Abstract
Background
Nationwide restrictions started in Finland in March to prevent the spread of COVID-19, leading to school and day care closures. The aim of this study is to describe the effect of closures and re-openings on the respiratory pathogen epidemiology.
Methods
Laboratory-confirmed cases of SARS-CoV-2; respiratory syncytial virus (RSV); influenza (A & B); parainfluenza-, adeno-, and rhinoviruses; Mycoplasma pneumoniae; and Streptococcus pneumoniae in children were collected from the National Infectious Disease Register over the period of 2017–2020. Weekly incidences (weeks 1 to 35) with 95% confidence intervals (CIs) were calculated per 100 000 children in 2020 and compared by incidence rate ratios (IRRs) to corresponding periods in 2017−2019.
Findings
The lockdown had immediate impact on the incidences of respiratory pathogens except SARS-CoV-2. Week after the lockdown began IRR was 0•3 (CI 0•3–0•4) and next week the IRR was 0•1 (0•1–0•2). The incidence of SARS-CoV-2 started to decline eight weeks after the lockdown began. The highest recorded weekly incidence of SARS-CoV-2 was 7•2/100 000 children. The effect of the lockdown lasted until late summer. Rhinovirus and SARS-CoV-2 began to increase before the schools or day cares opened in August. The re-opening of schools seemed to have no impact on the incidence of any pathogen.
Interpretation
Our results suggest that general social distancing, including school and day care closures, played a crucial role in reducing infections, and the effect lasted for several weeks. The re-opening of schools and day care centres seems to have had no immediate impact on the incidences of any respiratory pathogens.
Funding
This study had no funding source.
Keywords: COVID-19, Public health, Social distancing, Register study
Research in context.
Evidence before this study
Children attending school and day care have been shown to be an important source of general infection burden in influenza epidemics. During the COVID-19 pandemic, the role of children in spreading the virus has been controversial.
Added value of this study
In Finland, the nationwide lockdown restrictions have worked well in preventing the spread of both SARS-COV-2 and common respiratory infections in children. In this register study, we show that opening schools and day care centres did not cause an increase in the incidences of SARS-COV-2 or rhinovirus and that their incidences started to increase in the summer before the opening of day care centres and schools.
Implications of all the available evidence
Although day care centres and schools are important in spreading influenza, their impact seems to be much less in the COVID-19 pandemic and the spreading of rhinoviruses in the paediatric population.
Alt-text: Unlabelled box
1. Introduction
The Finnish government declared a state of emergency on 16 March 2020 (week 12) due to the COVID-19 pandemic, and a number of restrictions and recommendations entered into force to prevent the spread of the pandemic in Finland [1], [2], [3]. The main strategy was reducing in-person contacts and promoting social distancing. The use of facial masks was not recommended in the spring. Because of the wide restriction measures, close contacts and group activities among children decreased notably.
Soon after the onset of the restrictions, the number of all respiratory infections in children clearly declined [4]. RSV and influenza seasons were shorter compared to those of the previous four years [4]. Social restrictions and public health measures (e.g. social distancing and improved hand hygiene) to prevent COVID-19 transmission seemed to reduce the spread of seasonal influenza in Japan and China [5], [6], [7]. A study from the USA also demonstrated decreased rates of children's non-respiratory infectious diseases during social distancing [8]. However, a few previous reports have described the pathogen-specific incidences of laboratory-confirmed respiratory infections in children during and especially after the lockdown. The aim of this present study was to describe the effect of implementing and easing broad restrictions on the epidemiology of respiratory pathogens in the nationwide paediatric population in Finland.
2. Methods
2.1. Materials
In this retrospective register study, we collected the nationwide weekly numbers of positive SARS-CoV-2 findings in children aged 0 − 19 years and those of RSV; influenza viruses (A & B); parainfluenza-, adeno-, and rhinoviruses; Mycoplasma pneumoniae; and Streptococcus pneumoniae in children aged 0 − 14 over the period of 2017–2020. We grouped the SARS-CoV-2 findings by ages 0 − 9 and 10−19 years old and all other findings by 0 − 4, 5 − 9, and 10−14 years olds due the register design. The data were collected from the open-access National Infectious Disease Register (IDR) maintained by the Finnish National Institute for Health and Welfare (THL) [9].
All samples were taken on clinical basis. Influenza A/B and RSV PCR tests are taken also in primary care but multiplex tests are mainly performed at hospital settings. All tests are PCR tests from nasopharyngeal swabs but the register does not include the precise testing methods or the numbers of tests performed. For SARS-CoV-2, the testing capacity was limited during the first wave of COVID-19 in the spring of 2020, and only patients with quite severe symptoms and known exposure to COVID-19 were tested. Testing resources gradually increased during the summer 2020 and also children with less severe respiratory symptoms were tested in autumn 2020. Asymptomatic children have been tested only in some special occasions of large exposures. Overall, the nationwide weekly numbers of SARS-CoV-2 polymerase chain reaction (PCR) tests performed for all patients were included to demonstrate the nationwide testing capacity. No research permission is needed to access the open data. All data has been made available ass supplementary files.
2.3. Restrictions
Due to school closures, basic education was mostly carried out as distance learning, and the Finnish government recommended that parents arrange day care at home, if possible, from week 12–20 [2]. Also, public indoor premises were closed, and gatherings of more than 10 people were restricted. Good hand hygiene was recommended [11], and people were advised to stay home and avoid close contacts if they had any infection symptoms [12].
Schools were re-opened and the recommendation to arrange children's day care at home was annulled on 14 May 2020 (week 20) [13]. During the lockdown, approximately 78% of the day-care-aged children were at home, and when the closures lifted, over 62% of the children returned to day care centres, and 88% of the pupils returned to contact teaching [14]. Schools were open for two weeks, and the summer vacation started in week 23. During the school summer vacation period, the number of children in day care also decreased, and the number started to increase again at the beginning of August.
Travelling was restricted from March to June. In July and August it was possible to travel to countries with 14-day SARS-CoV-2 incidence less than 25/100 000 without quarantine. The limitations on gatherings were eased up to a maximum of 50 persons, and public indoor premises were gradually opened on 1 June 2020 (week 23) [15]. Furthermore, public events with more than 500 persons were allowed on 1 August 2020 (week 31). After ten weeks of summer vacation, pupils returned to schools in week 33. From week 33 on, THL recommended facial masks for people over 15 years of age when keeping a safe distance is not possible [16].
2.4. Statistical methods
Weekly incidences with 95% CIs for pathogens were calculated per 100 000 children from week 1–35 and compared by using incidence rate ratios (IRRs) to the corresponding weeks in the three previous years. We used Poisson's exact regression to calculate the CIs. The IRRs presented later included all other pathogens than SARS-CoV-2 and the IRR is based on their cumulative combined weekly incidence comparisons. The population for the age groups in Finland was collected for 2017–2020 from the population records of Statistics Finland [10]. We used IBM SPSS v. 27•0 for the statistical analyses. This study has been reported according to RECORD guidelines.
4. Results
We collected a total of 40 535 positive microbial findings from the register. Of these, 8 399 (20•7%) occurred from 1 January 2020 to 31 August 2020, and a total of 32 136 (79•3%) were found during corresponding dates in the reference years (2017−2019). The most common pathogens recorded in the register were influenza A & B (43•8%), RSV (32•2%), and rhinovirus (7•9%).
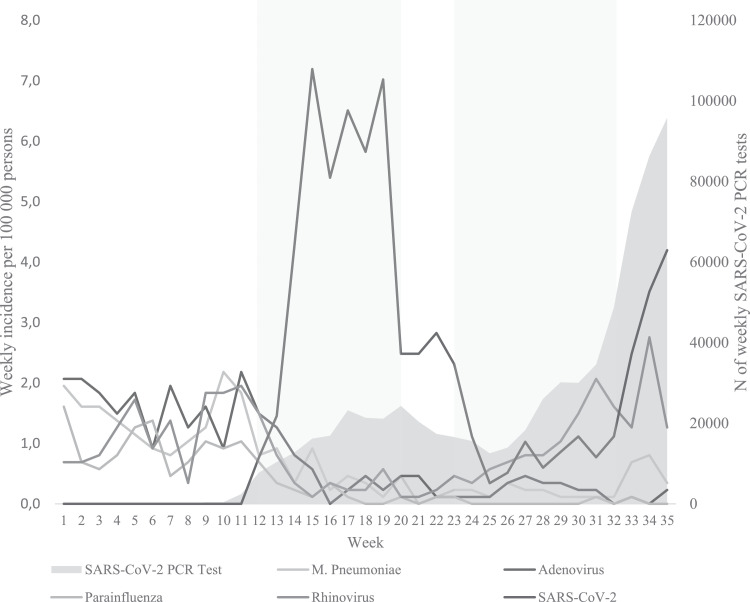
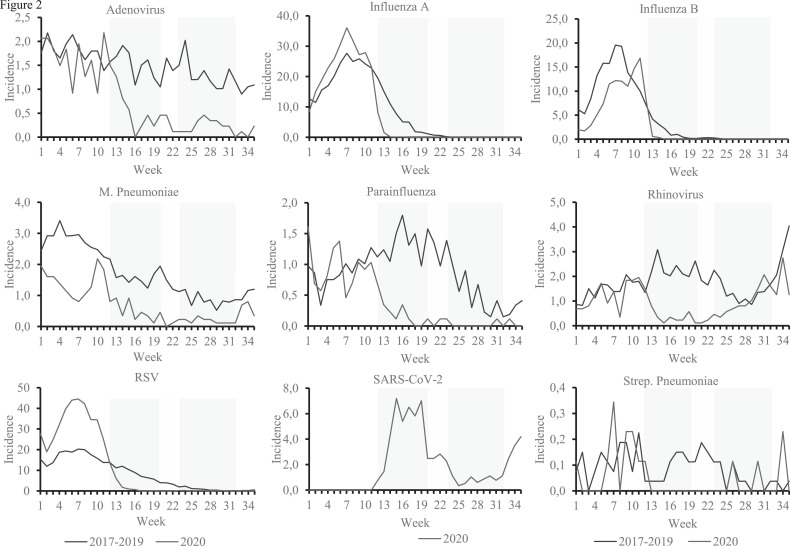
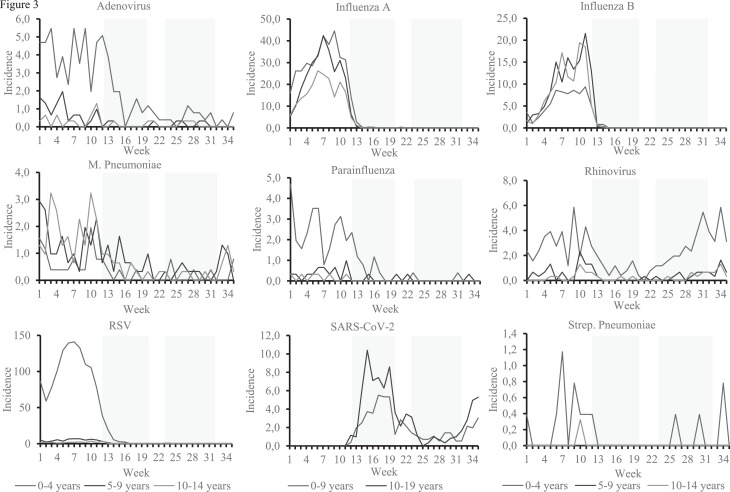
The immediate impact of the lockdown and closures of schools and day care centres was visible in the incidences of all respiratory pathogens other than SARS-CoV-2 (Table 1, Fig. 1, Fig. 2). The combined IRR for all respiratory findings was 0•3 (0•3–0•4) one week after the lockdown was announced and 0•1 (0•1–0•2) at two weeks. The incidences of parainfluenza- and adenoviruses differed the most from the reference years (Fig. 2). The impact was visible in all age groups (Fig. 3). At the beginning of the school and day care closures, the incidence of SARS-CoV-2 infections in children aged 0 − 19 years peaked (highest incidence 7•2/100 000, CI 5•8–8•9 in week 15). The increase ended quickly, and the incidence of SARS-CoV-2 remained stable until week 19. Incidences of all other respiratory pathogens remained significantly low during the lockdown (Table 1).
Table 1.
Weekly incidences with 95% CIs per 100 000 children of any positive laboratory-confirmed respiratory findings in 2020 compared to weekly mean incidence of 2017–2019 among patients aged 0 to 14 years by IRR with 95% CI. Pathogens included are RSV; influenza (A & B); parainfluenza-, adeno-, and rhinoviruses; Mycoplasma pneumoniae; and Streptococcus pneumoniae. SARS-CoV-2 incidences are for patients aged 0 to 19 years.
| All respiratory pathogens |
SARS-CoV-2 |
|||||||
|---|---|---|---|---|---|---|---|---|
| 2020 |
2017–2019 |
2020 |
||||||
| Week | incidence | 95% CI | Incidence | 95% CI | IRR | 95% CI | Incidence | 95% CI |
| Pre lockdown period | ||||||||
| 1 | 44.7 | (40.4–49.3) | 40.4 | (36.3–44.7) | 1.1 | (1.0–1.3) | – | – |
| 2 | 40.8 | (36.7–45.2) | 35.7 | (31.9–39.8) | 1.1 | (1.0–1.3) | – | – |
| 3 | 51.4 | (46.8–56.4) | 44.2 | (40.0–48.7) | 1.2 | (1.0–1.3) | – | – |
| 4 | 65.0 | (59.8–70.5) | 56.0 | (51.2–61.1) | 1.2 | (1.0–1.3) | – | – |
| 5 | 79.0 | (73.2–85.1) | 62.8 | (57.8–68.2) | 1.3 | (1.1–1.4) | – | – |
| 6 | 90.5 | (84.3–97.0) | 66.8 | (61.6–72.3) | 1.4 | (1.2–1.5) | – | – |
| 7 | 97.7 | (91.3–104.4) | 74.8 | (69.3–80.6) | 1.3 | (1.2–1.4) | – | – |
| 8 | 89.4 | (83.3–95.9) | 71.0 | (65.6–76.7) | 1.3 | (1.1–1.4) | – | – |
| 9 | 78.8 | (73.0–84.8) | 65.0 | (59.9–70.5) | 1.2 | (1.1–1.4) | – | – |
| 10 | 83.0 | (77.1–89.2) | 59.0 | (54.1–64.2) | 1.4 | (1.3–1.6) | – | – |
| 11 | 72.2 | (66.7–78.0) | 53.4 | (48.8–58.4) | 1.4 | (1.2–1.5) | – | – |
| Lockdown | ||||||||
| 12 | 34.3 | (30.6–38.4) | 46.5 | (42.2–51.1) | 0.7 | (0.6–0.9) | 0.8 | (0.4–1.4) |
| 13 | 11.6 | (9.5–14.0) | 37.0 | (33.2–41.2) | 0.3 | (0.3–0.4) | 1.5 | (0.9–2.3) |
| 14 | 3.9 | (2.8–5.4) | 33.6 | (30.0–37.6) | 0.1 | (0.1–0.2) | 4.3 | (3.2–5.6) |
| 15 | 2.8 | (1.8–4.0) | 27.0 | (23.8–30.6) | 0.1 | (0.1–0.2) | 7.2 | (5.8–8.9) |
| 16 | 1.7 | (1.0–2.8) | 21.4 | (18.6–24.6) | 0.1 | (0.0–0.1) | 5.4 | (4.2–6.9) |
| 17 | 1.0 | (0.5–1.9) | 19.9 | (17.1–23.0) | 0.1 | (0.0–0.1) | 6.5 | (5.2–8.1) |
| 18 | 1.0 | (0.5–1.9) | 15.3 | (12.9–18.0) | 0.1 | (0.0–0.1) | 5.8 | (4.6–7.3) |
| 19 | 1.0 | (0.5–1.9) | 13.6 | (11.3–15.1) | 0.1 | (0.0–0.1) | 7.0 | (5.6–8.7) |
| 20 | 1.1 | (0.6–2.0) | 12.6 | (10.5–15.1) | 0.1 | (0.0–0.2) | 2.5 | (1.7–3.5) |
| Schools and day cares re-opened | ||||||||
| 21 | 0.7 | (0.3–1.4) | 11.4 | (9.3–13.7) | 0.1 | (0.0–0.1) | 2.5 | (1.7–3.5) |
| 22 | 0.6 | (0.2–1.3) | 9.6 | (7.7–11.8) | 0.1 | (0.0–0.1) | 2.8 | (2.0–3.9) |
| School summer vacations | ||||||||
| 23 | 1.1 | (0.6–2.0) | 8.8 | (7.0–10.9) | 0.1 | (0.1–0.3) | 2.3 | (1.6–3.3) |
| 24 | 0.9 | (0.4–1.7) | 8.7 | (6.9–10.8) | 0.1 | (0.1–0.2) | 1,1 | (0.6–1.8) |
| 25 | 0.8 | (0.4–1.8) | 4.8 | (3.5–6.4) | 0.2 | (0.1–0.4) | 0.3 | (0.1–0.8) |
| 26 | 1.6 | (0.9–2.6) | 5.7 | (4.3–7.4) | 0.3 | (0.2–0.5) | 0.5 | (0.2–1.1) |
| 27 | 1.6 | (0.9–2.6) | 4.3 | (3.1–5.8) | 0.4 | (0.2–0.7) | 1.0 | (0.6–1.7) |
| 28 | 1.4 | (0.8–2.3) | 4.3 | (3.1–5.8) | 0.3 | (0.2–0.6) | 0.6 | (0.3–1.2) |
| 29 | 1.6 | (0.9–2.6) | 3.0 | (2.0–4.4) | 0.5 | (0.3–1.0) | 0.9 | (0.4–1.5) |
| 30 | 2.1 | (1.3–3.2) | 3.5 | (2.4–4.9) | 0.6 | (0.3–1.1) | 1.1 | (0.6–1.8) |
| 31 | 2.5 | (1.6–3.8) | 4.2 | (3.0–5.7) | 0.6 | (0.4–1.0) | 0.8 | (0.4–1.4) |
| Day cares continued | ||||||||
| 32 | 1.7 | (1.0–2.8) | 3.9 | (2.8–5.4) | 0.4 | (0.2–0.8) | 1.1 | (0.6–1.8) |
| Schools continued | ||||||||
| 33 | 2.3 | (1.4–3.5) | 4.3 | (3.1–5.8) | 0.5 | (0.3–0.9) | 2.5 | (1.7–3.5) |
| 34 | 3.8 | (2.7–5.3) | 5.8 | (4.4–7.6) | 0.7 | (0.4–1.0) | 3.5 | (2.6–4.7) |
| 35 | 1.8 | (1.1–2.9) | 7.2 | (5.6–9.2) | 0.3 | (0.1–0.4) | 4.2 | (3.1–5.5) |
Fig. 1.
Incidences of laboratory-confirmed respiratory pathogens in relation to school and day care closures and summer vacation among 0-to-14-year-old patients. SARS-CoV-2 infections among 0-to-19-year-old patients. The grey area presents the numbers of weekly SARS-CoV-2 PCR tests performed in Finland on patients of all ages. Pink boxes indicate the school and day care closures in the spring and summer vacation periods.
Fig. 2.
Weekly incidences of respiratory pathogens in 2020 in comparison to mean weekly incidences from 2017 to 2019. Children aged 0–14 years are included, and for SARS-CoV-2, children aged 0–19 years are included in the analysis. Pink boxes indicate the school and day care closures in the spring and summer vacation periods.
Fig. 3.
Weekly incidences of respiratory pathogens per 100 000 children grouped by age in 2020. Age groups are 0–4, 5–9 and 10–14 years for RSV; influenza (A & B); parainfluenza-, adeno-, and rhinoviruses; Mycoplasma pneumoniae; and Streptococcus pneumoniae. SARS-CoV-2 grouped to 0–9 and 10–19 years due to register design. Pink boxes indicate the school and day care closures in the spring and summer vacation periods.
When schools and day care centres were re-opened in week 20, the number of SARS-CoV-2 findings started to decrease (Fig. 1). The incidence dropped to 2•5/100 000 in week 20 and remained stable for a few weeks. The school opening seemed to have no observable impact on the incidence of SARS-CoV-2 or any other respiratory pathogen. The incidences remained lower compared to reference years (Table 1 and Fig. 2).
During the summer vacation period, the incidence of rhinovirus in children aged 0 − 4 years began to increase after week 21 (Fig. 3). In week 24, the incidence of SARS-CoV-2 started to decline again after the plateau, and the incidence reached the lowest rate in week 25 (0•3/100 000) (Table 1). During the summer, the number of SARS-CoV-2 infection cases started slowly to increase to the level of approximately 1•0/100 000.
During the last weeks of summer vacation, a rapid increase in the number of rhinovirus infections came after week 29, approximately the same time as in previous years. The increase was seen in the age group of 0 − 4 years old. In week 31, the incidence of rhinovirus (2•1/100 000, CI 1•6–3•8) was higher than the incidence of SARS-CoV-2 (0•8/100 000, CI 0•4–1•4) (Supplement 1). PCR testing for SARS-CoV-2 increased from week 27, and a sharp increase was seen after week 31 (Fig. 1).
When schools started after the summer vacation period, the incidence of SARS-CoV-2 (2•5/100 000, CI 1•7–3•5) exceeded the incidence of rhinovirus (1•3/100 000, CI 1.4–3.5) in week 33 (Fig. 1). Rhinovirus infections kept increasing, but not as much as in reference years (Fig. 2). Noteworthy changes in other respiratory infectious pathogens were not seen after the summer vacation.
Discussion
Studies have shown that children attending day care are at higher risk of infections [17], [18], [19], and children are thought to play an important role in infection transmission [20]. School closures have been a non-pharmaceutical intervention in previous influenza pandemics [3,20], and therefore reducing close contacts of children in day care centres and schools was a reasonable strategy to diminish the spread of SARS-CoV-2. According to our study, the restrictions, including the closure of schools and day care centres, were effective in reducing the spread of all respiratory pathogens, although the reduction of SARS-CoV-2 cases began later than for other respiratory pathogens.
The reduced spread of the common infectious pathogens in children due to the restrictive measures has also been observed in other studies [21,22]. In the USA, the incidence of streptococcal pharyngitis and acute otitis media decreased during the school closures [21]. In France the number of gastroenteritis, common cold, bronchiolitis and acute otitis media decreased over 70% in the paediatric population suggesting that especially viral or viral-induces infections reduced as a result of the national lockdown [22].
Our study demonstrates a sharp decrease in the incidence of influenza and the season ended rapidly in 2020 when comparing to previous years. Similarly to our results, a study from the USA showed a 98% decrease of positive influenza tests in adults and children during the lockdown and the number of positive tests remained low during the interseasonal circulation [23]. In Southern Hemisphere the restrictions came into force before the influenza season started and influenza activity kept exceptionally low over the whole influenza season in 2020 in the adult and paediatric population [23,24]. In addition to influenza, also positive RSV tests decreased remarkably [24]. In our study, the findings in the paediatric population were similar.
During the lockdown, SARS-CoV-2 was the prevailing pathogen, and its incidence decreased as a result of restrictive measures. Restrictions to prevent the spread of SARS-CoV-2 infections have been estimated to reduce the number of SARS-CoV-2 infections in one week, and the effect has been suggested to last for three weeks after easing restrictions [25]. According to our study, it took eight weeks before the restrictions affected the number of SARS-CoV-2 infections. One possible explanation for this finding is that in the spring 2020, testing was performed in Finland only for patients with clear symptoms (fever, acute respiratory symptoms) and known exposure to COVID-19 due to the limited testing capacity.
The incidence of SARS-CoV-2 infections started to increase 13 weeks after the school and day care closures were reversed. Other respiratory pathogens were immediately affected by the restrictions, and the re-opening of schools in the spring did not cause an increase in any infection incidences. These differences may account for the pre-existing immunity to the common viral pathogens and totally lacking immunity to SARS-CoV-2. The spread of the pathogens may also react differentially to improved hand hygiene and safety instructions where children with the slightest infectious symptoms were ordered to stay at home. Additionally, it must be noted that even though schools and day cares returned, the restrictions continued towards adult population. An increase was seen in the incidence of rhinovirus among 0 − 4 year olds after the day care centres were re-opened. The increase continued to be stable through summer vacations.
A recent study from the UK found that returning to schools after summer vacation was associated with an increase in rhinovirus infections in adults, and the authors suggested that children play a significant role in the spread of rhinovirus among adults [26]. In a study from Australia including both adult and paediatric population, the number of positive rhinovirus tests decreased sharply during restrictive measures in spring 2020 but started to increase quickly in May when restrictions to physical distancing were loosened to some extent [24]. In our study, the increase in the incidence of rhinovirus in children began in early summer, when school-aged children and some day-care-aged children were having summer vacation. The increase in summer was most likely due the lifting of social restrictions aimed towards adult population as bars were opened and restrictions for gatherings were eased. Instead, a rapid increase occurred before the return to day care centres and schools in August, but only in children aged 0 − 4. The incidence peaked at the same time as in previous years, although the increase in the incidence was not as high as previously. These results suggest that day care centres and schools may not be the main reason for the spread of rhinovirus. Furthermore, our previous report showed that the lockdown was effective in reducing paediatric emergency department visits; the visit rate normalized during summer vacation [4,27]. Also, the opening of schools and day care centres seemed to have had no influence on the rates of paediatric emergency department visits [27].
The increasing burden of rhinovirus and SARS-CoV-2 infections combined with the instructions to test for SARS-CoV-2 even in mild upper respiratory infections in children caused heavy congestion in health care and testing stations in August [28,29]. The testing chaos caused major delays (up to one week) from test to results, which led to unnecessary expenses and school and work absences, as the guideline was to wait for results in a quarantine-like environment. To prevent this from happening again, it is essential to monitor the epidemiology of other respiratory pathogens during epidemic situations and prepare the testing capacity and guidance.
The main strength of this study was the national open-access IDR, which is updated weekly and gives rapid information on the national microbial findings. The Finnish legislation mandates that laboratories report all positive findings to the register. The findings mostly come from hospitals and secondary/tertiary care paediatric emergency departments.
As for limitations, the data consist mainly of hospital-based data. However, the data were collected similarly during the study period. A further limitation is the absence of nationwide numbers of primary care and hospital visits due to infectious diseases, since this data will be available at the earliest in September 2021. Still, this study gives a good overview of the changes in the epidemiology of respiratory infectious pathogens in 2020 in relation to previous years. When interpreting the SARS-CoV-2 findings, it must be noted that the testing capacity was limited in spring 2020 in Finland like in all countries, which makes clear that our results underestimate the true incidence of SARS-CoV-2 during the first wave.
One possible limitation for our results is the missing number of tests performed for other pathogens, since the testing numbers are not recorded to the register. As the testing capacity was focused on SARS-CoV-2, it is possible that testing for other pathogens was limited and therefore the presented incidences could be underestimations. However, all published literature has shown remarkable reduction in all respiratory infections, and thus we feel our incidences are the best available estimation and describe the real incidences rather than limits in testing capacity.
In conclusion, the lockdown and social distancing were effective at mitigating the spread of respiratory infections. Also, our data suggest that the role of day care centres and schools might be smaller than previously thought in the transmission of rhinovirus. These results can be used in further decision-making on school and day care centre closures in an epidemic situation.
Declaration of Competing Interest
None of the authors have any potential competing interests to declare.
Acknowledgments
None.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.eclinm.2021.100807.
Appendix. Supplementary materials
References
- 1.WHO announces COVID-19 outbreak a pandemic. Mar 12, 2020 Web site. http://www.euro.who.int/en/health-topics/health-emergencies/coronavirus-covid-19/news/news/2020/3/who-announces-covid-19-outbreak-a-pandemic. Accessed Mar 22, 2020.
- 2.Preparedness for the novel coronavirus disease - A state of emergency in Finland. Mar 16, 2020 Web site. https://stm.fi/en/coronavirus-preparedness. Accessed Mar 19, 2020.
- 3.Bin Nafisah S., Alamery A.H., Al Nafesa A., Aleid B., Brazanji N.A. School closure during novel influenza: a systematic review. J Infect Public Health. 2018;11:657–2212. doi: 10.1016/j.jiph.2018.01.003. 661. [DOI] [PubMed] [Google Scholar]
- 4.Kuitunen I., Artama M., Mäkelä L., Backman K., Heiskanen-Kosma T., Renko M. Effect of social distancing due to the COVID-19 pandemic on the incidence of viral respiratory tract infections in children in Finland during early 2020. Pediatr Infect Dis J. 2020 doi: 10.1097/INF.0000000000002845. Publish Ahead of Print. [DOI] [PubMed] [Google Scholar]
- 5.Sakamoto H., Ishikane M., Ueda P. Seasonal influenza activity during the SARS-CoV-2 outbreak in Japan. JAMA. 2020;323:1969–2212. doi: 10.1001/jama.2020.6173. 1971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cowling B.J., Ali S.T., Ng T.W.Y. Impact assessment of non-pharmaceutical interventions against coronavirus disease 2019 and influenza in Hong Kong: an observational study. Lancet Public Health. 2020;5 doi: 10.1016/S2468-2667(20)30090-6. e279-2212;e288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sullivan S.G., Carlson S., Cheng A.C. Where has all the influenza gone? The impact of COVID-19 on the circulation of influenza and other respiratory viruses, Australia, March to September 2020. Euro Surveill Bull Eur Mal Transm. 2020;25:1. doi: 10.2807/1560-7917.ES.2020.25.47.2001847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hatoun J., Correa E.T., Donahue S.M.A., Vernacchio L. Social distancing for COVID-19 and diagnoses of other infectious diseases in children. Pediatrics (Evanston) 2020 doi: 10.1542/peds.2020-006460. [DOI] [PubMed] [Google Scholar]
- 9.Finnish national infectious diseases register. https://thl.fi/en/web/infectious-diseases/surveillance/infectious-disease-register. Accessed June 4, 2020.
- 10.StatFin statistics Finland's online service. https://www.stat.fi/org/avoindata/pxweb_en.html. Accessed Nov 8, 2020.
- 11.Hand hygiene can be further improved – handrubs should be possible in all public spaces. https://thl.fi/en/web/thlfi-en/-/hand-hygiene-can-be-further-improved-handrubs-should-be-possible-in-all-public-spaces-. Updated 2020. Accessed Nov 8, 2020.
- 12.Stay home if you have mild symptoms and seek medical help only if your symptoms are severe. https://thl.fi/en/web/thlfi-en/-/stay-home-if-you-have-mild-symptoms-and-seek-medical-help-only-if-your-symptoms-are-severe. Updated 2020. Accessed Nov 8, 2020.
- 13.Government decides to lift the restrictions on early childhood education and care and on primary and lower secondary education. https://valtioneuvosto.fi/artikkeli/-/asset_publisher/10616/hallitus-paatti-varhaiskasvatuksen-ja-perusopetuksen-rajoitteiden-purkamisesta?_101_INSTANCE_LZ3RQQ4vvWXR_languageId=en_US. Updated 2020. Accessed May 14, 2020.
- 14.Municipal survey: Across the country, 88 per cent of pupils took part in education after schools opened, with differences between provinces (in Finnish) http://www.avi.fi/web/avi/-/kuntakysely-koko-maassa-88-prosenttia-oppilaista-osallistui-opetukseen-koulujen-avauduttua-maakuntien-valilla-eroja.
- 15.Government decides on plan for hybrid strategy to manage coronavirus crisis and for gradual lifting of restrictions. https://valtioneuvosto.fi/artikkeli/-/asset_publisher/10616/hallitus-linjasi-suunnitelmasta-koronakriisin-hallinnan-hybridistrategiaksi-ja-rajoitusten-vaiheittaisesta-purkamisesta?_101_INSTANCE_LZ3RQQ4vvWXR_languageId=en_US. Updated 2020. Accessed May 14, 2020.
- 16.THL recommends the use of a face mask to protect others - hand washing and safety intervals are the most important ways to prevent coronary infections (article in Finnish). https://thl.fi/fi/-/thl-suosittaa-kasvomaskin-kayttoa-toisten-suojaamiseksi-kasienpesu-ja-turvavalit-ovat-tarkeimmat-keinot-ehkaista-koronatartuntoja. Updated 2020. Accessed Nov 5, 2020.
- 17.Louhiala P.J., Jaakkola N., Ruotsalainen R., Jaakkola J.J. Form of day care and respiratory infections among Finnish children. Am J Public Health. 1995;85:1109–2212. doi: 10.2105/ajph.85.8_pt_1.1109. 1112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Angoulvant F., Ouldali N., Yang D.D. Coronavirus disease 2019 pandemic: Impact caused by school closure and national lockdown on pediatric visits and admissions for viral and nonviral infections-a time series analysis. Clin Infect Dis. 2021;72:319–322. doi: 10.1093/cid/ciaa710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McBride J., Eickhoff J., Wald E. Impact of COVID-19 quarantine and school cancelation on other common infectious diseases. Pediatr Infect Dis J. 2020;39(12) doi: 10.1097/INF.0000000000002883. e449-e452. [DOI] [PubMed] [Google Scholar]
- 20.Cauchemez S., Ferguson N.M., Wachtel C. Closure of schools during an influenza pandemic. Lancet Infect Dis. 2009;9:473–481. doi: 10.1016/S1473-3099(09)70176-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Chen Y., Williams E., Kirk M. Risk factors for acute respiratory infection in the Australian community. PLoS One. 2014;9 doi: 10.1371/journal.pone.0101440. e101440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nesti M.M.M., Goldbaum M. Infectious diseases and daycare and preschool education. J Pediatr. 2007;83:299–2212. doi: 10.2223/JPED.1649. 312. [DOI] [PubMed] [Google Scholar]
- 23.Olsen S.J., Azziz-Baumgartner E., Budd A.P. Decreased influenza activity during the COVID-19 pandemic - United States, Australia, Chile, and South Africa, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1305–1309. doi: 10.15585/mmwr.mm6937a6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hsieh C., Lin C., Wang W.Y.C., Pauleen D.J., Chen J.V. The outcome and implications of public precautionary measures in Taiwan–Declining respiratory disease cases in the COVID-19 pandemic. Int J Environ Res Public Health. 2020;17:4877. doi: 10.3390/ijerph17134877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Li Y., Campbell H., Kulkarni D. The temporal association of introducing and lifting non-pharmaceutical interventions with the time-varying reproduction number (R) of SARS-CoV-2: a modelling study across 131 countries. Lancet Infect Dis. 2020 doi: 10.1016/S1473-3099(20)30785-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Poole S., Brendish N.J., Tanner A.R., Clark T.W. Physical distancing in schools for SARS-CoV-2 and the resurgence of rhinovirus. Lancet Respir Med. 2020 doi: 10.1016/S2213-2600(20)30502-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kuitunen I., Haapanen M., Artama M., Renko M. Closing Finnish schools and day care centres had a greater impact on primary care than secondary care emergency department visits. Acta Paediatr. 2020 doi: 10.1111/apa.15646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.A symptomatic child should be tested for corona if having a new respiratory infection or if there is reason to suspect exposure to the corona (article in Finnish). https://thl.fi/fi/-/oireinen-lapsi-tulee-vieda-koronatestiin-jos-hanella-on-uusi-hengitystieinfektio-tai-on-syyta-epailla-korona-altistumista. Updated 2020. Accessed Nov 6, 2020.
- 29.Corona testing is congested in many places in Finland - at worst it can take almost a week to get the test and wait for the result (article in Finnish). https://yle.fi/uutiset/3-11483598. Updated 2020. Accessed October 16, 2020.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.