In little more than a year, the COVID-19 pandemic has reached every continent, causing 98 million confirmed cases and over 2 million deaths (as of Jan 25, 2021). Equally rapid has been the progress in vaccine development, with clinical trials commencing just months after the initial release of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) genome on Jan 10, 2020. At present, a number of vaccines are already licenced or progressing through phase 3 trials. Most use a recombinant spike glycoprotein: either mRNA based (the Moderna and Pfizer–BioNTech vaccines), via an adenovirus vector (the Oxford–AstraZeneca, CanSino, and Johnson & Johnson vaccines), or via injection of the protein itself (the Novavax vaccine). In tandem with rapid vaccine development, widespread whole genome sequencing (WGS) efforts have provided more than 360 000 SARS-CoV-2 sequences on the Global Initiative on Sharing All Influenza Data platform. This sequencing has allowed researchers to track the spread of different lineages globally. Some mutations in the virus appear to provide fitness advantages and facilitate quicker spread of particular lineages, such as the globally dispersed variant with a Asp614Gly spike substitution,1 and the recently described variant of concern 202012/01 (B.1.1.7) lineage in the UK.2 A number of studies have yielded insight into the relationship between SARS-CoV-2 genomic variability and the host immune response; in this Comment, we discuss whether such variability has the potential to affect the efficacy of recently developed vaccines.
Firstly, what can we learn from other viral vaccines? Many viral vaccines present the entire virus in a live-attenuated form (measles, mumps, rubella, varicella, rotavirus, Sabin oral poliovirus, yellow fever, and some influenza vaccines) or an inactivated form (Salk poliovirus, hepatitis A, rabies, and some other influenza vaccines), leading to a polyclonal response to not just one, but a number of viral proteins. This multiplicity of humoral and T cell responses probably explains why no convincing vaccine escape strains have been documented for these viruses. The exception to this is influenza virus, in which viral antigenic drift (mutations accumulating with time in the haemagglutinin and neuraminidase proteins) and antigenic shift or reassortment (recombination of these segments leads to a different combination of haemagglutinin and neuraminidase proteins) mean that the immune response to previous influenza strains (or vaccines) is no longer effective in preventing infection by the new strains. SARS-CoV-2 is non-segmented, and its mutation rate is lower than that of other RNA viruses. However, results from a 2020 preprint (yet to be peer-reviewed) examining convalescent plasma for other human coronaviruses, such as human coronavirus 229E, suggest that, similar to influenza, mutations to human coronavirus 229E with time might render individuals less able to neutralise new strains.3
A smaller number of recombinant viral vaccines are in use, more similar in approach to those recently licensed for SARS-CoV-2. The human papillomavirus vaccine uses a recombinant L1 protein that is genotype specific, but no evidence suggests that mutations for a particular L1 protein have rendered the vaccine less effective for a given genotype. As yet, no evidence for SARS-CoV-2 shows that genomic variability has led to the formation of antigenically distinct genotypes. The recombinant varicella zoster vaccine contains a glycoprotein E antigen that provides protection to all genotypes, but again no evidence shows that genetic variability has rendered the vaccine less effective. However, another recombinant vaccine is that for hepatitis B virus, which uses one of the viral envelope proteins, HBV surface antigen. Neutralising antibodies are targeted mainly to a 25 amino acid sequence, spanning amino acids 124 to 149. Point mutations that result in an arginine rather than glycine residue at position 145 in this sequence lead to a failure of vaccine-induced neutralising antibodies, and infections of vaccinated individuals.4 However, despite the description of viral strains with these mutations in different locations globally, they appear to occur sporadically, and perhaps due to reduced fitness compared with the wild type, they have not threatened the success of global immunisation campaigns.
From this overview, only data on influenza might suggest that evolution in SARS-CoV-2 could eventually lead to a less efficacious vaccine. A protective factor is the relatively low mutation rate of SARS-CoV-2, although prolonged infection in immunocompromised hosts might accelerate mutation.5 However, the length of the spike protein used by licensed vaccines is relatively short (∼1270 amino acids), and one preprint paper has indicated that the natural antibody response to infection (and presumably also to a spike protein-based vaccine) is concentrated in just two sections of the protein: the N-terminal domain (NTD) and receptor-binding domain (RBD).6
Given that the antibody response to the spike protein is so focused, could mutations in these restricted sequences lead to a less efficacious vaccine, if the human immune response is specific to the vaccine sequence? These mutations might be driven by antigenic drift, or by selection, either during natural infection or due to the vaccine itself. When a virus is grown under the selective pressure of a single monoclonal antibody that targets a single epitope on a viral protein, mutations in that protein sequence will lead to the loss of neutralisation, and the generation of escape mutants. This sequence of events has been shown in the laboratory for polio, measles, and respiratory syncytial virus,7 and in 2020 for SARS-CoV-2.8
Another notable finding is that SARS-CoV-2 passaged in the presence of polyclonal antibodies (in the form of convalescent sera) can also mutate and escape neutralisation by the multiple antibodies. In a series of experiments described in a 2020 preprint, SARS-CoV-2 was grown in the presence of neutralising COVID-19 convalescent plasma from a recovered patient.9 After serial passages, three mutations were generated (a deletion and insertion in the NTD loops, and a point substitution in the RBD) that allowed the newly formed variant to become completely resistant to plasma neutralisation. When this virus was grown in the presence of convalescent plasma from 20 other patients, all samples showed a reduction in neutralising activity. The RBD amino acid substitution selected for in this experiment, Glu484Lys, is at the same position as mutations reported in a preprint paper describing monoclonal antibody selection experiments (with the mutant variants also escaping neutralisation by convalescent human sera),10 and as that found in501Y.V2 (B.1.351), a SARS-CoV-2 variant spreading rapidly in South Africa.11 An orthogonal approach is to take different SARS-CoV-2 variants and examine whether patient sera shows variable effectiveness in neutralising the variants. Two preprints from South Africa show that the 501Y.V2 variant with Lys417Asn, Glu484Lys, and Asn501Tyr substitutions in the RBD, and Leu18Phe, Asp80Ala, Asp215Gly, 242–244del, and Arg246Ile in the NTD, is less susceptible to neutralisation by convalescent sera from individuals exposed to earlier variants, in either live virus or pseudovirus neutralisation assays.12, 13 One of these studies showed complete loss of neutralising activity in a high proportion of samples (21 [48%] of 44).13
In principle, these findings suggest that variants of SARS-CoV-2 could evolve with resistance to immunity induced by recombinant spike protein vaccines (which are based on the original sequence, Wuhan-Hu-1) in some people; however, the studies also have reassuring aspects. Responses to the spike protein vary between individuals: for example, the mutant generated after multiple passages in convalescent sera, EM188, showed wide variability in escaping the neutralising activity of sera from different patients, with some samples showing only a 2-fold reduction in activity.9 A study looking at neutralisation of a Lys417Asn, Glu484Lys, and Asn501Tyr pseudovirus by sera from vaccinated individuals found a 1–3-fold reduction in titres of neutralising antibody activity,14 in contrast to the larger reductions seen in the selection study,9 and with no individuals showing loss of neutralisation activity.14 Thus, sera from vaccinated individuals seems of low concern regarding neutralisation of virus variants, although further studies testing vaccinated sera across the range of licensed and candidate vaccines are warranted.
An unresolved question is the effect that the reported mutations might have on T cell immunity, which is known from vaccine trials to be robustly stimulated by the recombinant spike protein. T cell escape has been well described for persisting viruses such as HIV, HBV, and hepatitis C virus.15 Substitutions occurring in T cell epitopes have the potential to impair cytotoxic T lymphocyte or T helper recognition, which might lead to delayed elimination of infected cells, or suboptimal help provided to B cells and the antibody response. However, in contrast to neutralising antibody sequences, T cell epitopes are located along the full length of the spike protein.16 The degree to which T cells contribute to protective immunity against SARS-CoV-2 is not yet known. However, the polyclonal nature of the T cell response, with multiple regions of the spike protein targeted, would suggest a limited effect of viral mutations on cellular immunity.
So is there cause for concern? Clearly, variability in the spike glycoprotein can affect the efficiency of antibody neutralisation. The role of spike protein variability inT cell immunity is likely to be elucidated in experimental studies in the next few months; a priori, the enhanced repertoire of T cell epitopes makes the loss of cytotoxic activity or recognition improbable. But only ongoing clinical trials will show whether vaccinated individuals recognise SARS-CoV-2 variants differently, and whether mutations decrease vaccine protection in some vaccinated individuals. The ongoing phase 3 trial of an adenovirus-vectored spike-based vaccine (Johnson & Johnson, NCT04505722) in South Africa, where the 501Y.V2 (B.1.351) strain with the Glu484Lys substitution is rapidly replacing pre-existing variants,11 might provide an opportunity to examine this question. Ultimately, most vaccines are based on a recombinant spike protein sequence. Thus if evidence emerges that particular variants do appear to influence vaccine efficacy, it should be possible to periodically reformulate the vaccines so that they better match the circulating strains.
Importantly, the overall effectiveness of immunisation will correlate with rates of vaccine uptake. We therefore encourage researchers, health-care providers, and policy makers to act as advocates for immunisation, and to advise individuals with questions about vaccines to seek this information from reliable sources. The higher the proportion of a population vaccinated, the lower the number of susceptible individuals, and the fewer opportunities SARS-CoV-2 will have to spread and mutate.
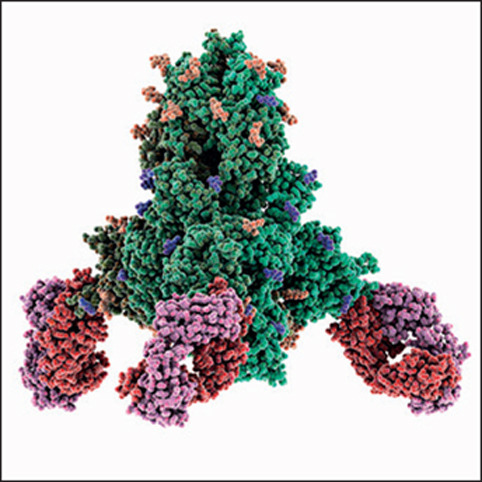
© 2021 Laguna Design/Science Photo Library
For the WHO COVID-19 Dashboard see covid19.who.int
Acknowledgments
We declare no competing interests. TCW is the recipient of a Wellcome Trust Award (204802/Z/16/Z). WAB is a senior fellow of the European and Developing Countries Clinical Trials Partnership 2 programme supported by the EU Horizon 2020 programme (grant number TMA2016SF-1535-CaTCH-22). We would like to thank Jesse Bloom for his reading of the text and insightful comments.
References
- 1.Korber B, Fischer WM, Gnanakaran S, et al. Tracking changes in SARS-CoV-2 spike: evidence that D614G increases infectivity of the COVID-19 virus. Cell. 2020;182:812–827.e19. doi: 10.1016/j.cell.2020.06.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Public Health England Investigation of novel SARS-CoV-2 variant. 2020. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/949639/Technical_Briefing_VOC202012-2_Briefing_2_FINAL.pdf
- 3.Eguia RD, Crawford KH, Stevens-Ayers T, et al. A human coronavirus evolves antigenically to escape antibody immunity. bioRxiv. 2020 doi: 10.1101/2020.12.17.423313. published online Dec 18. (preprint) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Romanò L, Paladini S, Galli C, Raimondo G, Pollicino T, Zanetti AR. Hepatitis B vaccination. Hum Vaccin Immunother. 2015;11:53–57. doi: 10.4161/hv.34306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Choi B, Choudhary MC, Regan J, et al. Persistence and evolution of SARS-CoV-2 in an immunocompromised host. N Engl J Med. 2020 doi: 10.1056/NEJMc2031364. published online Nov 11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Greaney AJ, Loes AN, Crawford KH, et al. Comprehensive mapping of mutations to the SARS-CoV-2 receptor-binding domain that affect recognition by polyclonal human serum antibodies. bioRxiv. 2021 doi: 10.1101/2020.12.31.425021. published online Jan 4. (preprint) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mas V, Nair H, Campbell H, Melero JA, Williams TC. Antigenic and sequence variability of the human respiratory syncytial virus F glycoprotein compared to related viruses in a comprehensive dataset. Vaccine. 2018;36:6660–6673. doi: 10.1016/j.vaccine.2018.09.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Weisblum Y, Schmidt F, Zhang F, et al. Escape from neutralizing antibodies by SARS-CoV-2 spike protein variants. eLife. 2020;9:1. doi: 10.7554/eLife.61312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Andreano E, Piccini G, Licastro D, et al. SARS-CoV-2 escape in vitro from a highly neutralizing COVID-19 convalescent plasma. bioRxiv. 2020 doi: 10.1101/2020.12.28.424451. published online Dec 28. (preprint) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu Z, VanBlargan LA, Rothlauf PW, et al. Landscape analysis of escape variants identifies SARS-CoV-2 spike mutations that attenuate monoclonal and serum antibody neutralization. bioRxiv. 2021 doi: 10.1101/2020.11.06.372037. published online Nov 8. (preprint) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tegally H, Wilkinson E, Giovanetti M, Iranzade A. Emergence and rapid spread of a new severe acute respiratory syndrome-related coronavirus 2 (SARS-CoV-2) lineage with multiple spike mutations in South Africa. medRxiv. 2020 doi: 10.1101/2020.12.21.20248640. published online Dec 22. (preprint) [DOI] [Google Scholar]
- 12.Cele S, Gazy I, Jackson L, et al. Escape of SARS-CoV-2 501Y.V2 variants from neutralization by convalescent plasma. Jan 21, 2021. https://www.ahri.org/wp-content/uploads/2021/01/MEDRXIV-2021-250224v1-Sigal.pdf [DOI] [PMC free article] [PubMed]
- 13.Wibmer CK, Ayres F, Hermanus T, et al. SARS-CoV-2 501Y.V2 escapes neutralization by South African COVID-19 donor plasma. bioRxiv. 2021 doi: 10.1101/2021.01.18.427166. published online Jan 19. (preprint) [DOI] [PubMed] [Google Scholar]
- 14.Wang Z, Schmidt F, Weisblum Y, et al. mRNA vaccine-elicited antibodies to SARS-CoV-2 and circulating variants. bioRxiv. 2021 doi: 10.1101/2021.01.15.426911. published online Jan 19. (preprint) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McMichael A. T cell responses and viral escape. Cell. 1998;93:673–676. doi: 10.1016/s0092-8674(00)81428-2. [DOI] [PubMed] [Google Scholar]
- 16.Mateus J, Grifoni A, Tarke A, et al. Selective and cross-reactive SARS-CoV-2 T cell epitopes in unexposed humans. Science. 2020;370:89–94. doi: 10.1126/science.abd3871. [DOI] [PMC free article] [PubMed] [Google Scholar]


