiians. Previous research that has examined the effects of discrimination on health outcomes for Native Hawaiians has found a positive association between perceived overt discrimination and obesity in Native Hawaiians22 as well as perceived discrimination and symptoms of depression. 23 Other studies have found positive associations between experiences of discrimination and hypertension24 and hypocortisolism25 among Native Hawaiians. Another recent study found that cultural affiliation moderated the relationship between perceived discrimination and hypertension, such that for individuals with lower Hawaiian cultural affiliation, frequent perceived discrimination was significantly associated with lower odds of having hypertension.26
While differences exist in Indigenous cultures and experiences, Indigenous Peoples have experienced long-standing cultural or historical trauma, which also serves as a unique adversity to Indigenous Peoples27 including Native Hawaiians. Historical trauma may particularly have profound impacts on Indigenous people as a result of colonization, which occurs when outsiders dominate societies and alienate Indigenous people from their traditional ways of life. Despite these adversities, Native Hawaiians and Indigenous peoples continue to thrive and exhibit resilience.
According to existing models, resilience may operate to counteract adversity through two primary models: the protective model (mediation model) and the compensatory model (moderation model) of resilience.28,29 In the mediation model, resilience factors help an individual mediate the experience of adversity by serving as an intervening or intermediary variable of adversity, therefore lessening the negative impact of the adversity. In the moderation model, resilience factors play an important role in helping an individual by interacting with adversity variables. In this model, the protective factors interact with risks and moderate the negative impacts of adversity, therefore neutralizing the outcome.
The purpose of this study was two-fold. First, this study aimed to determine the psychometric properties of scales that measure internal assets and external resources available to an individual on multiple levels (i.e., individual, interpersonal, and community), which in turn, may facilitate resilience.9 Because psychometrically valid tools were available to measure individual internal assets, social support, and Native Hawaiian cultural identity, confirmatory factor analyses were used to confirm the anticipated overall construct of resilience based on preexisting measures that independently measure individual internal assets and coping resources of resilience in a Native Hawaiian population. Second, this study aimed to investigate whether resilience (as defined by individual internal assets and external coping resources) mediated or moderated adversity (SES and discrimination) among Native Hawaiians living on Hawaiian Homestead Lands, leading to positive self-rated health (based on the Short Form Health Surveys-12 Item version composite score), after controlling for the number of selected health conditions.
Methods
Sample description
In 1921, the US Congress set aside 200,000 acres of government-sponsored homestead lands for the “rehabilitation” of Native Hawaiians.30 Native Hawaiians with at least 50% Hawaiian blood quantum are eligible to join a waitlist lottery for a 99-year lease for a plot of land.31 Surveys from this study were administered in 2015 as a pilot to the overall Hawaiian Homestead Health Survey initiative. The comprehensive survey was developed in response to Native Hawaiian Homestead communities expressing an interest in better understanding health and health-related factors. Pilot data were based on a convenient sample on O’ahu that is more urban compared with other Hawaiian Homestead communities, which tend to be rural or on other islands.
Using community-based participatory research approaches, the survey was developed and mailed to 390 lessees of the partner Hawaiian Homestead Community mailing list. One survey was provided to each household. While the respondents are representative of those residing in this urban, O’ahu Hawaiian Homestead community, each Homestead community has unique characteristics, identity, and connectedness. Of the 390 households invited to participate, 125 adults from different households participated (participation rate of 31.6%). Respondents were 18 years of age or older. A participant who did not identify as Hawaiian was removed from the database, for a final sample size of 124 adults. Participants were predominantly female (70.8, n = 85) with an average age of 58.5 the years (SD = 14.17, range 24–95). About had 43% of the sample was currently married, 40% had a high school diploma, and 52% had an annual household income under $50,000 (See Table 1).
Table 1.
Participants’ Characteristics (N = 124).
| Characteristics | Mean (SD) or N, % |
|---|---|
| Age (years) | 58.5 (14.2) |
| Female (vs. male) | 85/120 (70.8%) |
| Marital Status | |
| Currently single (not married) | 40/122 (32.8%) |
| Currently married | 52/122 (42.6%) |
| Divorced/separated/widowed | 30/122 (24.6%) |
| Adversity | |
| Educational attainment | |
| No high school diploma | 2 (1.6%) |
| High school graduate/ General Education Development | 49 (39.8%) |
| Some college/technical school | 44 (35.8%) |
| College graduate | 28 (22.8%) |
| Income | |
| 0-less than $25,000 | 22 (20.4%) |
| $25,000 to less than $50,000 | 35 (32.4%) |
| $50,000 to less than $75,000 | 10 (9.3%) |
| $75,000 or more | 41 (38.0%) |
| Perceived Discrimination | 12.6 (6.52) |
| Ad-hoc Resilience Enhancement Construct | |
| Internal Assets | |
| Internal Assets Hope | 4.58 (1.06) |
| Satisfaction With life | 5.29 (1.44) |
| Environmental Mastery | 4.26 (0.91) |
| Coping Resources | |
| Social Support | 3.93 (1.05) |
| Native Hawaiian Cultural Identity | 3.90 (0.76) |
| Number of Health Conditions | 0.35 (0.21) |
| Short Form Health Survey-12 item version | |
| Total Composite Score | 63.99 (16.54) |
Measures
Resilience
The construct of resilience for this study, termed the Ad-hoc Resilience Enhancing Construct (AREC), consisted of two components: 1) individual internal assets and 2) external coping resources including social support and cultural identity.
Three scales measured individual internal assets, including: 1) the Hope Scale, 2) the Satisfaction with Life Scale (SWLS), and 3) the Environmental Mastery Scale (EMS). The Hope Scale measured a person’s ability to create and persevere toward their goals, and thus, measured hopefulness.31 This assessment consisted of 6 items ranging on a Likert scale from one (none of the time) to six (all of the time), with a total score ranging from 6 to 36. The items have been acknowledged as two sub-scales: agency, which measured a person’s ability to initiate and create goals and pathways, which measured a person’s perceived ability to reach these goals. An item from the agency subscale was “I think I am doing pretty well” and an item from the hope subscale was “I can think of many ways to get the things in life that are most important to me”. While the original version of this survey was created with the intent of measuring hope with children, the Hope Scale has also been adapted and administered to adults. The original Hope Survey was selected for the adult homestead population to ensure user-friendliness and decrease participant fatigue. Other research with Indigenous communities has also incorporated the original Hope Scale in comprehensive community-based surveys.32 The Hope Scale has demonstrated good internal consistency with Cronbach alphas ranging from .72 to .86 with a median of .77.31
The Satisfaction with Life Scale (SWLS) measured a person’s global satisfaction with life based on their perceived quality of life and perceived ideal life.33 This survey consisted of 5 items rated on a Likert scale ranging from 1 to 7 (strongly disagree to strongly agree). Higher scores on the SWLS indicated greater satisfaction with life, and thus, increased psychological wellbeing.34–36 An example item included: “In most ways, my life is close to my ideal.” The SWLS has demonstrated high internal reliability with Cronbach alphas ranging from .79 to .89.33
The Environmental Mastery Scale (EMS) was a four-item scale that measured competence in managing everyday life based on one’s environment. For the purpose of the Hawaiian Homestead Health Survey, the original EMS was adapted from a 5-point Likert scale (completely disagree to completely agree) to a 7-point Likert scale (strongly disagree to strongly agree). Research and community partners provided the SWLS and EMS on the same Likert scale to minimize confusion and decrease participant fatigue of the overall Homestead Health Survey. Two of the four items were negatively worded, and therefore, these items were reverse-scored such that higher scores indicated higher levels of self-efficacy and environmental mastery.35,36 A sample item from the EMS included: “I have been able to build a home and a lifestyle for myself that is much to my liking”. The EMS has demonstrated high internal consistency with a coefficient of .86 and a test-retest reliability coefficient of .81.35,36
Two scales measured external coping resources, including: 1) the modified, shortened version of the Medical Outcomes Study, Social Support Scale (mMOS-SSS) and 2) the Native Hawaiian Cultural Identity Scale (NHCIS).
Social support was measured by the 8-item modified version of the Medical Outcomes Study, Social Support Scale (mMOS-SSS).37,38 The mMOS-SSS measured two forms of social support: emotional social support and instrumental social support. An example of an instrumental social support item was “Someone to help you if you were confined to bed,” while an example of an emotional social support item was “Someone to have a good time with”. Each subscale consisted of four items, scored on a 5-point Likert scale ranging from none of the time (1) to all of the time (5). Higher scores indicated greater levels of social support.38 Studies have demonstrated high internal reliability for the mMOS-SSS, with Cronbach alphas ranging from .88 to .93.38
The Native Hawaiian Cultural Identity Scale (NHCIS) consisted of 4 items, ranging on a 1–5 rating scale, and measured the individual’s self-reported knowledge, attitudes, and association with Native Hawaiian heritage and lifestyle. Total scores ranged from 4 to 20; higher scores indicated stronger identity and affiliation with Hawaiian culture. This scale has been administered to other Native Hawaiians through the Kohala Health Research Project.39 Although Cronbach alphas were not reported for this scale, the NHCIS has demonstrated good convergent and divergent validity.39
Adversity
The construct of Adversity was based on two constructs: 1) socio-economic status (SES) based on income and educational attainment and 2) perceived racism based on the Everyday Discrimination Scale. Education and income were measured through categorical responses, reverse-scored, then converted to z-scores (referred to as SES or reverse-scored SES hereafter), while discrimination scores were converted to z-scores. The adversity construct was calculated based on the mean of SES and perceived discrimination. Because the construct of adversity did not demonstrate a good model fit as a unidimensional construct, adversity was considered as two constructs in the final model consisting of reverse-scored SES and discrimination.
Reverse-scored SES (educational attainment and household income) was based on the reverse-coding of income and educational status. Annual household income was collapsed into four ranges and coded as follows: (1) less than $25,000; (2) $25,000 to $49,999; (3) $50,000 to $74,999; and (4) $75,000 or more. Education was measured by asking participants to report the highest grade or year of school completed. The final categories of education were as followed: (1) no high school diploma, high school graduate/General Education Development (GED), (2) some college/technical school, and (3) college graduate. For the purpose of this study, those with lower levels of income and education were categorized as experiencing increased adversity.
Discrimination was measured through the Everyday Discrimination Scale (EDS).40 The EDS was a 9-item scale that assessed a person’s perceived discrimination based on a Likert scale ranging from 1 to 6 (never to almost everyday). Total scores ranged from 9 to 54, with higher scores indicating increased frequency of everyday discrimination. An example item included “You are treated with less courtesy than other people are”. Participants were also asked to indicate the reasons for their endorsed experiences (e.g., race, gender, skin), which impacted their composite score. If a person indicated that the reason for discrimination was due to race, ancestry, or national origins, their composite score remained. If a person indicated another reason for these experiences (i.e., gender, education level or income, physical disability), the composite score was computed as a zero to allow for a final construct of perceived acts of racism.
Number of health conditions (NHC) as a covariate
To test the mediation versus moderation model of resilience, participants were asked to indicate if a physician ever told them they had or have the following selected health conditions: cardiovascular disease (1 = yes, 0 = no), diabetes (1 = yes, 0 = no), cancer (1 = yes, 0 = no), and depression (1 = yes, 0 = no). Participants also were asked to report their weight (“About how much do you weigh in pounds without shoes?”) and height (“About how tall are you [in feet and inches] without shoes?”), from which Body mass index (BMI) was calculated as weight (kg)/[height (m)]2. Those with a BMI of 25–29.99 were considered overweight (overweight= 0.5) and those with a BMI of 30 were considered obese (obese = 1). Findings were transformed to calculate mean of the selected health conditions, which ranged from 0 (absence of health conditions), 0.2 (presence of one health condition), 0.4 (presence of two health conditions), 0.6 (presence of three health conditions), 0.8 (presence of four health conditions), or 1 (presence of all five conditions).
Outcome measure of self-rated health status (SRH)
Self-rated health (SRH) was assessed through the 12-item Short Form Health Survey (SF-12).41 The SF-12 was originally developed based on research from the RAND Medical Outcomes Study. The SF-12 constitutes the few validated health surveys that measure subjective and functional health status through multiple domains of health, including physical health, bodily pain, general health, vitality, social functioning, emotional health, mental health, and physical functioning.40 The Composite Score of the SF-12 was calculated as the outcome variable of self-rated health by taking the average of all items included in the SF-12. Each item was calculated based on the following equation: 100 × [(observed score – minimum possible score)/(maximum possible score – minimum possible score)]. This equation has been utilized in other studies, such as the RAND Medical Outcomes Study, to score self-rated health.40 Each item was converted to a scale from 0 to 100 with final composite scores ranging from 0 to 100. Higher scores indicated higher levels of positive subjective health.
Procedures
This study was approved by all community partners and the University of Hawai’i at Mānoa Institutional Review Board (IRB). The measures of this study were part of a larger survey (Hawaiian Homestead Health Survey) under the project titled, Cancer-Related Behaviors and Cancer Screening Assessment of Hawaiian Homesteads. The overall project incorpo-rated community-based participatory research princi-ples to assess modifiable SES, socio-cultural, and psychosocial factors associated with cancer-related health behaviors in adult Native Hawaiians residing on Hawaiian homestead lands.
In January 2015, three documents were mailed to prospective participants. One survey was mailed to each household. These documents included: 1) a consent form, 2) a personalized cover letter describing the purpose of the project, and 3) the Homestead Health Survey packet. After completing the survey, participants returned the surveys in a pre-addressed envelope and were compensated with a $15 gift card for participating in the study. By returning completed surveys, participants consented to participate in the study, as described in the consent form. Surveys were assigned an ID number to ensure confidentiality. Data were entered in REDCap, a secured, electronic database.
Statistical analyses
Data were exported to SAS 9.4 to determine participant characteristics, conduct correlational analyses, determine the reliability of individual scales, and create Mplus files for remaining analyses of this study. The validity of the resilience scale was based on several forms of validity: (1) factorial validity, which exists when the hypothesized structure is confirmed in an empirical test such as a CFA,42 (2) convergent validity, which exists when there is an overlap in tests that presumably measure the same construct,42 (3) discriminant validity, sometimes referred to as divergent validity, which exists when a construct does not correlate with other, theoretically distinct constructs,42 and (4) overall construct validity, based on the extent to which variables accurately measure constructs of interest, which exists in this study through the theoretically meaningful structural equation model comparisons, in addition to the previous mentioned validities.42,43
Factor analyses were conducted using Mplus Version 8.4. Mplus was used because it utilizes the full information maximum likelihood (FIML) approach to address missing scores and retain all data, rather than listwise deleting participants’ data. Based on the missing pattern frequencies generated by MPlus, it was confirmed that 112 (out of 124=90.3%) participants completed the full survey.
Goodness of fit statistics were reported for each model. Recommended RMSEA cutoff values have been .07 or lower,44 with a recommended CFI value of .95 or greater. 45 While RMSEA is a common measure of goodness of fit, Kenny, Kaniskan, and McCaoch (2015) have warned that RMSEA is overestimated when the model has small degrees of freedom and the sample size is small, regardless of any structural equation model. Therefore, in addition to assessing goodness of fit statistics, alternative comparison models were analyzed for this study.46
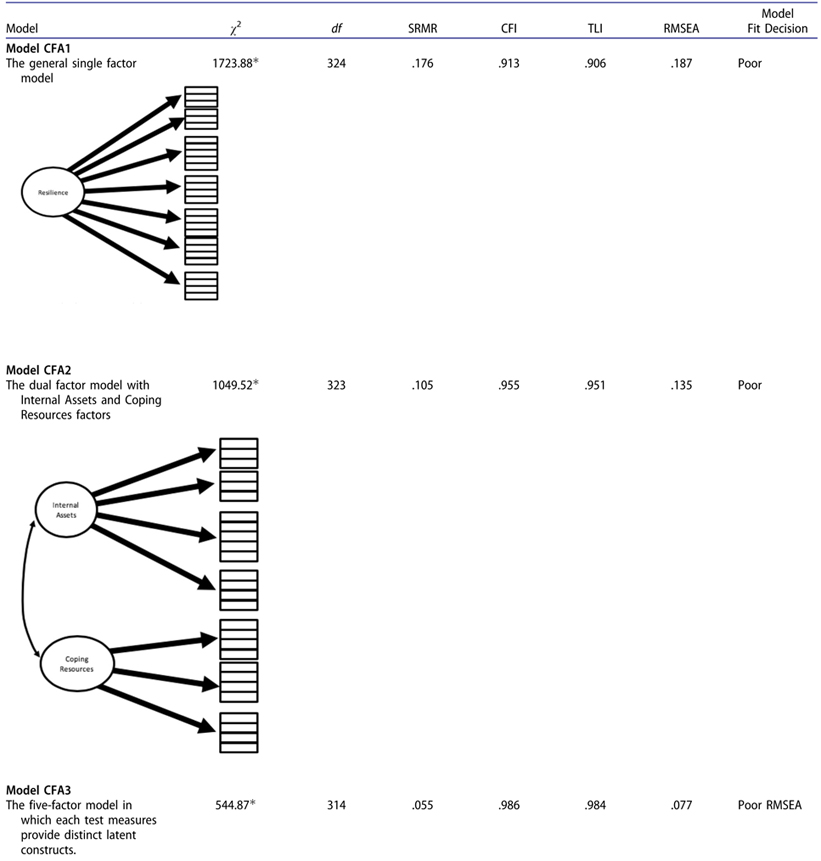
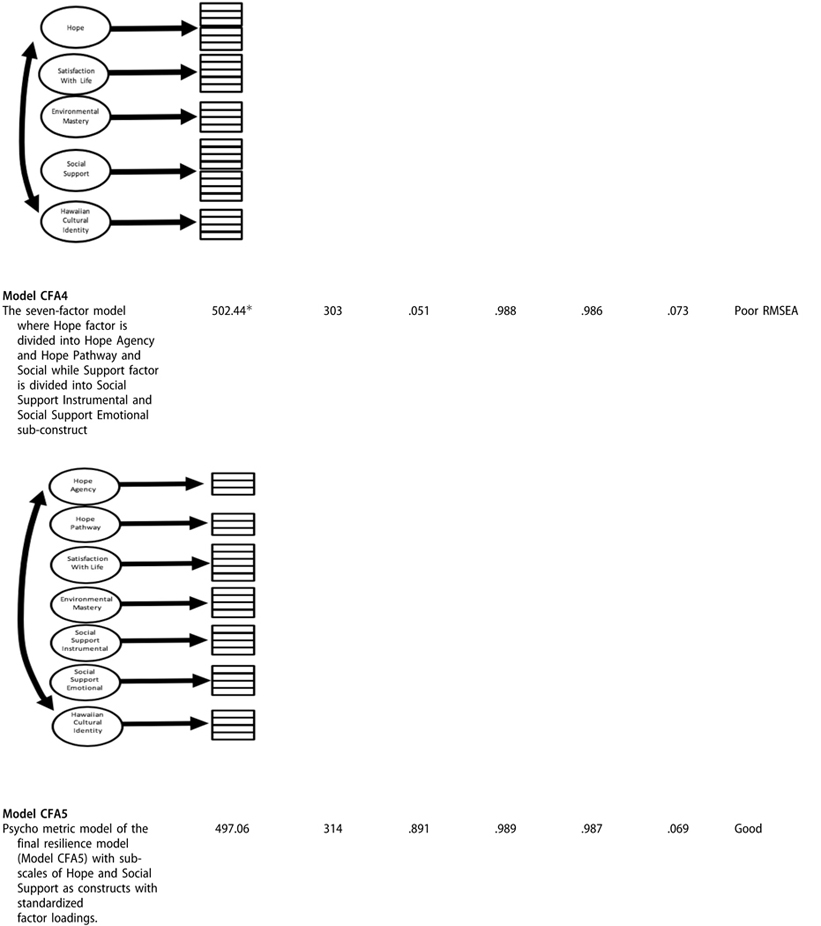
Five conceptually meaningful confirmatory factor models were analyzed. Model CFA1 was a single-factor model, in which an overall unitary construct was formed by all assessment items. Model CFA2 comprised two latent constructs: Internal Assets and Coping Resources. Model CFA3 was based on five latent constructs in which each separate assessment (Hope, Satisfaction in Life, Environmental Mastery, Social Support, and Hawaiian Cultural Identity) was designed to measure a distinct latent construct. Model CFA4 was an extension of Model 3 with 7 constructs, including the subscales of Hope and Social Support, without any higher-order factors. Model CFA5 was the final proposed model of Resiliency. The resilience construct consisted of four hierarchical levels: individual internal assets (Hope, SWLS, EMS) and coping resources (mSSS and NHCID), with an additional level of Hope agency and Hope pathways under the Hope subscale, and Social Support instrumental and Social Support emotional under the Social Support subscale. Parameters for the CFA models were estimated by robust estimators for the categorical factor analyses via weighted least square with mean-variance adjustment (WLSMV). The proposed Resilience factor model was statistically compared with alternative confirmatory factor models with the scaled likelihood ratio difference tests.44
Once the factor structure was determined, the internal consistency (i.e., Cronbach alpha & McDonald’s Omega) was computed for each scale (e.g., Hope Scale) and construct (e.g., internal assets) using the JASP software.47 The minimal cutoff of Cronbach alpha and McDonald’s Omega for each scale was set at .70 or greater. Because different rating scales were used across the higher-order constructs (e.g., internal assets, coping resources, resilience composite scores), z-scores (mean = 0.0, standard deviation = 1.0) were calculated, and the means of the z-scores served as the composite scores. Internal assets comprised the mean of z-scores for the Hope, Satisfaction With Life, and Environmental Mastery scales. Coping resources comprised the mean of z-scores for Social Support and Native Hawaiian Cultural Identity. Resilience comprised the mean of z-scores for internal assets and coping resources.
The inter-factor correlations among these composites were computed and used as measures of convergent and divergent validity.42 Although one would expect all of the inter-factor correlations to be positive in light of the confirmatory factor analysis and the measurement of a common, underlying construct of resilience, one would not expect all of the positive correlations to be equal, especially given the subscales that purport to measure different aspects of the underlying construct of resilience. For example, one would expect higher correlations among the internal assets factors and among the coping resources factors, and lower coefficients between the set of internal assets factors and set of coping resources factors. The inter-scale correlations were also computed to determine the convergent and divergent validities of the AREC with other non-resilience measures (i.e., socioeconomic, number of health conditions, self-reported health). For example, one would expect higher correlations among the internal assets, coping resources, and construct of resilience, and lower coefficients between the AREC and number of health conditions or varibales of socio-economic status.
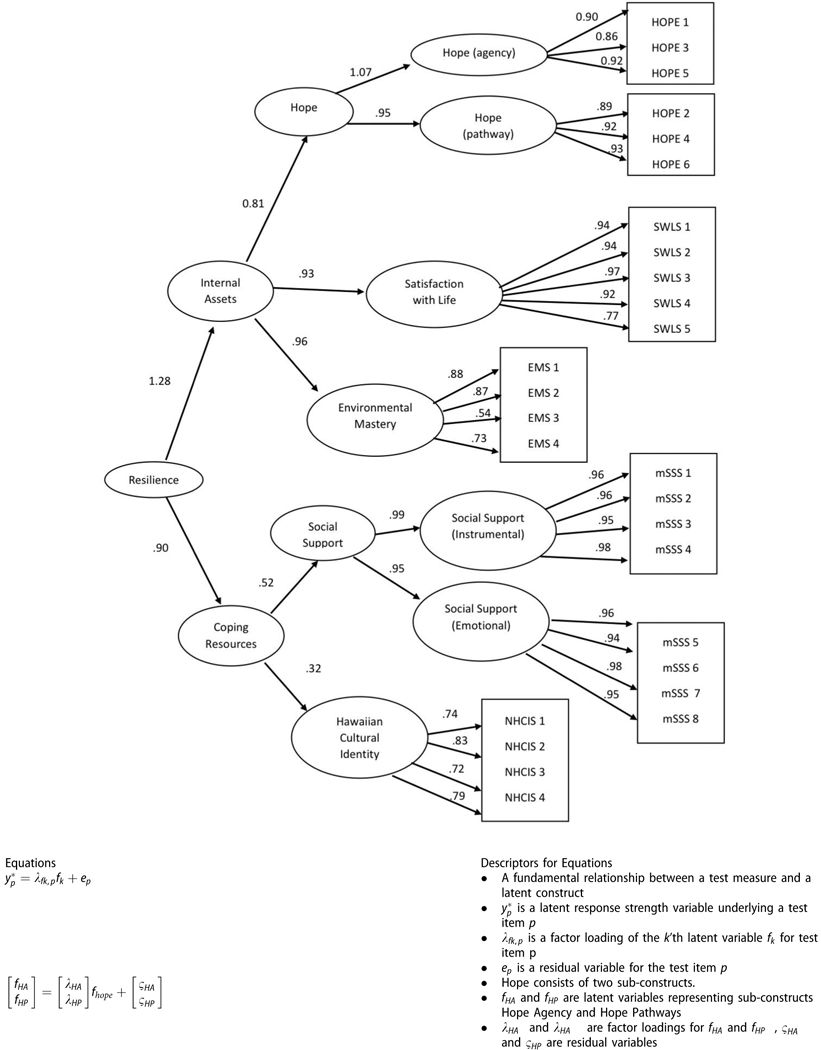
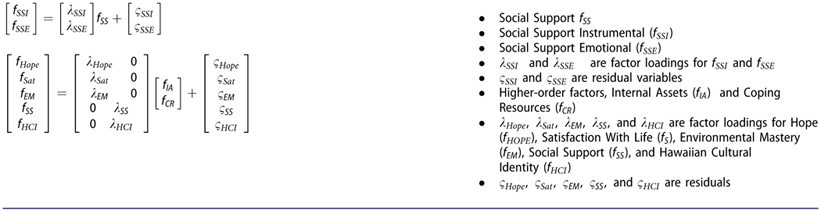
Latent factor structures were used to conduct six Structural Equation Models (SEMs). SEMs were tested to determine whether resilience serves as a mediator or moderator of adversity on health. Models 1 and 2 established the coefficients of the mediation model and determined whether resilience serves as a mediator of adversity on health. Model 3 presents the partial mediation model, which determines whether the relationship between resilience and health continued to exist after resilience was included as a mediator of adversity. Model 4 was tested next to determine whether the mediation model demonstrated a full mediation based on the direct relationship between adversity and health and the indirect relationship with resilience as a mediator. Model 5 tested the moderation model, which determined whether resilience served as a moderator of health. Model 6 tested for the interaction between adversity and resilience, as moderators of health. Theoretically meaningful results of these model comparisons, along with the factorial, convergent, and divergent validities, contributed to the overall construct validity of the AREC.42,43
Results
Participant characteristics
The final sample of this study comprised 124 adults who were 18 years of age or older. Table 1 provides a summary of participant characteristics, including demographic information and average scores of measures included in this study. A description of each measure is described above in the methods section.
Psychometric model and confirmatory factor analysis
Factorial validity
A summary of the abbreviated path diagrams for Confirmatory Factor Analysis (CFA) models and goodness of fit statistics are displayed in Table 2. The final CFA model (Model CFA5) of resilience comprised internal assets and coping resources with Hope and Social Support as two respective subscales. Model fit indices demonstrated good fit with an RMSEA of .069 and a CFI of .99. The final CFA model (CFA5) was compared against other factor models, which allowed for an analysis of alternative comparison models.43 An adjusted fit difference between Model CFA1 and Model CFA5 was statistically significant (SB Δχ2 = 298.336, Δdf=10, p < .01). The scaled fit difference between CFA2 versus CFA5 was also statistically significant (SB Δχ2 = 211.1, Δd f = 9, p <.01). For the comparison between CFA3 and CFA5, the scaled chi-square was SB Δχ2 = 24.9 (p = undefined) in favor for Model CFA5, with no difference in degrees of freedom. CFA4, despite having more parameters in the model, was worse than CFA5 in terms of misfit. Thus, CFA5 was superior to account for the covariance information of test items (SB Δχ2 = −36.3, Δdf = −11, p <.01). We concluded CFA5, or the proposed Resilience factor model, was the most tenable model among alternative candidate factor models in terms of statistical testing and from the conceptual perspective.
Table 2.
Abbreviated path diagrams for Confirmatory Factor Analysis (CFA) models and goodness of fit statistics.
 |
 |
 |
 |
Note: p < .05.
Reliability
Table 3 presents the internal consistency coefficients (i.e., reliability) for each factor subscale and composite. The results indicated overall good reliability with McDonald’s Omega and standardized Cronbach alphas that were greater than the recommended value of .70, with the exception of coping resources, with a standardized Cronbach’s alpha of .63, but a McDonald’s Omega of .77.
Table 3.
Correlation matrix of measures included in the Ad-hoc Resilience Enhancing Construct (AREC).
| McDonald’s Omega | Standardized Cronbach’s Alpha | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Internal Asset Scales | ||||||||||||||
| 1. Hope Agency | .89 | .89 | ||||||||||||
| 2. Hope Pathways | .91 | .91 | .90* | |||||||||||
| 3. Hope | .95 | .95 | .97* | .97* | ||||||||||
| 4. Satisfaction With Life | .94 | .94 | .68* | .62* | .67* | |||||||||
| 5. Environmental Mastery | .77 | .77 | .70* | .62* | .67* | .75* | ||||||||
| Coping Resources Scales | ||||||||||||||
| 6. Social Support Instrumental | .96 | .96 | .45* | .37* | .42* | .51 * | .39* | |||||||
| 7. Social Support Emotional | .96 | .96 | .40* | .35* | .39* | .49* | .37* | .88* | ||||||
| 8. Social Support | .97 | .97 | .44* | .37* | .41 * | .52* | .39* | .97* | .97* | |||||
| 9. Native Hawaiian Cultural Identity | .79 | .79 | .31* | .33* | .33* | .29* | .16 | .14 | .07 | .11 | ||||
| First Order Constructs of Resilience | ||||||||||||||
| 10. Internal Assets | .91 | .91 | .87* | .82* | .87* | .90* | .91* | .48* | .45* | .48* | .28* | |||
| 11. Coping Resources | .77 | .63 | .50* | .47* | .50* | .54* | .37* | .74* | .70* | .74* | .76* | .52* | ||
| Second Order Construct of Resilience | ||||||||||||||
| 12. Resilience | .87 | .86 | .80* | .75* | .80* | .85* | .76* | .69* | .65* | .69* | .58* | .89* | .85* |
Convergent and divergent validities based on inter-factor correlations
Correlations between the individual scales and subscales included in internal assets (i.e., Hope Agencies, Hope Pathways, Hope, SWLS, & EMS) ranged from .62 to .97 (p < .01) suggesting good convergent validity. The social support subscales were highly correlated (.88–.97, p < .01) with mSSS, suggesting convergent validity, and moderately correlated (.35–.52, p < .01) with the scales included in internal assets suggesting divergent validity. The cultural identity scale was the only construct that was not significantly related to the individual constructs included in the AREC or had low correlations with the other measures (.07–.33). The correlation among the z-scores of the calculated resilience construct scale were moderately to highly correlated (.58–.89, p < .01) with the other individual scales, internal assets construct, and coping resources construct, which also suggested good convergent validity.
Theoretical model of adversity, resilience, and health
Convergent and divergent validities based on inter-scale correlations
An inter-correlation matrix was generated to determine the bivariate relationships among the final variables included in the structural equation models: SES, perceived racism, resilience constructs (i.e., internal assets, coping resources), number of health conditions (NHC, covariate), and the composite score of self-rated health (SRH) based on the Short Form 12-Item Health Survey (outcome variable) (see Table 4). An alpha value of .05 was used to determine significant relationships.
Table 4.
Inter-correlation matrix of adversity, resilience, and health variables.
| Variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
|---|---|---|---|---|---|---|---|---|
| 1. Income level (reverse-scored) | 1.00 | |||||||
| 2. Educational attainment (reverse-scored) | .38** | 1.00 | ||||||
| 3. Perceived discrimination | −.18 | −.07 | 1.00 | |||||
| 4. Internal assets | 32** | −.28** | −.09 | 1.00 | ||||
| 5. Coping resources | −.22* | −.26** | −.01 | .52** | 1.00 | |||
| 6. Ad-hoc Resilience Enhancing Construct | .32** | 31** | −.06 | .89** | .85** | 1.00 | ||
| 7. Number of Health Conditions (NHC) | .23* | .18* | −.08 | −.17 | −.22* | −.22* | 1.00 | |
| 8. Self-Reported Health (SRH) Based on the Short Form 12-Item Health Survey Total Score | −.26** | −.28** | .00 | .36** | .20* | .33** | .33** | 1.00 |
Note: Income level and education attainment were based on reversed scores. Results are reported based on z-scores.
p < .05;
p < .01.
The correlations among the calculated resilience construct scale was highly correlated (.85–.89, p < .01) with internal assets and coping resources construct, suggesting good convergent validity, while the correlations between the calculated resilience construct scale was lowly correlated with reverse-scored income level (−.32, p < .01), reverse-scored education (−.31, p < .01), number of health conditions (−.22, p < .01), and self-rated health (.33, p < .01), indicating good divergent validity. Findings from Table 4 helped provide a foundation for subsequent structural equation models.
The correlations demonstrated negative and significant relationships between the set of SES measures and measures of resilience, including internal assets, coping resources, and the AREC with correlations ranging from −.22 to −.32 for income and −.26 to −.31 for educational attainment. Reverse-scored income level and educational attainment were also negatively correlated with self-perceived health based on the SF12 scoring. Resilience measures, including internal assets (r = .36, p < .01), coping resources (r = .20, p < .05), and the AREC (r = .33, p < .01) were positively correlated with self-perceived health based on the SF12. Perceived racism was the only measure that was not significantly related to other variables included in this study.
Structural equation modeling and construct validity
Structural equation modeling was used to determine the adequacy of fit and individual parameter estimates for six models to comparatively test the mediation and moderation theories of resilience.48 Final structural equation models and a summary of model fit statistics are presented in Table 5
Table 5.
Final structural equation models and summary of model fit statistics among alternative structural equation models (The path diagram is provided for the unconstrained structural equation model with standardized parameter estimates embedded in the path; various fit indices are provided for the unconstrained model as well as alternative models). In the models below, NHC = Number of Health Conditions, SES = Socio-economic Status, D = Discrimination, R = Resilience, SRH = Self-Rated Health. Effect sizes are provided below the models.
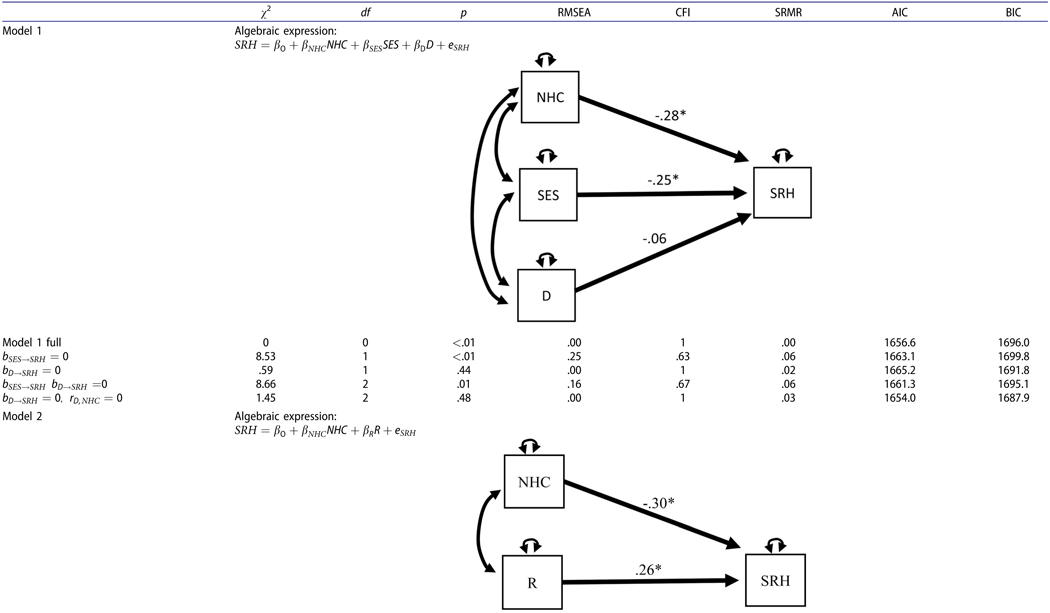 |
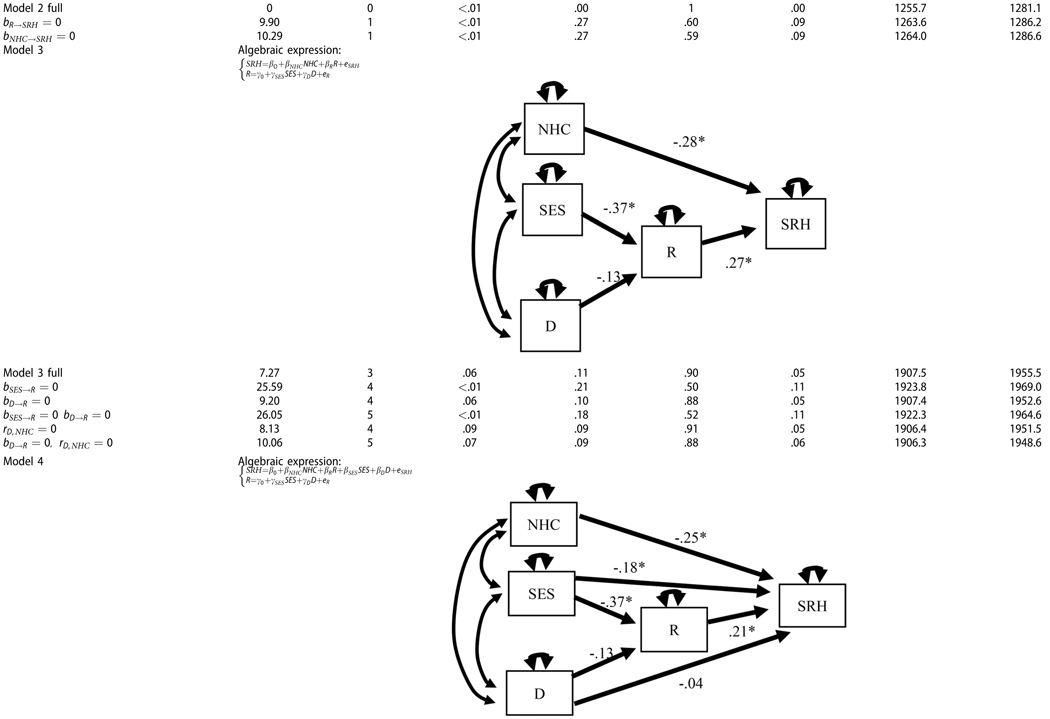 |
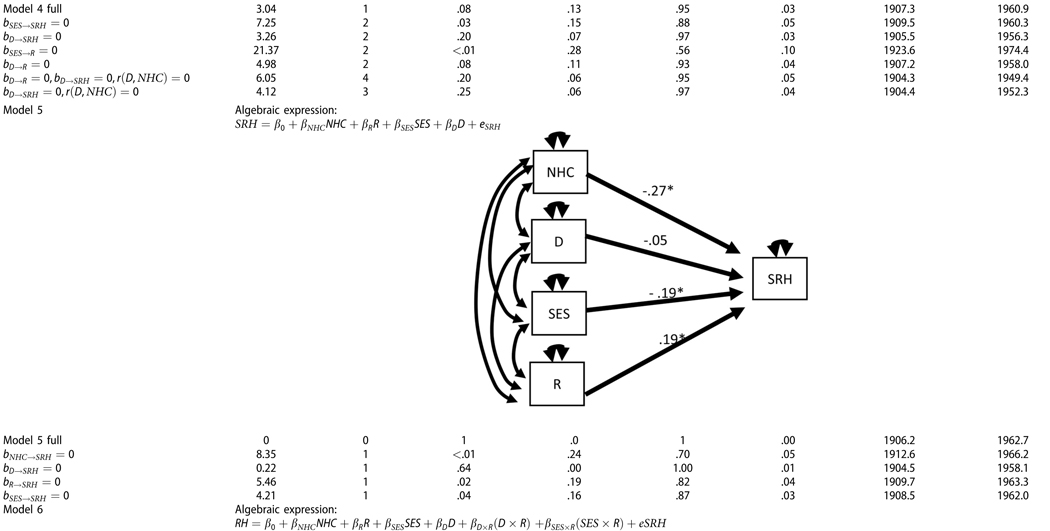 |
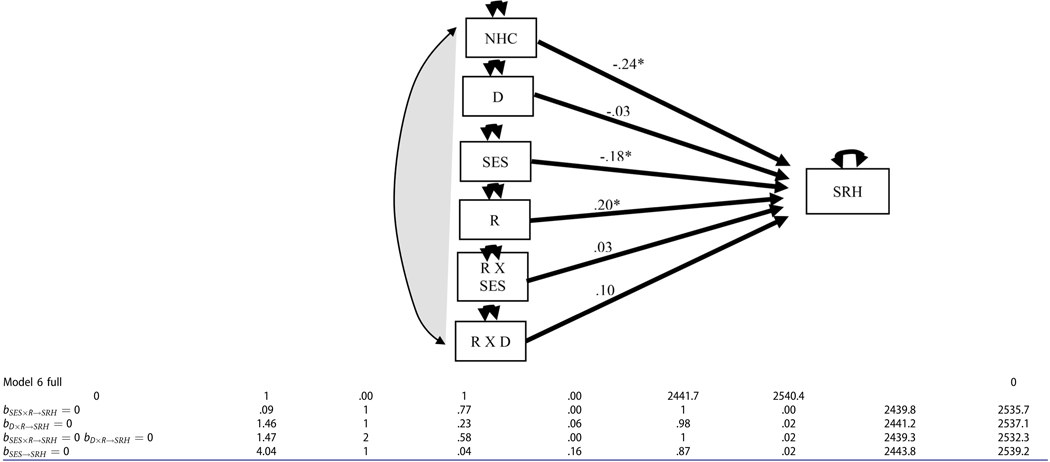 |
Note: εSES = .26 for the model 1 - the effect size of direct effect of SES on the self-reported health.
εSES,R =.39 for the model 3 - the effect size of indirect effect of SES on the self-reported health.
εSES,R = .39 for the model 4 - the effect size of indirect effect of SES on the self-reported health.
εSES,SF = .19 for the model 4 - the effect size of direct effect of SES on the self-reported health.
εSES,SF = .19 for the model 5 - the effect size of direct effect of SES on the self-reported health.
εSES,R = .37 for the simple regression model in which SES predicts Resilience.
εSES,R = .18 for the simple regression model in which SES predicts SRH.
In Model 1, the relationship between SRH and adversity in life was examined. SRH was inversely related to SES and Discrimination. When the effect of SES on health was removed from the equation, the misfit of the prediction model deteriorated and the effect size was εSES = .26 (Δχ2 = 8.53, Δdf = 1, p < .01). When the effect of Discrimination was removed the misfit difference was not statistically significant. In Model 2, the overall relationship between Resilience and the SRH was examined and was found to be positive (bR = .26). When this effect was removed from the model, the fit significantly worsened (Δχ2 = 9.90, Δdf = 1, p < .01).
In Model 3, the effect of Adversity on SRH was indirect, mediated by the Resilience factor. The indirect effect of SES on SRH was significant (bSES→R→SRH = −.10, p <.01), while the indirect effect of Discrimination on SRH was not statistically significant (bD→R→SRH = −0.03, p = .20). When the effect of SES on Resilience was removed from the model, the misfit worsened (Δχ2 = 18.32, Δdf = 1, p < .01). The statistical power to reject bSES→R = 0 was pH0≠true = .90. The statistical effect size was εSES→R = −.39.
In Model 4, the direct and indirect effects of adversity factors on self-awareness of health were tested. The indirect effect of SES on SRH (bSES→R→SRH = −.08, p < .01) and the direct effect of SES on SRH (bSES→SRH = −.18, p < .01) were statistically significant. This resulted in the significant total effect of SES on SRH (Total bSES→SRH = −.26, p < .01). For Discrimination, the indirect, direct, and total effects were all non-significant. When we removed the effect of SES on SHR from the model, the misfit worsened (Δχ2 = 4.21, Δdf=1, p = .04). The statistical effect size for the indirect effect of SES was εSES→R = .39. In contrast, the effect size of the direct effect of SES on SRH was εSES→SRH = .19. When the effect of SES on Resilience was removed from the model, the misfit worsened (Δχ2= 18.32, Δdf=1, p < .001). The statistical power to reject that bSES→R = 0 was pH0≠true = .95. Based on strict RMSEA fit statistics, the best mediation model was plausible when the direct effect of Discrimination to SRH was fixed at 0 and the exogenous correlation between Discrimination and NHC was fixed at 0 (RMSEA = .06, χ2 = 4.12, df=5, p = .25).
In Model 5, the mediation effect of adversity variables on health was disregarded, and instead, the model analyzed for the direct effect of adversity variables on health. Again, SES negatively impacted SRH (bSES→SRH = −.19, p < .05, εSES→SRH = .19). NHC was negatively influential on SRH (bNHC→SRH = −.27, p < .01), while the effect of Resilience was found to be positively influential on SRH (bR→SRH = .19, p <.05). When the effect of SES on SRH was removed, the model misfit significantly worsened (Δχ2 = 4.21, Δdf=1, p <.05). The effect of Discrimination on health was trivial (Δχ2 = .22, Δdf=1, p =.64). The statistical power to reject the hypothesis that bSES→SRH = 0 was pH0≠true=.90.
In Model 6, the moderation effects of Resilience with Discrimination and SES on SRH were analyzed. The interaction effect of Discrimination with Resilience was not statistically significant (Δχ2= 1.460, Δdf = 1, p = .227). Furthermore, the interaction effect of Discrimination by Resilience was not statistically significant (Δχ2= .09, Δdf = 1, p = .77). When both interaction terms were removed from the model, the misfit difference from the full Moderation model was statistically trivial (Δχ2= 1.47, Δdf = 2, p = .58). Thus, the moderation effect was not viable to account for variance of SHR. For the moderation model, the effect size of SES was εSES,R = .18.
Discussion
The overall purpose of this study was to estimate psychometric properties of scales that measured resilience-based factors through multiple levels using higher-order confirmatory factor analyses (CFA) and ascertain if this construct of resilience mediated or moderated adversity experienced by a sample of Native Hawaiians residing on Hawaiian Homestead Lands. The results of the overall study suggested that resilience is a multi-dimensional construct, consistent with recent research focusing on resilience.9 Furthermore, socio-economic burdens may be considered as substantial adversities for Native Hawaiians.
Findings from this study are consistent with recent literature, such as the multi-dimensional model of resilience.9,11 As predicted, the CFA demonstrated good model fit for the construct of resilience based on preexisting scales and recent definitions suggesting that resilience may exist as multiple factors (i.e., individual internal assets and external coping resources). These findings emphasize the importance of enhancing resilience, specifically among Native Hawaiian adults, by considering internal factors indicative of high resilience including hope, satisfaction with life, and mastery of one’s environment, while considering strengths available to an individual on the interpersonal and community levels.
The overall construct validity of the AREC was supported by the meaningful model comparisons, in addition to the factorial, convergent, and divergent validities. Inter-factor and inter-scale correlations between resilience measures and individual scales included in the construct were in the anticipated direction, suggesting convergent and divergent validity, with the exception of cultural identity. While the model demonstrated a good fit with cultural identity as a coping resource, the validity measures suggested that cultural identity may have better convergent validity with individual assets. To adhere with the proposed model based on the preexisting literature and because model fit indices indicated a good model fit, the final model consisted of cultural identity as a coping resource. Therefore, future research is needed to determine the role of cultural identity even further as a resilience enhancing factor. Future studies may also expand on this research by including other ethnic/cultural groups to determine the way cultural identity plays a role in adults who affiliate with different cultural backgrounds.
The second part of this study examined the way resilience factors based on the AREC construct mediated and moderated the effects of adversity on self-rated health in the sample of Native Hawaiian adults. The general findings support the negative effect that SES may have on self-rated health, while resilience may have a positive effect on self-rated health. Although the final SEMs indicated that resilience may slightly mediate and moderate the relationship between adversity and health, the overall model indicated that lower SES leads to poorer health despite the mediation of resilience factors. Although resilience factors did not reverse the negative association that adversity had on health, resilience factors slightly decreased the relationship between reverse-scored SES and health. Both the Mediating and Moderating Model demonstrated the significance of SES as an adversity that may uniquely impact health. These findings are consistent with the need to address adversity factors directly, with a specific need of addressing SES factors. In particular, increased efforts to address economic gaps and burdens that may be experienced by Native Hawaiians residing on Hawaiian Homestead Lands3 may aid in reducing some of the adversity experienced by Native Hawaiians.
The final models of this study indicated a non-significant relationship between perceived racism and self-rated health. Based on previous literature,22–26 one would assume that perceived racism would have a negative relationship with health. Upon examination of the inter-correlation matrix and the structural equation models, perceived racism did not have a significant relationship with health or additional variables examined in this study. While the findings suggest that perceived racism may not be as pertinent of a stressor or adversity as the socio-economic burdens experienced by Native Hawaiians, the data were limited to participants who selected race or ethnicity as the reason for acts of discrimination and does not account for other forms of discrimination. Moreover, it is possible that discrimination in specific forms (i.e., covert or overt)22 may interact with health differently and should be considered as separate factors in future research. Acts of discrimination (i.e., discrimination in general versus perceived racism) may also be considered in future research as potential factors of adversity.
Some of the strengths of the study were the incorporation of community-based approaches to holistically examine resilience, health, and health-related factors and psychometrically testing a model of resilience that may serve as a foundation for resilience research and interventions. This model of resilience continues to build on recent literature by incorporating individual internal assets, social support, and cultural identity, which were incorporated in multiple structural equation models to examine resilience as a mediating and moderating variable on adversity and health.
Despite the strengths of this study, limitations are also recognized. The current study was based on cross-sectional pilot data for the overall Hawaiian Homestead Health Survey initiative, and therefore, the direction of cause cannot be determined. Data were also based on a convenient sample on O’ahu that is more urban compared with other Hawaiian Homestead communities. Furthermore, the participation rate of 32% may have resulted in a non-representative sample. For example, approximately three-fourths of the partic-ipants in this study were female; they may experience resilience and health-related factors differently from men. This study also focused exclusively on Native Hawaiians who resided on urban Hawaiian Homestead Lands on the island of O’ahu, which may have impacted some of the suggested factors of resilience, including a sense of social support and identification with the Native Hawaiian culture that may not be experienced by all Native Hawaiian adults. Therefore, our data likely generalize to Native Hawaiians and Native Hawaiians residing on Hawaiian Homesteads on O’ahu. Finally, although there is no agreed-upon neces-sary ratio of participants to items,49 our ratio of approximately five participants for each item was on the low end.
Despite these limitations, this study has implications for future research, practice, and interventions focusing on health and resilience. Health and resilience may be perceived through a holistic lens, and thus, future research must consider resilience as a multi-dimensional construct, with additional emphasis given to external coping resources. Cultural identity may particularly serve as an important resilience factor in addition to social support. Increased attention to holistic practices and research, specifically research and practice that facilitate social support and are culturally based may foster resilience by addressing multiple dimensions of health. Future researchers should develop and test interventions to increase resilience and may specifically consider the incorporation of internal assets measured by hope, satisfaction with life, and environmental mastery and coping resources measured by social support and cultural identity.
Public policies should also emphasize a strengths-based approach to health by recommending that interventions and policies incorporate multi-dimensional factors of resilience on the individual, interpersonal, community, and cultural level. Future programs and policies may also aim to reduce economic disparities in light of the findings from this study, which identified socio-economic burdens as an adversity for Native Hawaiians.
Future researchers may consider utilizing a larger sample size to replicate the factor structure of the resilience model. Subsequent research should also investigate the way measures included in the AREC may enhance resilience among other Native Hawaiian populations. Future research may also expand on this study by including a diverse population of adults who affiliate with different cultures to understand the way cultural identity may help to facilitate resilience throughout Hawai’i and on a national level. Future research is also warranted to determine the way this construct of resilience may mediate or moderate the effect of adversity on health in research, practice, and future interventions. Exploring this relationship would determine the true concept of resilience, or the ability to overcome a situation expected to negatively impact health and wellbeing and demonstrate positive outcomes despite being exposed to adversity.
Conclusions
The findings from this study provide preliminary evidence that resilience consists of multiple components rather than serve as a unidimensional construct (i.e., resilience as a single factor). Although the findings of this study are specific to Native Hawaiian adults residing on urban Homestead Lands on the island of O’ahu and with a sample that was pre-dominantly female and middle-aged, the CFA confirmed a good model fit for this construct of resilience, with implications for future research and future interventions focusing on resilience. Findings from this study also support the fact that SES variables, specifically low household income and low education attainment, are adversely associated with perceived health. Resilience, on the other hand, may be positively associated with self-rated health. Findings from this study suggest that resilience may slightly mediate and moderate the effect that adversity has on health. Despite the limitations of the present study, there is a pressing need to conduct additional research with and by Native Hawaiians and other Indigenous Peoples to examine the mediating and moderating effects that resilience may have on the relationship between adversity and health, while also testing strategies that address adversity related to SES.
Acknowledgements
The authors would like to express their gratitude to Faith Kalamau, Kaapuni Kekauoha, and Morgan Torres for their contribution to data entry management. We also thank all of the participants and everyone who helped make this study possible.
Funding
This project, Cancer-Related Behaviors and Cancer Screening Assessment of Hawaiian Homesteads, was supported by a grant provided by the University of Hawai’i Cancer Center (UHCC). Funding for the time of biostatistics support was provided by grant number U54MD007601 from the National Institute on Minority Health and Health Disparities (NIMHD), a component of the National Institutes of Health (NIH). The contents of this paper are solely the responsibility of the authors and do not necessarily represent the official views of UHCC or NIH, nor does mention by trade names, commercial practices, or organizations imply endorsement by UHCC or NIH.
References
- 1.U.S. Statistics. Comprehensive census data by state. https://www.infoplease.com/us/comprehensive-census-data-state/demographic-statistics-78. Published 2019. Accessed July 31, 2019.
- 2.Hawai’i Health Data Warehouse. Community snapshot for Native Hawaiian race/ethnicity (DOH)—Community profiles. http://ibis.hhdw.org/ibisph-view/community/snap-shot/report/CommunityInd/RacEthDOH/2.html?PageName=. Published 2019.
- 3.Look MA, Trask-Batti 2019. Agres R MK, Mau ML, Kaholokula JK. Assessment and Priorities for Health & Well-Being in Native Hawaiians & Other Pacific Peoples. Honolulu, HI: Center for Native Hawaiian Excellence; 2013. http://blog.hawaii.edu/uhmednow/files/2013/09/AP-Hlth-REPORT-2013.pdf. Accessed July 31, 2019. [Google Scholar]
- 4.Kaholokula JK, Hermosura AH, Antonio M. Physical wellbeing of Native Hawaiians, the Indigenous people of Hawai’i. In Flemin C, Manning M, Miller A, eds. Routledge Handbook of Indigenous Wellbeing. Chapter 6. London: Routledge; 2019. [Google Scholar]
- 5.Pulla V What are strengths based practices all about? In: Pulla V, Chenoweth L, Francis A, Bakaj S, eds. Papers in Strength Based Practices, Pvt Ltd. New Delhi: Allied Publishers; 2012:51–68. [Google Scholar]
- 6.Zimmerman MA. Resiliency theory: a strengths-based approach to research and practice for adolescent health. Health Educ Behav. 2013;40(4):381–383. doi: 10.1177/1090198113493782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kirmayer LJ, Valaskakis GG. Healing traditions: the mental health of Aboriginal peoples in Canada. Vancouver: UBC Press; 2009:xxii, 503. [Google Scholar]
- 8.Grych J, Hamby S, Banyard V. The resilience portfolio model: understanding healthy adaptation in victims of violence. Psychol Violence. 2015;5(4):343–354. doi: 10.1037/a0039671. [DOI] [Google Scholar]
- 9.American Psychological Association. The road to resilience. http://www.apa.org/helpcenter/road-resilience.aspx. Published 2015.[AQ9] [Google Scholar]
- 10.Barton WH. Methodological challenges in the study of resilience. In: Ungar M, ed. Handbook for Working with Children and Youth. Thousand Oaks. London: Sage Publications; 2005. [Google Scholar]
- 11.Southwick SM, Vythilingam M, Charney DS. The psychobiology of depression and resilience to stress: implications for prevention and treatment. Annu Rev Clin Psychol. 2005;1(1):255–291. doi: 10.1146/annurev.clinpsy.1.102803.143948. [DOI] [PubMed] [Google Scholar]
- 12.Mau M, Blanchette P, Carpenter D, Kamaka M, Saito E. Lōkahi triangle. In: Health and Health Care of Native Hawaiian and Other Pacific Islander Older Adults. Standford, CA: eCampus-Geriatrics; 2010. http://geriatrics.stanford.edu/wp-content/uploads/downloads/ethnomed/hawaiian_pacific_islander/downloads/hawaiian_american.pdf. [Google Scholar]
- 13.Wagnild GM, Young HM. Development and psychometric evaluation of the Resilience Scale. J Nurs Meas. 1993;1(2):165–178. [PubMed] [Google Scholar]
- 14.Wagnild G A review of the resilience scale. J Nurs Meas. 2009;17(2):105–113. doi: 10.1891/1061-3749.17.2.105. [DOI] [PubMed] [Google Scholar]
- 15.Smith BW, Dalen J, Wiggins K, Tooley E, Christopher P, Bernard J. The brief resilience scale: assessing the ability to bounce back. Int J Behav Med. 2008;15(3):194–200. doi: 10.1080/10705500802222972. [DOI] [PubMed] [Google Scholar]
- 16.Cloud Ramirez L, Hammack PL. Surviving colonization and the quest for healing: narrative and resilience among California Indian tribal leaders. Transcult Psychiatry. 2014;51(1):112–133. doi: 10.1177/1363461513520096. [DOI] [PubMed] [Google Scholar]
- 17.Wexler L Looking across three generations of Alaska Natives to explore how culture fosters Indigenous resilience. Transcult Psychiatry. 2014;51(1):73–92. doi: 10.1177/1363461513497417. [DOI] [PubMed] [Google Scholar]
- 18.Carlton BS, Goebert DA, Miyamoto RH, et al. Resilience, family adversity and well-being among Hawaiian and non-Hawaiian adolescents. Int J Soc Psychiatry. 2006;52(4): 291–308. doi: 10.1177/0020764006065136. [DOI] [PubMed] [Google Scholar]
- 19.Pulla V What are strengths based practices all about? In: Pulla V, Chenoweth L, Francis A, Bakaj S, eds. Strength Based Practices. Pvt Ltd, New Delhi: Allied Publishers; 2012:51–68. [Google Scholar]
- 20.United States Census Bureau Publications. Poverty rates for selected detailed race and Hispanic groups by state and place: 2007–2011. http://www.census.gov/prod/2013pubs/acsbr11-17.pdf. Published 2013. Accessed July 31, 2019.
- 21.United States Census Bureau. Census. http://www.census.gov/2010census/. Published 2010. Accessed July 31, 2019.
- 22.McCubbin LD, Antonio M. Discrimination and obesity among Native Hawaiians. Hawaii J Med Public Health. 2012;71(12):346–352. [PMC free article] [PubMed] [Google Scholar]
- 23.Antonio MC, Ahn HJ, Ing CT, et al. Self-reported experiences of discrimination and depression in Native Hawaiians. Hawaii J Med Public Health. 2016; 75(9):266–272. [PMC free article] [PubMed] [Google Scholar]
- 24.Kaholokula JK, Iwane MK, Nacapoy AH. Effects of perceived racism and acculturation on hypertension in Native Hawaiians. Hawaii Med J. 2010;69(5):11–15. [PMC free article] [PubMed] [Google Scholar]
- 25.Kaholokula JK, Grandinetti A, Keller S, Nacapoy AH, Kingi TK, Mau MK. Association between perceived racism and physiological stress indices in Native Hawaiians. J Behav Med. 2012;35(1):27–37. doi: 10.1007/s10865-011-9330-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ing CT, Antonio M, Ahn HJ, et al. An examination of the relationship between discrimination, depression, and hypertension in Native Hawaiians. Asian Am J Psychol. 2019;10(3):249–257. doi: 10.1037/aap0000151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Evans-Campbell T Historical trauma in American Indian/Native Alaska communities: a multilevel framework for exploring impacts on individuals, families, and communities. J Interpers Violence. 2008; 23(3):316–338. doi: 10.1177/0886260507312290. [DOI] [PubMed] [Google Scholar]
- 28.Fergus S, Zimmerman MA. Adolescent resilience: a framework for understanding healthy development in the face of risk. Annu Rev Public Health. 2005;26(1): 399–419. doi: 10.1146/annurev.publhealth.26.021304.144357. [DOI] [PubMed] [Google Scholar]
- 29.Walsh F Family resilience: a framework for clinical practice. Family Process. 2003;42(1):1–18. doi: 10.1111/j.1545-5300.2003.00001.x. [DOI] [PubMed] [Google Scholar]
- 30.SMS Research Hawaii. DHHL Lessee Survey. In: Homelands SoHDoH. Honolulu, HI: SMS Research Marketing Services, Inc; 2008. https://dhhl.hawaii.gov/wp-content/uploads/2011/05/DHHL2008AppReportFinal.pdf. [Google Scholar]
- 31.Snyder CR, Hoza B, Pelham WE, et al. The development and validation of the Children’s Hope Scale. J Pediatr Psychol. 1997;22(3):399–421. doi: 10.1093/jpepsy/22.3.399. [DOI] [PubMed] [Google Scholar]
- 32.O’Keefe VM, Haroz EE, Goklish N, et al. Employing a sequential multiple assignment randomized trial (SMART) to evaluate the impact of brief risk and protective factor prevention interventions for American Indian Youth Suicide. BMC Public Health. 2019;19(1): 1675. doi: 10.1186/s12889-019-7996-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pavot W, Diener E. Review of the satisfaction with life scale. Psychol Assessment. 1993;5(2):164–172. doi: 10.1007/978-90-481-2354-4_5. [DOI] [Google Scholar]
- 34.Diener E, Emmons RA, Larsen RJ, Griffin S. The satisfaction with life scale. J Pers Assess. 1985;49(1): 71–75. doi: 10.1207/s15327752jpa4901_13. [DOI] [PubMed] [Google Scholar]
- 35.Ryff CD, Singer B. Psychological well-being: meaning, measurement, and implications for psychotherapy research. Psychother Psychosom. 1996;65(1):14–23. doi: 10.1159/000289026. [DOI] [PubMed] [Google Scholar]
- 36.Ryff CD. Happiness is everything, or is it? Explorations on the meaning of psychological wellbeing. J Pers Soc Psychol. 1989;57(6):1069–1081. doi: 10.1037/0022-3514.57.6.1069. [DOI] [Google Scholar]
- 37.Moser A, Stuck AE, Silliman RA, Ganz PA, Clough-Gorr KM. The eight-item modified Medical Outcomes Study Social Support Survey: psychometric evaluation showed excellent performance. J Clin Epidemiol. 2012;65(10):1107–1116. doi: 10.1016/j.jcli-nepi.2012.04.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sherbourne CD, Stewart AL. The MOS social support survey. Soc Sci Med. 1991;32(6):705–714. doi: 10.1016/0277-9536(91)90150-B. [DOI] [PubMed] [Google Scholar]
- 39.Kaholokula JK, Nacapoy AH, Grandinetti A, Chang HK. Association between acculturation modes and type 2 diabetes among Native Hawaiians. Diabetes Care. 2008;31(4):698–700. doi: 10.2337/dc07-1560. [DOI] [PubMed] [Google Scholar]
- 40.Williams DR, Yan Yu JS, Jackson NB, Anderson NB. Racial differences in physical and mental health: socio-economic status, stress and discrimination. J Health Psychol. 1997; 2:335–351. doi: 10.1177/135910539700200305. [DOI] [PubMed] [Google Scholar]
- 41.Ware J, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3): 220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 42.Vogt WP, Johnson RB. The SAGE Dictionary of Statistics and Methodology: A Nontechnical Guide for the Social Sciences. 5th ed. Los Angeles, CA: Sage; 2016. [Google Scholar]
- 43.American Educational Research Association. Standards for Educational and Psychological Testing. Washington, DC: American Educational Research Association; 2014. [Google Scholar]
- 44.Hooper D, Coughlan J, Mullen MR. Structural equation modeling: guidelines for determining model fit. Electron J Bus Res Methods. 2008;6:53–60. [Google Scholar]
- 45.Hu LT, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equation Model Multidiscip J. 1999;6(1):1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- 46.Satorra A, Bentler PM. A scaled difference chi-square test statistic for moment structure analysis. Psychometrika. 2001;66(4):507–514. doi: 10.1007/BF02296192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Team JASP. 2019. JASP (Version 0.11.1) [Computer software]. [Google Scholar]
- 48.Fairchild AJ, Mackinnon D. A general model for testing mediation and moderation effects. Prev Sci. 2009; 10(2):87–99. doi: 10.1007/s11121-008-0109-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Osborne JW, Costello AB. Sample size and subject to item ratio in principal components analysis. Pract Assess Res Eval. 2004;9(11):1–9. http://PAREonline.net/getvn.asp?v=9&n=11. [Google Scholar]


