Abstract
Purpose
The use of Endoscopic ultrasonography (EUS) in pediatric patients is not as common as in adults. The aim of this study is to evaluate the role of EUS in the diagnosis of pancreatobiliary disease in childhood.
Methods
Between December 2016 and January 2018, the findings of patients who underwent EUS were evaluated retrospectively.
Results
Of the 41 patients included in the study 25 were girls (61.0%), mean age was 12.2±4.2 years. EUS was performed for biliary colic in 21 (51.2%), for recurrent pancreatitis in 12 (29.2%), for cholecystitis/cholangitis in 5 (12.2%), and for acute pancreatitis in 3 (7.4%) patients. EUS had a significant clinical effect in the decision of treatment and follow-up of 6/21 biliary colic cases, in diagnosis and follow-up of 6/12 recurrent pancreatitis cases, in decision-making and monitoring of invasive procedures (ERCP/surgery) of 3/5 acute cholecystitis/cholangitis and 2/3 of acute pancreatitis cases as well as in follow-up of the other cases. The effectiveness of EUS in determining direct treatment and invasive intervention was 43.9%. None of the patients had complications related to the EUS procedure.
Conclusion
Although current guidelines show that EUS can be used in pediatric patients, this is limited to a few published studies. In this study, it is shown that EUS is a safe method for the diagnosis, follow-up and treatment of common pancreatobiliary pathologies in childhood.
Keywords: Child; Endosonography; Gallbladder, pancreas
INTRODUCTION
Endoscopic ultrasonography (EUS) provides high-resolution imaging for the evaluation of diseases of the gastrointestinal wall and adjacent organs such as pancreas, bile duct, and liver [1]. It has been used widely in adults since the early 1980s in the diagnosis, treatment and follow-up of diseases of these organ systems. Although the indications for diagnosis are well known in adults, EUS techniques are still limited in childhood [2,3]. Despite the lack of sufficient experience in pediatric patients, other valid diagnostic modalities such as ultrasonography (USG), computed tomography (CT), magnetic resonance imaging (MRI) or magnetic resonance cholangiopancreatography (MRCP) are more preferred [4]. However, there are a few studies in childhood that demonstrate the role and clinical impact of EUS, particularly to avoid endoscopic retrograde cholangiopancreatography (ERCP), a more invasive procedure [5,6].
The pancreatobiliary tract diseases are the essential scope of endo-sonographic diagnosis and intervention [7,8]. The use of EUS in pediatric patients with pancreatobiliary system diseases is not as common as in adults. Our main goal in this study was to evaluate retrospectively the role of EUS in the diagnosis and follow-up of common pancreatic and biliary system diseases in childhood.
MATERIALS AND METHODS
Patients
Between December 2016 and January 2018, 41 pediatric patients (age under 18 years old) who underwent EUS at least once in our institution were evaluated retrospectively. Demographic data, findings of conventional abdominal imaging (USG, MRCP, and ERCP), EUS indications and results were analyzed. The patients were categorized into 4 groups. Group 1 consisted of patients with biliary colic symptoms and EUS was performed following transabdominal USG evaluation as well as due to continued symptoms despite of medical treatment. Group 2 was the patients presented with recurrent pancreatitis (RP) attacks which is determined according to acute RP diagnostic criteria by the International Study Group of Pediatric Pancreatitis in Search for a Cure (INSPPIRE) [9]. EUS was performed in these patients due to the inadequacy of diagnosis with other imaging methods (USG and MRCP) which were performed in advance and to delineate the parenchymal changes. Group 3 were the patients who presented with cholecystitis/cholangitis symptoms (fever, vomiting, jaundice, abnormality in liver function tests), and in this group EUS was performed only after evaluation by MRCP and/or USG, which were insufficient for the evaluation of the biliary tract, especially the distal common bile duct. Group 4 patients were those who applied with gallstone-related acute pancreatitis attack and EUS performed only after applying USG and/or MRCP in order to evaluate the decision of ERCP or surgery.
Endoscopic ultrasonography procedure
EUS was applied to all patients following the evaluation by other imaging methods–USG, MR or MRCP. All the EUS procedures were performed by an experienced gastroenterologist using a radial echo endoscopy (Fujinon EG-530 UR2; Fujinon Co., Tokyo, Japan). Following 6-hour fasting period, patients were monitored throughout the procedure for the O2 saturation (with pulse oximetry) and heart rate while administering midazolam, propofol or ketamine by anesthesia care team. The results of the EUS were scored from the endoscopy reports by an independent gastroenterologist other than endoscopist. Hyperechoic foci, hyperechoic strands, lobular contour, cysts, main duct dilatation, duct irregularity, hyperechoic margins, visible side branches and stones were noted according to conventional EUS score for chronic pancreatitis [10]. Normal or low probability was recorded as consistent with 0–2 criteria, indeterminate or intermediate probability was recorded as consistent with 3-4 criteria, and high probability was recorded as consistent with 5–9 criteria. Patients with 3 or more of these criteria as a result of EUS were determined to be pathological.
The efficiency of EUS was evaluated in terms of diagnosis, treatment, and follow-up decision of the groups. The clinical effect of EUS was confirmed after the clinical and radiological diagnostic studies and is defined as (1) positive: due to confirmation of the final diagnoses in false-negative or false-positive results with other tests, or (2) negative: incorrect diagnosis of EUS due to false-negative or false-positive results.
Ethics
The study was approved by the Ethics Committee of University Hospital (decision no: 2018/140). Written informed consent forms were obtained from the parents and/or relatives of all the patients included in the study.
Statistical methods
All statistical analyses were performed using SPSS Statistics for Windows, Version 21.0 (IBM Co., Armonk, NY, USA). Data were presented as mean (median as well as mean)±standard deviation, and as number (n) and percentage (%).
RESULTS
Endoscopic ultrasound was performed on 41 patients between December 2016 and January 2018 in our department. Out of 41 patients, 25 (61.0%) were female, and 16 (39.0%) were male. The mean age of the patients at the time of EUS application was 12.2±4.2 years (range, 3.7–17.6 years), and these patients had a mean follow-up period of 21.3 months (range, 3–89 months).
EUS was applied to 21 patients (51.2%) with biliary colic, 12 (29.2%) with RP, 5 (12.2%) with cholecystitis/cholangitis, and 3 patients (7.4%) with acute pancreatitis symptoms. EUS was applied to the patients who underwent other tests in advance and there was a maximum period of 3 months (mean, 1.6 months) between other tests and EUS (Table 1).
Table 1. Comparison of demographic findings of patients.
| Variable | Clinical findings (n=41) | |||
|---|---|---|---|---|
| BC (n=21) | RP (n=12) | CC (n=5) | AP (n=3) | |
| Age (yr) | 12.1±4.2 | 16.7±3.6 | 10.6±2.4 | 9.4±3.1 |
| Sex (female/male) | 12/9 | 8/4 | 3/2 | 2/1 |
| Height Z score | −0.54±0.2 | −0.34±0.1 | −0.56±0.1 | −0.45±0.2 |
| Weight Z score | −0.63±0.9 | −0.73±0.2 | −0.54±0.2 | −0.51±0.5 |
| BMI Z score | −0.56±0.3 | −0.93±0.2 | −0.55±0.3 | −0.49±0.3 |
| Abdominal pain* | 21 | - | 5 | 3 |
| Jaundice* | - | - | 5 | 3 |
| Elevated liver function test* | - | - | 5 | 3 |
| Elevated amylase, lipase* | - | - | - | 3 |
| USG | 21 | 12 | 5 | 3 |
| EUS | 21 | 12 | 5 | 3 |
| ERCP | - | - | 2 | 1 |
| MRCP | - | 12 | 5 | 2 |
| Surgery treatment | 6 | - | 3 | 2 |
| Clinical follow-up | 15 | 12 | 2 | 1 |
Values are presented as mean±standard deviation or number only.
BC: biliary colic, RP: recurrent pancreatitis, CC: cholecystitis/cholangitis, AP: acute pancreatitis, BMI: body mass index, USG: transabdominal ultrasonography, EUS: endoscopic ultrasonography, ERCP: endoscopic retrograde cholangiopancreatography, MRCP: magnetic resonance cholangiopancreatography.
*During Endoscopic ultrasonography.
Evaluation of endoscopic ultrasonography with gallbladder stone presentation
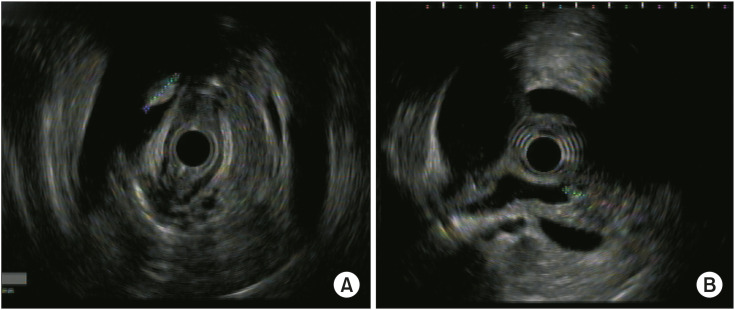
USG was applied to all patients with biliary colic symptoms. Gallbladder stones (mean diameter 7.6 mm; range 3 to 17 mm) were recorded in the EUS findings of all biliary colic patients with no history of cholecystitis/cholangitis attacks (Fig. 1). Cholecystectomy was performed in 6 (28.6%) patients after EUS procedure who could not be diagnosed or misdiagnosed with USG in advance. In 4 of the 6 patients, the size of the stones in the gallbladder was reported to be small on ultrasonographic evaluation (14 mm, 15 mm, and 17 mm). In 2 patients, while USG detected the gallstone in the corpus, surgery was performed due to its presence in the neck as reported in EUS. Because of the similarities of the findings between EUS and USG of the other patients, EUS was not applied again but rather follow-up decision was made.
Fig. 1. Endoscopic ultrasonography findings of the patients. Gallbladder stone 9.6 mm (A), choledocholithiasis 6.7 mm (B).
Evaluation of endoscopic ultrasonography with recurrent pancreatitis presentation
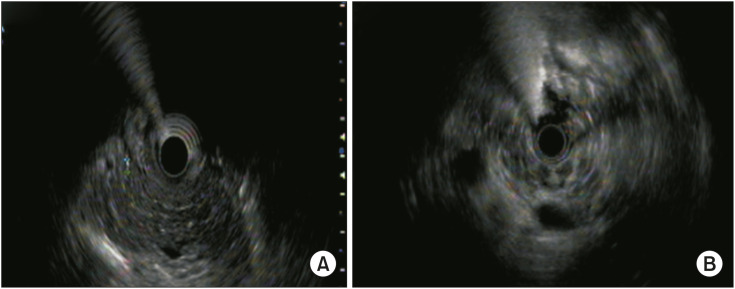
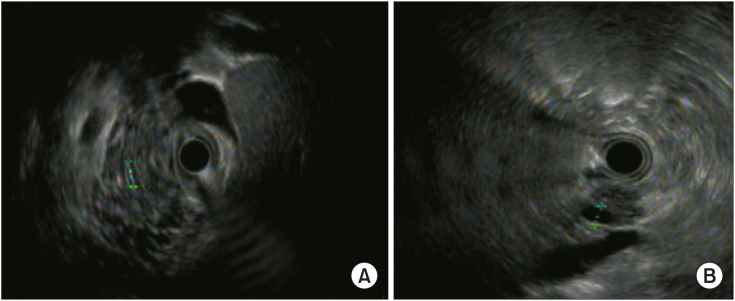
All patients with RP had USG and MRCP before EUS. The most common EUS finding of the 10 patients (83.3%) was hyperechoic strands ≥3 mm in the pancreatic parenchyma. According to the Conventional criteria, ≥3 pathological findings were determined in 7 (58.3%) patients (6 criteria in 4 patients, 4 criteria in 1 patient), 2 pathological findings in 3 (25.0%) patients and no pathological finding was present in 2 patients (Figs. 2 and 3). In three patients whose MRCP was inadequate (by the INSPPIRE) were diagnosed as chronic pancreatitis following EUS procedure which revealed the evidence of hyperchoic strands and lobularity. In six of RP patients EUS was applied to aid the diagnosis of chronic pancreatitis due to the lack of adequacy of other imaging modalities-MRI and USG, and the follow up decision was in made in these patients.
Fig. 2. Endoscopic ultrasonography findings of the patients. Hyperechoic strands (A), lobularity (B).
Fig. 3. Endoscopic ultrasonography findings of the patients. Hyperechoic duct wall (A) and dilatation of the main pancreatic duct (B).
Evaluation of endoscopic ultrasonography with cholecystitis/cholangitis presentation
In EUS, in five patients with history of cholecystitis/cholangitis attacks gallbladder stone and sludge were determined, and cholecystectomy and ERCP were performed in 3 (60.0%) and 2 (40.0%) of these patients, respectively. ERCP was applied in 3 patients following EUS in whom USG and MRCP could not evaluate the distal part of the common bile duct. In 2 patients, bile sludge was detected in EUS and ERCP.
Evaluation of endoscopic ultrasonography with acute pancreatitis presentation
Preceding the EUS procedure, in patients with acute pancreatitis, two underwent USG and MRCP, one patient USG only. The liver function tests (AST, ALT, total and direct bilirubin), amylase and lipase levels were high in these patients. Gallbladder stones and increment in bile duct width and pancreatic size were the EUS findings of three acute pancreatitis patients. Cholecystectomy and ERCP were performed in 2 and 1 of these patients, respectively, who could not be diagnosed with USG and MRCP. These patients underwent ERCP or cholecystectomy and no additional EUS was applied again.
The effectiveness of endoscopic ultrasonography
The EUS procedure had an impact in the decision of diagnosis, treatment and follow-up of the groups. In this study, EUS had a significant clinical effect in the decision of treatment and follow-up of 6/21 biliary colic cases, in diagnosis and follow-up of 6/12 RP cases, in decision-making and monitoring of invasive procedure (ERCP) in 3/5 of acute cholecystitis/cholangitis and in 2/3 of acute pancreatitis cases as well as follow-up of the other cases (Table 2). The effectiveness of EUS in determining direct treatment and invasive intervention was 43.9%. No complication has occurred in patients undergoing EUS procedure.
Table 2. Evaluation of the effectiveness of endoscopic ultrasonography in pediatric patients.
| Total (n=41) | Decision of diagnosis | Decision of treatment* | Decision of follow-up |
|---|---|---|---|
| Biliary colic (n=21) | - | 6 (28.6)† | - |
| Recurrent pancreatitis (n=12) | 6 (50.0)‡ | - | 6 (50.0)‡ |
| Cholecystitis/cholangitis (n=5) | 3 (60.0) | 3 (60.0)§ | - |
| Acute pancreatitis (n=3) | 2 (66.7) | 2 (66.7)∥ | - |
Values are presented as number (%).
*Surgery, endoscopic retrograde cholangiopancreatography (ERCP) or medical treatment. †Surgery due to the size and location of gallstones. ‡Follow-up decision upon finalizing the diagnosis. §3 patients avoided ERCP, 2 patients avoided surgery. ∥2 patients avoided ERCP, 1 patient avoided surgery.
DISCUSSION
Endoscopic ultrasound is becoming a more popular diagnostic tool and can be effectively utilized in pediatric population. Compared to the effectiveness of EUS in adult pancreatobiliary diseases, the experience in pediatric patients is limited with a few studies [11,12,13]. Many studies conducted with EUS in childhood showed a high positive effect in the management of diseases from 44 to 98% [11,12,13]. In this study, the effect of EUS in pancreatobiliary diseases in childhood was 43.9% and found to be reliable diagnostic tool in the follow-up of the patients. There was no false negative result of EUS in our study. According to the data presented in this study, the efficiency of EUS was found to be a useful and safe procedure in pediatric patients. In the review of literature, published in 2018 by Bizzarri et al. [14] stated that the effectiveness of EUS reached from 35.5% to 100% in the management of pediatric patients.
When pancreatobiliary diseases were examined in our study, EUS was applied most frequently in patients with gallstones, followed by, RP, cholecystitis/cholangitis and acute pancreatitis. In the study by Téllez-Ávila et al. [6] there were 54% recurrent acute pancreatitis, 25.9% microlithiasis, 16.7% chronic pancreatitis and 11.1% pancreatic tumor cases.
The prevalence of childhood gallbladder diseases has increased significantly for the last 20 years [15]. Nowadays, USG is the most widely used and first choice noninvasive examination method in patients with biliary system disease [16]. It is difficult to diagnose microlithiasis – gallstones smaller than 3 mm, in patients with biliary colic symptoms by USG. In the diagnosis of diseases such as microlithiasis, gallbladder sludge and choledocholithiasis, EUS has shown between 95 to 100% of precision [12]. A systematic review comparing EUS to MRCP found similar overall diagnostic performance while in another systematic review that included eight randomized trials demonstrated slightly higher overall accuracy for EUS as compared with MRCP (93 vs. 90 percent) for detecting choledocholithiasis [16]. In this study, 21 patients with biliary colic symptoms had stones in the gallbladder (mean diameter 7.6 mm; range 3 to 17 mm) in EUS findings. Following EUS procedure, 28.7% of these patients were underwent cholecystectomy. In our study, EUS was found to be effective in showing the size and location of gallbladder stones. Of 5 patients with the history of cholecystitis/cholangitis episodes with gallstone and sludge findings in EUS, cholecystectomy was applied to 60% and ERCP to 40% patients. Even the American Society of Gastrointestinal Endoscopy places the highest probability based on laboratory values and imaging studies at only greater than 50% in guidelines to stratify the presence of choledocholithiasis in adult patients [17]. EUS may prevent unnecessary cholecystectomy or ERCP in children with no evidence of microlithiasis [18]. Scheers et al. [5] showed that ERCP was prevented in 13 out of 17 children due to the findings in EUS. The increasing use of EUS in adult population has allowed for more sensitive detection of small gallstones that are missed on abdominal ultrasound or CT [19].
While EUS was performed in 29.2% patients with RP, the main indication for EUS was recurrent acute pancreatitis, which agrees with the reports of Varadarajulu et al. [20], Téllez-Ávila et al. [6] and Scheers et al. [5] According to the conventional criteria, only 7 patients who underwent EUS procedure for RP fulfilled the criteria of chronic pancreatitis. Because of non-invasiveness and lack of radiation the transabdominal USG and MRI are the first-line imaging modalities in the diagnosis and follow-up of recurrent/chronic pancreatitis in childhood. In this study, in patients with RP who had normal results in conventional evaluation and MRCP, parenchymal and ductal pathologies were observed in EUS procedure. In comparison to adult patients with RP the use of EUS in pediatric patients is occasionally reported [21,22,23]. EUS allows for a highly accurate assessment of pancreatic parenchymal and ductal changes and disease severity. Singh et al. [21] reported of 31% chronic pancreatitis cases in the study comprising of 32 pediatric patients with RP.
The incidence of childhood acute pancreatitis has been rising [24]. Endoscopic ultrasound is reported to be the most sensitive and highly specific diagnostic tool for choledocholithiasis and microlithiasis, which are responsible for at least half of all cases of acute pancreatitis [9,24,25,26]. The presence of gallbladder stone and increment in bile duct and pancreas size were documented in 3 patients with acute pancreatitis. Two of these patients underwent cholecystectomy and one patient underwent ERCP. In the study of Téllez-Ávila et al. [6] 3 patients had acute pancreatitis; in 1 of them, cholecystectomy was performed after the first acute pancreatitis following EUS procedure.
This study highlights the additional contribution and safety of EUS procedure to diagnosis, treatment and follow-up of common hepatobiliary diseases in pediatric patients. Although the therapeutic use of EUS was not necessary in our patients, it was important to evaluate the location and size of the stones, especially in patients with biliary colic for determining the treatment processes (follow-up or surgical decision). As in this study, EUS had a significant effect in deciding the treatment or follow-up process of the disease in patients with biliary colic who could not be diagnosed or misdiagnosed with other tests. In patients with RP, EUS made a significant contribution to detailed evaluation of parenchymal and ductal changes, or to patients who did not fully meet the INSPPIRE diagnostic criteria and other imaging methods were inadequate. In our patients with cholecystitis/cholangitis or acute pancreatitis due to bile duct stones, EUS has shown that it is a good alternative for diagnostic purposes in suspicious cases that cannot be diagnosed with other diagnostic methods, where it can detect bile duct dilatation, small stones and sludge. The EUS had a clinical significant effect for its role in the management of treatment and follow-up of 6/21 of biliary colic cases, in the diagnosis and follow-up of 6/12 of RP cases, in decision-making of invasive procedure (ERCP) and follow-up of 3/5 of acute cholecystitis/cholangitis cases and 2/3 of patients with acute pancreatitis as well as in follow-up of the other cases. As other valid diagnostic methods such as USG, CT, MRI or MRCP are more frequently preferred, EUS techniques are still bear a limited number of indications in pediatric patients. However, there is an increasing evidence to support the role and clinical impact of EUS, particularly to avoid unnecessary ERCP [17,27]. Ardengh et al. [28] showed with 83.2% accuracy of EUS in identifying of microlithiasis in adults with RP whom surgical histology confirmed in 75% patients. EUS was also found to be more accurate in evaluating microlithiasis of the gallbladder and early chronic/idiopathic pancreatic diseases [28,29].
The limitations of this study are the small number of patients and the limited use of EUS that is described only in pancreatobiliary diseases despite of its broad range of utilization in other pediatric diseases such as, pyloric stenosis, inflammatory bowel disease, vascular lesions and liver disease.
Even though guidelines state that EUS can be used in pediatric patients, such use is reviewed in restricted sources in literature. EUS, which has a significant clinical effect in the common pancreatobiliary pathologies in childhood, can be safely applied in the diagnosis, follow-up and treatment. New studies are needed to broaden the experience in pediatric patients.
Footnotes
Conflict of Interest: The authors have no financial conflicts of interest.
References
- 1.DiMagno EP, Buxton JL, Regan PT, Hattery RR, Wilson DA, Suarez JR, et al. Ultrasonic endoscope. Lancet. 1980;1:629–631. doi: 10.1016/s0140-6736(80)91122-8. [DOI] [PubMed] [Google Scholar]
- 2.Lakhole A, Liu QY. Role of endoscopic ultrasound in pediatric disease. Gastrointest Endosc Clin N Am. 2016;26:137–153. doi: 10.1016/j.giec.2015.08.001. [DOI] [PubMed] [Google Scholar]
- 3.Roseau G, Palazzo L, Dumontier I, Mougenot JF, Chaussade S, Navarro J, et al. Endoscopic ultrasonography in the evaluation of pediatric digestive diseases: preliminary results. Endoscopy. 1998;30:477–481. doi: 10.1055/s-2007-1001311. [DOI] [PubMed] [Google Scholar]
- 4.Suzuki M, Sai JK, Shimizu T. Acute pancreatitis in children and adolescents. World J Gastrointest Pathophysiol. 2014;5:416–426. doi: 10.4291/wjgp.v5.i4.416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Scheers I, Ergun M, Aouattah T, Piessevaux H, Borbath I, Stephenne X, et al. Diagnostic and therapeutic roles of endoscopic ultrasound in pediatric pancreaticobiliary disorders. J Pediatr Gastroenterol Nutr. 2015;61:238–247. doi: 10.1097/MPG.0000000000000692. [DOI] [PubMed] [Google Scholar]
- 6.Téllez-Ávila FI, Duarte-Medrano G, Herrera-Mora D, Lopez-Arce G, Leal-García M, Ramírez-Martínez M, et al. Endoscopic ultrasound in pediatric patients with pancreatobiliary disease. Surg Laparosc Endosc Percutan Tech. 2019;29:271–274. doi: 10.1097/SLE.0000000000000673. [DOI] [PubMed] [Google Scholar]
- 7.Hawes RH, Zaidi S. Endoscopic ultrasonography of the pancreas. Gastrointest Endosc Clin N Am. 1995;5:61–80. [PubMed] [Google Scholar]
- 8.Kondo S, Isayama H, Akahane M, Toda N, Sasahira N, Nakai Y, et al. Detection of common bile duct stones: comparison between endoscopic ultrasonography, magnetic resonance cholangiography, and helical-computed-tomographic cholangiography. Eur J Radiol. 2005;54:271–275. doi: 10.1016/j.ejrad.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 9.Gariepy CE, Heyman MB, Lowe ME, Pohl JF, Werlin SL, Wilschanski M, et al. Causal evaluation of acute recurrent and chronic pancreatitis in children: consensus from the INSPPIRE group. J Pediatr Gastroenterol Nutr. 2017;64:95–103. doi: 10.1097/MPG.0000000000001446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kalmin B, Hoffman B, Hawes R, Romagnuolo J. Conventional versus Rosemont endoscopic ultrasound criteria for chronic pancreatitis: comparing interobserver reliability and intertest agreement. Can J Gastroenterol. 2011;25:261–264. doi: 10.1155/2011/302382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Attila T, Adler DG, Hilden K, Faigel DO. EUS in pediatric patients. Gastrointest Endosc. 2009;70:892–898. doi: 10.1016/j.gie.2009.04.012. [DOI] [PubMed] [Google Scholar]
- 12.Cohen S, Kalinin M, Yaron A, Givony S, Reif S, Santo E. Endoscopic ultrasonography in pediatric patients with gastrointestinal disorders. J Pediatr Gastroenterol Nutr. 2008;46:551–554. doi: 10.1097/MPG.0b013e31815ce571. [DOI] [PubMed] [Google Scholar]
- 13.Bjerring OS, Durup J, Qvist N, Mortensen MB. Impact of upper gastrointestinal endoscopic ultrasound in children. J Pediatr Gastroenterol Nutr. 2008;47:110–113. doi: 10.1097/MPG.0b013e31816c74af. [DOI] [PubMed] [Google Scholar]
- 14.Bizzarri B, Nervi G, Ghiselli A, Manzali E, Di Mario F, Leandro G, et al. Endoscopic ultrasound in pediatric population: a comprehensive review of the literature. Acta Biomed. 2018;89(9-S):33–39. doi: 10.23750/abm.v89i9-S.7876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Baran M, Appak YC, Tumgor G, Karakoyun M, Ozdemir T, Koyluoglu G. Etiology and outcome of cholelithiasis in Turkish children. Indian Pediatr. 2018;55:216–218. [PubMed] [Google Scholar]
- 16.De Castro VL, Moura EG, Chaves DM, Bernardo WM, Matuguma SE, Artifon EL. Endoscopic ultrasound versus magnetic resonance cholangiopancreatography in suspected choledocholithiasis: a systematic review. Endosc Ultrasound. 2016;5:118–128. doi: 10.4103/2303-9027.180476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.ASGE Standards of Practice Committee. Maple JT, Ben-Menachem T, Anderson MA, Appalaneni V, Banerjee S, et al. The role of endoscopy in the evaluation of suspected choledocholithiasis. Gastrointest Endosc. 2010;71:1–9. doi: 10.1016/j.gie.2009.09.041. [DOI] [PubMed] [Google Scholar]
- 18.Patel S, Marshak J, Daum F, Iqbal S. The emerging role of endoscopic ultrasound for pancreaticobiliary diseases in the pediatric population. World J Pediatr. 2017;13:300–306. doi: 10.1007/s12519-017-0020-y. [DOI] [PubMed] [Google Scholar]
- 19.Zakko SF. Overview of gallstone disease in adults [Internet] Waltham (MA): UpToDate, Inc.; 2020. [cited 2020 Feb 12]. Available from: https://www.uptodate.com/contents/overview-of-gallstone-disease-in-adults?search=endoscopic%20ultrasound&source=search_result&selectedTitle=15~150&usage_type=default&display_rank=15#H58361831. [Google Scholar]
- 20.Varadarajulu S, Wilcox CM, Eloubeidi MA. Impact of EUS in the evaluation of pancreaticobiliary disorders in children. Gastrointest Endosc. 2005;62:239–244. doi: 10.1016/s0016-5107(05)00312-3. [DOI] [PubMed] [Google Scholar]
- 21.Singh SK, Srivastava A, Rai P, Yachha SK, Poddar U. Yield of endoscopic ultrasound in children and adolescent with acute recurrent pancreatitis. J Pediatr Gastroenterol Nutr. 2018;66:461–465. doi: 10.1097/MPG.0000000000001855. [DOI] [PubMed] [Google Scholar]
- 22.Mahajan R, Simon EG, Chacko A, Reddy DV, Kalyan PR, Joseph AJ, et al. Endoscopic ultrasonography in pediatric patients: experience from a tertiary care center in India. Indian J Gastroenterol. 2016;35:14–19. doi: 10.1007/s12664-016-0619-2. [DOI] [PubMed] [Google Scholar]
- 23.Kadyada SP, Thapa BR, Dhaka N, Bhatia A, Menon J. Role of diagnostic endoscopic ultrasound in idiopathic acute pancreatitis and acute recurrent pancreatitis in children. Pancreas. 2019;48:350–355. doi: 10.1097/MPA.0000000000001243. [DOI] [PubMed] [Google Scholar]
- 24.Schwarzenberg SJ. Clinical manifestations and diagnosis of chronic and acute recurrent pancreatitis in children [Internet] Waltham (MA): UpToDate, Inc.; 2020. [cited 2020 Mar 17]. Available from: https://www.uptodate.com/contents/clinical-manifestations-and-diagnosis-of-chronic-and-acute-recurrent-pancreatitis-in-children?search=chronic%20pancreatitis&source=search_result&selectedTitle=2~142&usage_type=default&display_rank=2. [Google Scholar]
- 25.Anderloni A, Repici A. Role and timing of endoscopy in acute biliary pancreatitis. World J Gastroenterol. 2015;21:11205–11208. doi: 10.3748/wjg.v21.i40.11205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Anderloni A, Ballarè M, Pagliarulo M, Conte D, Galeazzi M, Orsello M, et al. Prospective evaluation of early endoscopic ultrasonography for triage in suspected choledocholithiasis: results from a large single centre series. Dig Liver Dis. 2014;46:335–339. doi: 10.1016/j.dld.2013.11.007. [DOI] [PubMed] [Google Scholar]
- 27.Kieling CO, Hallal C, Spessato CO, Ribeiro LM, Breyer H, Goldani HA, et al. Changing pattern of indications of endoscopic retrograde cholangiopancreatography in children and adolescents: a twelve-year experience. World J Pediatr. 2015;11:154–159. doi: 10.1007/s12519-014-0518-5. [DOI] [PubMed] [Google Scholar]
- 28.Ardengh JC, Malheiros CA, Rahal F, Pereira V, Ganc AJ. Microlithiasis of the gallbladder: role of endoscopic ultrasonography in patients with idiopathic acute pancreatitis. Rev Assoc Med Bras (1992) 2010;56:27–31. doi: 10.1590/s0104-42302010000100011. [DOI] [PubMed] [Google Scholar]
- 29.Al-Rashdan A, LeBlanc J, Sherman S, McHenry L, DeWitt J, Al-Haddad M. Role of endoscopic ultrasound for evaluating gastrointestinal tract disorders in pediatrics: a tertiary care center experience. J Pediatr Gastroenterol Nutr. 2010;51:718–722. doi: 10.1097/MPG.0b013e3181dac094. [DOI] [PubMed] [Google Scholar]