Abstract
Background
Mental disorders are related to high individual suffering and significant socio-economic burdens. However, it remains unclear to what extent self-reported mental distress is related to individuals’ days of incapacity to work and their medical costs. This study aims to investigate the impact of self-reported mental distress for specific and non-specific days of incapacity to work and specific and non-specific medical costs over a two-year span.
Method
Within a longitudinal research design, 2287 study participants’ mental distress was assessed using the Hospital Anxiety and Depression Scale (HADS). HADS scores were included as predictors in generalized linear models with a Tweedie distribution with log link function to predict participants’ days of incapacity to work and medical costs retrieved from their health insurance routine data during the following two-year period.
Results
Current mental distress was found to be significantly related to the number of specific days absent from work and medical costs. Compared to participants classified as no cases by the HADS (2.6 days), severe case participants showed 27.3-times as many specific days of incapacity to work in the first year (72 days) and 10.3-times as many days in the second year (44 days), and resulted in 11.4-times more medical costs in the first year (2272 EUR) and 6.2-times more in the second year (1319 EUR). The relationship of mental distress to non-specific days of incapacity to work and non-specific medical costs was also significant, but mainly driven from specific absent days and specific medical costs. Our results also indicate that the prevalence of presenteeism is considerably high: 42% of individuals continued to go to work despite severe mental distress.
Conclusions
Our results show that self-reported mental distress, assessed by the HADS, is highly related to the days of incapacity to work and medical costs in the two-year period. Reducing mental distress by improving preventive structures for at-risk populations and increasing access to evidence-based treatments for individuals with mental disorders might, therefore, pay for itself and could help to reduce public costs.
Keywords: Mental distress, Incapacity to work, Longitudinal study, Prevention and health promotion, Presenteeism
Background
Mental disorders are related to high individual suffering and a significantly reduced quality of life for those affected [1, 2]. In addition, they are related to significant socio-economic burdens worldwide [3–6]. Depression and anxiety disorders are ranked third and eighth among all diseases regarding the most years lived with disability (DALY) worldwide [5, 7]. About one in five people across industrialized countries and the world is suffering from a current mental disorder (18% Germany, 17.3% the EU, 18.9% the US, and 17.6% worldwide) [8, 9]. According to current forecasts, the economic burden of mental disorders will continue to increase in the coming years [10]; accordingly, it has been assumed that direct and indirect medical costs due to mental illness will more than double between 2010 and 2030 (factor 2.4) and that the global loss of economic output (loss of working days) will amount to $16.3 USD trillion during this period (2011–2030) [10, 11]. This global loss of economic output due to mental disorders is not only caused by increased absence days, but also by an increased prevalence of presenteeism. Presenteeism, which refers to attending work while ill [12] has been estimated to produce 4-times as many costs compared to being absent from work [13].
Therefore, recognizing and reducing mental distress is of central importance to society to reduce individual suffering and socio-economic burdens [14]. For doing so, individuals with mild or moderate mental distress should be given access to prevention services. In addition, individuals with severe mental distress or even mental illness should be given rapid access to specialized treatments and professional help. However, to date, mental distress or even mental illness are often detected and treated too late or not at all; only about one in five mentally ill people seek medical treatment (18.9% as 12-month prevalence) [15]. The treatment gap for mental disorders is universally large across countries [16]. For example, in a representative survey of the French population, 46.5% of participants with any type of mental disorder reported no lifetime use of mental health treatment (ranging from 35.6% for mood disorders to 56.7% for substance use disorders) [17]. Over time, mild mental distress can turn into severe mental distress – with its consequences for the duration of incapacity to work and sickness costs [18–21]. Indeed, previous studies have shown that subclinical symptoms in the general population are predictive of later mental disorders. Subclinical psychotic symptoms, for example, were studied early in the general population [22–24], with significant associations with progression to psychotic disorders [25, 26] but also with non-psychotic disorders [27, 28]. Further studies on other subclinical symptoms suggest that ‘sadness’ as a subclinical symptom is predictive of later major depressive disorder [29, 30].
Creating a low-threshold and rapid access to professional help requires financial investment. At the same time, when considering the reduction of days of incapacity to work and productivity losses, it could save money. Results from the English Improving Access to Psychological Therapies (IAPT; e.g., [31]) service in the UK have shown that increasing access to psychological therapies would largely pay for itself by reducing other depression and anxiety-related public costs (e.g., medical costs and productivity loss) and increasing revenues (e.g., paying taxes [32];). It has been suggested that mental health services from other countries might benefit from adopting this approach [33]. However, to the best of our knowledge, a detailed analysis of the socio-economic consequences of mental distress from other European countries in the general population is still lacking. This analysis is important in estimating the potential amount of money that could be saved by effective treatments and invested in improving services. Health insurers, politicians, employers, and other health care decision-makers should, therefore, be informed about the financial consequences of increased mental distress when thinking about implementing and improving preventive and curative structures to maintain and restore mental health [34].
Aim of the study
This study aims to examine the impact of different degrees of self-reported mental distress as expressed in terms of subclinical anxiety and depression levels on the number of specific (due to mental disorder and burnout) and non-specific (due to any diagnosis) days of incapacity to work (DIW) as well as specific and non-specific medical costs in a two-year period in Germany.
Method
Data from a passive control cohort of a large health promotion intervention study were used, which was conducted in 2013 and 2014 in 43 locations in Southern Germany [35–37]. The study has been registered in the German Register of Clinical Trials (DRKS) and was approved by the Ethics Review Committee at the University of Heidelberg, Germany (Study Registration: DRKS00006216). For this study, data collected in a longitudinal section were analyzed. At the beginning of the study (t0), the mental distress and the sample’s socio-demographic data were collected. The DIW data were analyzed with a latency of 1 and 2 years, respectively, starting after t0.
Sample
A total of 34,207 policyholders of a large German health insurance company were contacted, 5549 of whom declared their willingness to participate in the study. This corresponds to a response rate of 16%. The data could not be analyzed for 861 participants because (i) the questionnaire data was incomplete or DIW data was not available because of being insured with another health insurance company (n = 808), (ii) consent to participate in the study was withdrawn (n = 20), or (iii) the questionnaire was sent out twice (n = 23). The education variable “still in school” (n = 10) was excluded because the incomplete educational status could not be included in the ranking of the education factor. Of the remaining 4688 insured persons, 1329 insured persons were not included because they were not entitled to sickness benefits (e.g., pensioners, family insured persons, rehabilitates, voluntarily insured persons not entitled to sickness benefit), and 1072 because they belonged to the experimental group in the initial study. Finally, a total sample of 2287 study participants were included in the analyses. For details, see Lyssenko et al. [35].
Assessments
Mental distress
Cross-sectional mental distress was assessed with the Hospital Anxiety and Depression Scale (HADS) [38]. The HADS is a self-report questionnaire measuring anxiety and depressive symptoms with good psychometric properties [39]. The questionnaire consists of seven items for each of the two subscales, assessing the frequency of occurrence of respective symptoms on a four-point Likert-Scale, ranging from 0 = ‘not at all’ to 3 = ‘very often’. Total scores can be calculated for each subscale, ranging from 0 to 21 or an overall score for both subscales ranging from 0 to 42, which can be interpreted as a global screener of mental distress [40]. Higher values in the subscales indicate more severe anxiety or depressive symptoms. Based on the values in one of the two subscales, the degree of mental distress can be differentiated as no distress (0–7), mild distress (8–10), moderate distress (11–15), and severe mental distress (≥ 16) [41]. In addition, cut-off values are provided to distinguish between inconspicuous values and values requiring therapy. For the HADS, cut-off values apply to one of the two subscales of ≥8 (values ≥11 are considered conspicuous) [42, 43]. Therefore, a need for therapy should be clarified by further procedures, even at a low level of mental distress. A meta-analytic consideration showed an averaged sensitivity of 0.82 and specificity of 0.74 when applying a cut-off point of 8 and an averaged sensitivity of 0.56 and specificity of 0.92 when applying a cut-off point of 11 across different clinical samples [44]. In our sample, the HADS showed good reliability, with a Cronbach’s α of 0.91.
Days of incapacity to work
The number of specific and non-specific DIW was selected from all study participants’ routine health insurance data. As specific DIW, the days of incapacity to work due to mental illness were selected classified according to the following ICD-10 domains (International Statistical Classification of Diseases and Related Health Problems), F00-F99, “mental and behavioral disorders”, and ICD 10, Z73, “problems with regard to difficulties in coping with life”, including burnout. As non-specific DIW, all days of incapacity to work due to any ICD 10 diagnosis were selected. Both specific and non-specific DIW were retrieved cumulatively during the first and second year, starting on the day after the HADS assessment.
Medical costs
Direct specific and non-specific medical costs were retrieved from routine health insurance data for all study participants. The direct specific health care costs of the diagnostic main group “mental and behavioral disorders” (ICD 10, F00-F99) and “problems related to difficulties in coping with life” including burnout (Z73) were determined for the cost fields of outpatient treatment, hospital (main diagnosis), and rehabilitation (admission diagnosis). The drug costs were composed of the costs for antidepressants (N06A), psycholeptics, and psychoanaleptics in combination (N06C), anxiolytics (N05B), and hypnotics and sedatives (N05C). The averaged direct specific and non-specific medical costs are available in Euro and were retrieved cumulatively during the first and second year, starting on the day after the HADS assessment.
Socio-demographic data
The socio-demographic characteristics of the sample age, gender, and employment status were retrieved from the routine health insurance data. The questionnaires also assessed education and marital status.
Statistical analyses
Many individuals do not generate any medical costs and do not cause a single DIW. Therefore, health insurance costs and DIW data are usually not normally distributed, but represent a probability distribution, with a positive mass at zero (discrete distribution) and a continuous distribution above zero. This, so-called compound Poisson-gamma distribution belongs to the family of Tweedy distributions and can be modeled in generalized linear models [45–51].
Accordingly, instead of using analyses of covariance, which would be appropriate in the case of normally distributed outcome variables, a generalized linear model with a Tweedie distribution with log link function was calculated with mental distress (HADS) as an independent variable and the specific and non-specific DIW and medical costs in the first and second year after the HADS assessment as dependent variables. Since prior studies have shown an effect of socio-demographic variables on DIW [52–54], we included our sample’s socio-demographic variables as control variables in the model (age, gender, education, and relationship and employment status). By retrieving DIW and medical costs from the routine health insurance data, these data were complete for all participants over the two-year period, so there were no dropouts. The analyses were performed with SPSS 26 (Statistical Package for Social Sciences).
Results
The sample of 2287 participants consisted of 89% women and averaged 46.1 years of age (SD = 10.4). Most (72.4%) of the study participants were married. The percentage of participants holding an A-Level degree was 25.7%, whereas 2.5% had no school-leaving certificate. A small group of participants (0.5%) became unemployed by losing their job during the study period. Regarding mental distress, 47.6% of study participants were classified as no case, 24.1% were classified as a mild case, 23.5% were classified as moderate cases, and 4.7% were classified as severe cases, by applying the proposed cut-off values to their HADS scores. Socio-demographics of the sample are depicted in Table 1.
Table 1.
Socio-demographic characteristics of the sample (N = 2287)
| N | Percent | |
|---|---|---|
| Gender | ||
| Female | 2029 | 88.7% |
| Male | 258 | 11.3% |
| Age | ||
| 18–33 years | 366 | 16.0% |
| 34–49 years | 906 | 39.6% |
| 50–65 years | 1015 | 44.4% |
| Marital status | ||
| Married | 1655 | 72.4% |
| Not married | 632 | 27.6% |
| Years of school education | ||
| No school-leaving certificate | 57 | 2.5% |
| 9 years | 592 | 25.9% |
| 10 years | 1051 | 46.0% |
| 13 years (A-Level) | 587 | 25.7% |
| Employment Status | ||
| Employed | 2276 | 99.5% |
| Unemployed | 11 | 0.5% |
| Mental distress category (HADS) | ||
| No case | 1089 | 47.6% |
| Mild case | 552 | 24.1% |
| Moderate case | 538 | 23.5% |
| Severe case | 108 | 4.7% |
With 78% of all specific DIW due to mental illnesses and burnout, the diagnostic groups affective disorders (41%, e.g., depression) and neurotic, stress, and somatoform disorders (37%, e.g., anxiety disorders) dominate in the sample. None of the other diagnostic groups from the “mental and behavioral disorders” or burnout showed a proportion above 9% (i.e., 8% substance-related disorders, 7% personality disorders, 3% schizophrenia spectrum disorders, 2% problems related to difficulties in coping with life incl. Burnout, 2% behavioral syndromes associated with physiological disturbances and physical factors [e.g., eating disorders], 1% mental disorders due to known physiological conditions [e.g., dementia]).
However, 79.6% of our sample had no specific DIW in the 2 years that followed the HADS testing. Based on the sample’s HADS scores, the percentage of participants who did not have any specific DIW was 89% for no cases, 82% for mild cases, 66% for moderate cases, and 42% for severe cases. Regarding non-specific DIW, 21% of our sample had no non-specific DIW in the following 2 years. Based on the sample’s HADS scores, the percentage of participants who did not have any non-specific DIW was 27% for no cases, 20% for mild cases, 13% for moderate cases, and still 8% for severe cases.
Regarding specific (non-specific) medical costs, the proportion without any costs depending on the HADS scores was 51.1% (1.0%) for no cases, 38.9% (0.4%) for mild cases, 19.9% (0.0%) for moderate cases, and 8.3% (0.9%) for severe cases.
Impact of socio-demographic variables
Gender
Gender revealed no significant differences in non-specific and specific DIW in the first and second years (Tables 2 and 3). Accordingly, no differences in non-specific medical costs were obtained between male and female participants (Table 4). However, specific medical costs were significantly increased for female participants in the second year (Table 5). Compared to men, female participants showed 1.2-times as many specific medical costs (χ2[1] = 2.60, p = .107) in the first year and 1.4-times as many specific medical costs (χ2[1] = 8.51, p = .004) in the second year.
Table 2.
Results from the generalized linear model to predict the non-specific days of incapacity to work (due to any diagnosis) by self-reported mental distress, controlled for socio-demographic characteristics of the sample
| Non-specific DIW in the first year | Non-specific DIW in the second year | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | 95% CI | Exp(B) | 95% CI | p-value | M | 95% CI | Exp(B) | 95% CI | p-value | |||||
| Constant | 6.44 | 4.95 | 8.38 | < .001 | 6.39 | 4.85 | 8.41 | < .001 | ||||||
| Gender | ||||||||||||||
| Malea | 32.2 | 22.9 | 45.4 | 1.00 | 22.5 | 15.2 | 33.2 | 1.00 | ||||||
| Female | 37.8 | 27.8 | 51.6 | 1.17 | 0.97 | 1.42 | .093 | 27.2 | 19.0 | 39.1 | 1.21 | 1.00 | 1.47 | .052 |
| Age groups | ||||||||||||||
| 18–33 yearsa | 28.4 | 20.1 | 40.2 | 1.00 | 21.0 | 14.2 | 31.2 | 1.00 | ||||||
| 34–49 years | 35.0 | 25.4 | 48.2 | 1.23 | 1.03 | 1.48 | .026 | 22.8 | 15.7 | 33.0 | 1.08 | 0.89 | 1.31 | .412 |
| 50–65 years | 42.8 | 31.4 | 58.5 | 1.51 | 1.26 | 1.81 | < .001 | 31.6 | 22.0 | 45.4 | 1.51 | 1.25 | 1.82 | < .001 |
| Marital status | ||||||||||||||
| Marrieda | 33.0 | 24.1 | 45.1 | 1.00 | 23.2 | 16.2 | 33.4 | 1.00 | ||||||
| Not married | 37.0 | 26.8 | 51.1 | 1.12 | 0.99 | 1.27 | .072 | 26.3 | 18.1 | 38.2 | 1.13 | 0.99 | 1.29 | .065 |
| Years of school education | ||||||||||||||
| 13 years (A-Level)a | 25.1 | 18.1 | 34.9 | 1.00 | 16.5 | 11.3 | 24.2 | 1.00 | ||||||
| 10 years | 30.3 | 22.1 | 41.5 | 1.21 | 1.04 | 1.40 | .016 | 20.7 | 14.3 | 30.1 | 1.23 | 1.07 | 1.47 | .005 |
| 9 years | 37.9 | 27.5 | 52.2 | 1.51 | 1.23 | 1.79 | < .001 | 29.6 | 20.3 | 43.0 | 1.79 | 1.50 | 2.13 | < .001 |
| No school-leaving certificate | 51.7 | 34.2 | 78.1 | 2.06 | 1.50 | 2.83 | < .001 | 36.9 | 23.6 | 57.7 | 2.23 | 1.59 | 3.13 | < .001 |
| Employment Status | ||||||||||||||
| Employeda | 27.9 | 24.6 | 31.5 | 1.00 | 24.9 | 21.9 | 28.3 | 1.00 | ||||||
| Unemployed | 43.8 | 24.0 | 79.9 | 1.57 | 0.86 | 2.87 | .143 | 24.6 | 12.1 | 49.8 | 0.99 | 0.48 | 2.02 | .973 |
| Mental distress category (HADS) | ||||||||||||||
| No casea | 15.8 | 11.4 | 22.1 | 1.00 | 13.1 | 9.0 | 19.1 | 1.00 | ||||||
| Mild case | 25.8 | 18.4 | 36.2 | 1.63 | 1.40 | 1.90 | < .001 | 19.1 | 13.0 | 28.0 | 1.46 | 1.25 | 1.70 | < .001 |
| Moderate case | 44.7 | 32.2 | 61.9 | 2.82 | 2.45 | 3.25 | < .001 | 30.6 | 21.1 | 44.3 | 2.34 | 2.02 | 2.71 | < .001 |
| Severe case | 81.4 | 58.0 | 114.3 | 5.14 | 4.11 | 6.41 | < .001 | 48.9 | 32.7 | 73.0 | 3.73 | 2.95 | 4.72 | < .001 |
Note. N = 2.287. t0 Assessment of predictor variables. M Mean days of incapacity to work, CI 95% confidence interval, HADS Hospital Anxiety and Depression Scale. areference category. Method = log-link function, Tweedie-distribution of residuals
Table 3.
Results from the generalized linear model to predict the specific days of incapacity to work (due to mental illness) by self-reported mental distress, controlled for socio-demographic characteristics of the sample
| Specific DIW in the first year | Specific DIW in the second year | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | 95% CI | Exp(B) | 95% CI | p-value | M | 95% CI | Exp(B) | 95% CI | p-value | |||||
| Constant | 0.78 | 0.36 | 1.69 | .533 | 1.25 | 0.58 | 2.69 | .567 | ||||||
| Gender | ||||||||||||||
| Malea | 11.2 | 5.1 | 24.5 | 1.00 | 10.2 | 4.4 | 23.3 | 1.00 | ||||||
| Female | 17.5 | 9.1 | 33.9 | 1.57 | 0.91 | 2.69 | .373 | 15.1 | 7.4 | 30.9 | 1.48 | 0.87 | 2.52 | .147 |
| Age groups | ||||||||||||||
| 18–33 yearsa | 11.1 | 5.0 | 24.5 | 1.00 | 11.3 | 4.9 | 26.1 | 1.00 | ||||||
| 34–49 years | 16.3 | 8.1 | 32.5 | 1.47 | 0.89 | 2.41 | .129 | 11.5 | 5.4 | 24.5 | 1.01 | 0.62 | 1.65 | .964 |
| 50–65 years | 15.2 | 7.7 | 29.7 | 1.37 | 0.83 | 2.26 | .221 | 14.6 | 7.1 | 30.0 | 1.29 | 0.79 | 2.09 | .309 |
| Marital status | ||||||||||||||
| Marrieda | 14.2 | 7.2 | 28.1 | 1.00 | 11.2 | 5.4 | 23.4 | 1.00 | ||||||
| Not married | 13.7 | 6.8 | 27.9 | 0.96 | 0.68 | 1.36 | .835 | 13.6 | 6.4 | 29.2 | 1.22 | 0.87 | 1.70 | .258 |
| Years of school education | ||||||||||||||
| 13 years (A-Level)a | 10.8 | 5.2 | 22.6 | 1.00 | 7.3 | 3.3 | 16.1 | 1.00 | ||||||
| 10 years | 13.1 | 6.7 | 25.8 | 1.21 | 0.80 | 1.83 | .360 | 10.2 | 4.8 | 21.7 | 1.41 | 0.92 | 2.15 | .114 |
| 9 years | 12.1 | 6.0 | 24.6 | 1.12 | 0.70 | 1.79 | .636 | 13.1 | 6.0 | 28.4 | 1.80 | 1.13 | 2.85 | .013 |
| No school-leaving certificate | 22.1 | 8.7 | 56.5 | 2.04 | 0.93 | 4.48 | .074 | 24.2 | 9.5 | 61.6 | 3.32 | 1.51 | 7.28 | .003 |
| Employment Status | ||||||||||||||
| Employeda | 8.4 | 6.0 | 11.7 | 1.00 | 9.0 | 6.5 | 12.5 | 1.00 | ||||||
| Unemployed | 23.4 | 6.6 | 82.5 | 2.80 | 0.80 | 9.86 | .108 | 17.0 | 4.2 | 68.0 | 1.88 | 0.46 | 7.59 | .377 |
| Mental distress category (HADS) | ||||||||||||||
| No casea | 2.6 | 1.2 | 5.6 | 1.00 | 4.3 | 2.0 | 9.3 | 1.00 | ||||||
| Mild case | 7.4 | 3.5 | 15.8 | 2.83 | 1.78 | 4.49 | < .001 | 6.2 | 2.8 | 14.0 | 1.46 | 0.94 | 2.28 | .095 |
| Moderate case | 27.5 | 13.6 | 55.9 | 10.50 | 7.04 | 15.67 | < .001 | 20.1 | 9.5 | 42.4 | 4.71 | 3.21 | 6.90 | < .001 |
| Severe case | 71.5 | 34.7 | 147.1 | 27.26 | 15.79 | 47.07 | < .001 | 43.9 | 19.5 | 99.0 | 10.29 | 5.97 | 17.72 | < .001 |
Note. N = 2.287. t0 Assessment of predictor variables. M Mean days of incapacity to work, CI 95% confidence interval, HADS Hospital Anxiety and Depression Scale. areference category. Method = log-link function, Tweedie-distribution of residuals
Table 4.
Results from the generalized linear model to predict the direct non-specific medical costs (EUR) by self-reported mental distress, controlled for socio-demographic characteristics of the sample
| Non-specific costs in the first year | Non-specific costs in the second year | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | 95% CI | Exp(B) | 95% CI | p-value | M | 95% CI | Exp(B) | 95% CI | p-value | |||||
| Constant | 1217.15 | 1016.57 | 1457.31 | < .001 | 1302.23 | 1082.57 | 1566.46 | < .001 | ||||||
| Gender | ||||||||||||||
| Malea | 2799.9 | 2174.8 | 3604.7 | 1.00 | 3142.1 | 2415.0 | 4088.0 | 1.00 | ||||||
| Female | 3191.1 | 2527.0 | 4029.9 | 1.14 | 1.00 | 1.30 | .053 | 3207.3 | 2507.0 | 4103.3 | 1.02 | 0.89 | 1.17 | .761 |
| Age groups | ||||||||||||||
| 18–33 yearsa | 2682.3 | 2078.7 | 3461.0 | 1.00 | 2760.1 | 2111.1 | 3608.7 | 1.00 | ||||||
| 34–49 years | 3008.9 | 2370.6 | 3819.0 | 1.12 | 0.99 | 1.27 | .072 | 3099.7 | 2413.6 | 3980.9 | 1.12 | 0.98 | 1.28 | .083 |
| 50–65 years | 3309.2 | 2613.7 | 4189.8 | 1.23 | 1.09 | 1.40 | .001 | 3739.3 | 2917.0 | 4793.3 | 1.35 | 1.19 | 1.54 | < .001 |
| Marital status | ||||||||||||||
| Marrieda | 2947.5 | 2330.6 | 3727.7 | 1.00 | 3055.6 | 2387.9 | 3909.9 | 1.00 | ||||||
| Not married | 3031.3 | 2380.1 | 3860.7 | 1.03 | 0.94 | 1.13 | .545 | 3298.1 | 2557.3 | 4253.5 | 1.08 | 0.98 | 1.19 | .108 |
| Years of school education | ||||||||||||||
| 13 years (A-Level)a | 3059.7 | 2401.1 | 3899.0 | 1.00 | 2833.3 | 2193.2 | 3660.3 | 1.00 | ||||||
| 10 years | 2870.0 | 2267.9 | 3632.0 | 0.94 | 0.85 | 1.04 | .221 | 2609.4 | 2033.0 | 3349.1 | 0.92 | 0.83 | 1.03 | .131 |
| 9 years | 3123.5 | 2466.3 | 3955.8 | 1.02 | 0.91 | 1.15 | .731 | 3620.8 | 2822.6 | 4644.8 | 1.28 | 1.13 | 1.44 | < .001 |
| No school-leaving certificate | 2910.6 | 2099.8 | 4034.4 | 0.95 | 0.73 | 1.23 | .707 | 3793.8 | 2732.5 | 5267.5 | 1.34 | 1.04 | 1.73 | .024 |
| Employment Status | ||||||||||||||
| Employeda | 2111.4 | 1923.4 | 2317.9 | 1.00 | 2474.8 | 2253.9 | 2717.2 | 1.00 | ||||||
| Unemployed | 4231.7 | 2693.3 | 6648.7 | 2.00 | 1.27 | 3.16 | .003 | 4072.2 | 2522.1 | 6574.8 | 1.65 | 1.01 | 2.67 | .044 |
| Mental distress category (HADS) | ||||||||||||||
| No casea | 2031.0 | 1588.2 | 2597.4 | 1.00 | 2259.5 | 1744.5 | 2926.6 | 1.00 | ||||||
| Mild case | 2329.7 | 1810.8 | 2997.2 | 1.15 | 1.03 | 1.27 | .010 | 2635.1 | 2024.0 | 3430.7 | 1.17 | 1.05 | 1.30 | .005 |
| Moderate case | 3048.4 | 2389.3 | 3889.4 | 1.50 | 1.36 | 1.66 | < .001 | 3292.0 | 2546.0 | 4256.6 | 1.46 | 1.31 | 1.62 | < .001 |
| Severe case | 5543.7 | 4273.8 | 7167.5 | 2.73 | 2.30 | 3.23 | < .001 | 5181.3 | 3952.3 | 6792.3 | 2.29 | 1.92 | 2.74 | < .001 |
Note. N = 2.287. t0 Assessment of predictor variables, M Mean non-specific direct costs in Euro per person and year, CI 95% confidence interval, HADS Hospital Anxiety and Depression Scale. areference category. Method = log-link function, Tweedie-distribution of residuals
Table 5.
Results from the generalized linear model to predict the direct specific medical costs (EUR) by self-reported mental distress, controlled for socio-demographic characteristics of the sample
| Specific costs in the first year | Specific costs in the second year | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | 95% CI | Exp(B) | 95% CI | p-value | M | 95% CI | Exp(B) | 95% CI | p-value | |||||
| Constant | 93.72 | 67.94 | 129.28 | < .001 | 132.74 | 96.86 | 181.92 | < .001 | ||||||
| Gender | ||||||||||||||
| Malea | 595.4 | 395.2 | 897.1 | 1.00 | 397.7 | 259.9 | 608.6 | 1.00 | ||||||
| Female | 721.4 | 395.2 | 897.1 | 1.21 | 0.96 | 1.53 | .107 | 564.9 | 384.7 | 608.6 | 1.42 | 1.12 | 1.80 | .004 |
| Age groups | ||||||||||||||
| 18–33 yearsa | 687.6 | 458.6 | 1030.8 | 1.00 | 464.9 | 304.7 | 709.4 | 1.00 | ||||||
| 34–49 years | 641.7 | 439.5 | 937.0 | 0.93 | 0.76 | 1.15 | .515 | 444.9 | 298.7 | 662.6 | 0.96 | 0.78 | 1.17 | .673 |
| 50–65 years | 638.0 | 443.2 | 918.6 | 0.93 | 0.75 | 1.14 | .484 | 514.8 | 349.6 | 758.1 | 1.11 | 0.90 | 1.36 | .330 |
| Marital status | ||||||||||||||
| Marrieda | 531.9 | 367.8 | 769.2 | 1.00 | 414.7 | 280.7 | 612.7 | 1.00 | ||||||
| Not married | 807.5 | 552.8 | 1179.6 | 1.52 | 1.31 | 1.76 | < .001 | 541.7 | 363.4 | 807.5 | 1.31 | 1.13 | 1.52 | < .001 |
| Years of school education | ||||||||||||||
| 13 years (A-Level)a | 492.3 | 334.1 | 725.4 | 1.00 | 474.3 | 315.0 | 714.1 | 1.00 | ||||||
| 10 years | 648.7 | 449.0 | 937.3 | 1.89 | 1.04 | 1.40 | .001 | 487.7 | 328.0 | 725.1 | 1.03 | 0.87 | 1.22 | .753 |
| 9 years | 619.4 | 423.4 | 906.2 | 1.26 | 1.23 | 1.79 | .029 | 541.4 | 360.9 | 812.2 | 1.14 | 0.94 | 1.39 | .187 |
| No school-leaving certificate | 932.6 | 573.7 | 1516.1 | 1.32 | 1.10 | 1.58 | .003 | 403.0 | 238.8 | 680.2 | 0.85 | 0.55 | 1.31 | .464 |
| Employment Status | ||||||||||||||
| Employeda | 531.1 | 458.9 | 614.7 | 1.00 | 409.7 | 350.6 | 478.7 | 1.00 | ||||||
| Unemployed | 808.7 | 402.3 | 1625.8 | 1.52 | 0.76 | 3.05 | .234 | 548.4 | 259.3 | 1159.7 | 1.34 | 0.63 | 2.85 | .448 |
| Mental distress category (HADS) | ||||||||||||||
| No casea | 199.0 | 134.8 | 293.9 | 1.00 | 213.1 | 142.2 | 319.5 | 1.00 | ||||||
| Mild case | 433.6 | 291.8 | 644.3 | 2.18 | 1.80 | 2.64 | < .001 | 271.6 | 179.0 | 412.2 | 1.27 | 1.06 | 1.53 | .010 |
| Moderate case | 940.9 | 647.1 | 1368.0 | 4.73 | 3.97 | 5.63 | < .001 | 661.1 | 445.5 | 980.9 | 3.10 | 2.63 | 3.66 | < .001 |
| Severe case | 2272.3 | 1521.0 | 3394.6 | 11.42 | 8.90 | 14.66 | < .001 | 1318.9 | 858.7 | 2026.0 | 6.19 | 4.79 | 7.99 | < .001 |
Note. N = 2.287. t0 assessment of predictor variables, M Mean specific direct costs in Euro per person and year, CI 95% confidence interval, HADS Hospital Anxiety and Depression Scale. areference category. Method = log-link function, Tweedie-distribution of residuals
Age
Compared to 18–33-year-old participants, older participants showed significantly increased non-specific DIW in the first year (χ2[2] = 22.54, p < .001, factor 1.2 to 1.5) and the second year (χ2[2] = 31.86, p < .001, 1.1 to 1.5). This increase of non-specific DIW was not driven by higher specific DIW (first year: χ2[2] = 2.31, p = .315; second year: χ2[2] = 2.23, p = .328). Accordingly, older participants showed significantly higher non-specific medical costs in the first year (χ2[2]) = 11.68, p = .003) and second year (χ2[2] = 26.83, p < .001), but no significant differences in specific medical costs.
Marital status
Marital status revealed no significant differences in non-specific and specific DIW in the first or second years. Accordingly, no differences in non-specific medical costs were obtained between married and unmarried participants. The specific medical costs, however, were significantly increased in unmarried participants both in the first year (χ2[1] = 30.56, p < .001, factor 1.5) and the second year (χ2[1] = 12.51, p < .001, factor 1.3).
Education
Lower educated participants showed a significant increase in non-specific DIW. Compared to participants holding an A-Level degree, lower educated participants showed 1.2 to 2.2 as many non-specific DIW in the first (χ2[3] = 33.59, p < .001) and in the second year (χ2[3] = 54.60, p < .001). The number of specific DIW was also increased for lower educated participants, however, this only yielding significance in the second year. Lower educated participants showed in the first year 1.2 to 2.0 as many specific DIW (χ2[3] = 3.46, p = .326) and in the second year 1.4 to 3.3 as many specific DIW (χ2[3] = 11.22, p = .011). Regarding the medical costs, no differences were obtained on non-specific costs in the first year, but an increase was shown in non-specific medical costs for lower educated participants in the second year (χ2[3] = 43.12, p < .001). An opposite pattern was found concerning specific costs. Here, lower educated participants showed increased costs in the first year (χ2[3] = 14.56, p = .002) but not in the second year.
Employment status
Employment status revealed no significant differences in non-specific and specific DIW in the first and second years. However, the non-specific costs of unemployed participants were significantly increased. Compared to employed participants, unemployed participants showed 2.0-times as many non-specific medical costs (χ2[1] = 8.99, p < .003) in the first year and 1.7-times as many non-specific medical costs (χ2[1] = 4.07, p = .044) in the second year. Specific medical costs of unemployed participants were descriptively increased (1.3 to 1.5), but this was not significant.
Impact of self-reported mental distress
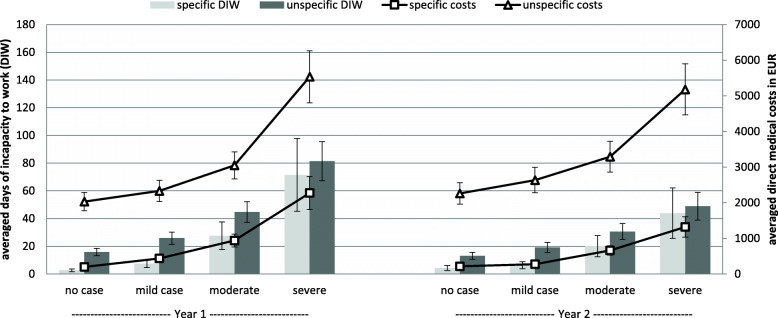
The impact of HADS severity scores on specific and non-specific DIW and medical costs in the first and second years after HADS assessment is depicted in Fig. 1.
Fig. 1.
Mean scores of specific and non-specific days of incapacity to work (DIW) on the left y-axis and specific and non-specific medical costs (MC) on the right y-axis in the first and second year after HADS assessment, depending on the HADS severity score. Specific = DIW or MC due to mental illness. Non-specific = DIW or MC due to all diagnoses. Results are controlled for age, gender, marital status, education, and employment status. Error bars represent standard errors
Days of incapacity to work
Mental distress, as measured with the HADS at t0, showed a significant effect on the number of non-specific DIW in the first year (χ2[3] = 320.78, p < .001; see Table 2) and the second year (χ2[3] = 195.17, p < .001). The number of non-specific DIW increased continuously with the degree of mental distress. While participants classified as no cases averaged 15.8 non-specific DIW in the first year (13.1 in the second year), mild case participants averaged 1.6 (1.5) times as many non-specific DIW (M = 25.8 days in the first year and M = 19.1 days in the second year), moderate case participants averaged 2.8 (2.3) times as many non-specific DIW (M = 44.7 days in the first year and M = 30.6 days in the second year), and severe case participants averaged 5.1 (3.7) times as many non-specific DIW (M = 81.4 days in the first year and 48.9 days in the second year).
This increase of non-specific DIW was mainly driven by an increase of specific DIW in the first year (χ2[3] = 196.98, p < .001) and the second year (χ2[3] = 106.21, p < .001; see Table 3). While participants, classified as no cases averaged 2.6 specific DIW in the first year (4.3 in the second year), mild case participants averaged 2.8 (1.5) times as many specific DIW (M = 7.4 days in the first and M = 6.2 days in the second year), moderate case participants averaged 10.5 (4.7) times as many specific DIW (M = 27.5 days in the first and M = 20.1 days in the second year), and severe case participants averaged 27.3 (10.3) times as many specific DIW (M = 71.5 days in the first and M = 43.9 days in the second year).
The increases of DIW in the first and second years were obtained on both the anxiety and depression subscales (all p values < .001).
Medical costs
The increase of DIW depending on mental distress was also reflected in higher non-specific medical costs in the first year (χ2[3] = 164.41, p < .001; see Table 4) and the second year (χ2[3] = 110.45, p < .001). Again, the number of non-specific medical costs increased continuously according to the degree of mental distress: While participants classified as no cases averaged 2031 EUR non-specific medical costs in the first year (2260 EUR in the second year), mild case participants had 1.2 (1.2) times as many non-specific medical costs (M = 2330 EUR in the first year and M = 2635 EUR in the second year); moderate case participants had 1.5 (1.5) times as many non-specific medical costs (M = 3048 EUR in the first and M = 3292 EUR in the second year); and severe case participants had 2.7 (1.9) times as many non-specific medical costs (M = 5544 EUR in the first and M = 5181 EUR in the second year).
The increase of non-specific medical costs was again mainly driven by an increase of specific medical costs in the first year (χ2[3] = 496.56, p < 0.001; see Table 5) and the second year (χ2[3] = 309.45, p < .001). While participants classified as no cases averaged 199 EUR specific medical costs in the first year (213 EUR in the second year), mild case participants had 2.2 (1.3) times as many specific medical costs (M = 434 EUR in the first and M = 272 EUR in the second year); moderate case participants had 4.7 (3.1) times as many specific medical costs (M = 941 EUR in the first and M = 661 EUR in the second year); and severe case participants had 11.4 (6.2) times as many specific medical costs (M = 2272 EUR in the first and 1319 EUR in the second year).
The increases in medical costs in the first and second years were obtained on both the anxiety and depression subscales (all p values < .001).
Discussion
This study aimed to examine the impact of self-reported mental distress, assessed by the HADS, on the number of specific and non-specific DIW and medical costs in the 2 years following the testing. To address this aim, we conducted a longitudinal study, in which the HADS scores of 2287 participants were used to predict their specific and non-specific DIW and medical costs in the first and second years after HADS assessment.
Our results revealed that self-reported mental distress (HADS scores) was significantly related to the number of non-specific DIW in the first and second years. Accordingly, the number of non-specific DIW increased continuously based on the level of mental distress. Compared to the reference group classified as no cases, severe cases had 5.1-times as many non-specific DIW in the first year and 3.7-times as many non-specific DIW in the second year. Not surprisingly, the increase of non-specific DIW was mainly driven by a significant increase of specific DIW. Compared to the no cases, severe cases showed 27.3-times as many specific DIW in the first year and 10.3-times as many specific DIW in the second year.
These results demonstrate that mental distress impacts a person’s life for several years by predicting their sickness absence rates even 2 years later. This increased sickness absence rate might be, in turn, related to a generally reduced social and occupational functioning levels and reduced well-being of individuals [55]. Furthermore, mental distress appears to be a central challenge for employers in terms of productivity loss. The financial consequences of specific DIW due to production loss can be calculated by multiplying the specific DIW by average income. Regarding average costs due to production loss in 2014 of 105 EUR per DIW [56], the averaged additional costs for an employee under severe mental distress due to absenteeism alone amount to 7230 EUR in the first years and 4163 EUR in the second year, compared to an employee without mental distress. According to prior empirical findings, the additional costs due to presenteeism can be estimated to be four times higher [53]. Our results revealed that 66% of participants classified as moderate cases and 42% of participants classified as severe cases, did not have any specific DIW in the two-year period that was analyzed. These results indicate that the percentage of people who go to work despite severe mental distress might be considerably high and illustrate the importance and spread of presenteeism. Given this high prevalence of presenteeism and the assumed adverse mental health outcomes, future studies should characterize this sub-sample’s environmental context (e.g. country, cultural norms), work related variables (e.g. job insecurity, strict attendance policies), psychological and personal factors (e.g. consciousness, perfectionism) as well as socio-demographic characteristics (e.g. gender, educational level) to better understand the risk factors of presenteeism [12, 57–59]. By doing so, a distinction should be made between whether work characteristics are perceived as resources and thus contribute to the stabilization of mental health, or as stressors that lead to the maintenance of high mental distress [60].
Both the anxiety and depression subscales of the HADS were predictive for specific and non-specific DIW. This is not surprising since 78% of all specific DIW due to mental illness and burnout in our sample were caused by the diagnostic groups affective disorders (41%, e.g., depression) and neurotic, stress and somatoform disorders (37%, e.g., anxiety disorders). This roughly corresponds to results from other studies in Germany, in which 88.6% of all specific DIW resulted from affective (41.4%) or neurotic, stress, and somatoform disorders (47.2%) [54]. Accordingly, it seems plausible that both the anxiety and depression subscale of the HADS predicted the number of specific DIW in our analyses. However, the impact of both HADS subscales for non-specific DIW is in contrast to the results of Schneider et al. [52], in which only the anxiety symptoms, but not the depressive symptoms, were found to be a significant predictor of the duration of absences due to non-specific DIW.
Beyond non-specific and specific DIW, our results demonstrated that mental distress is also significantly related to individuals’ specific and non-specific medical costs in the first and second year. Specific costs in the first year were 11.4-times higher for severe cases, compared to no cases. Even in the second year, severe cases showed 6.2-times as many specific costs as no cases. This amounts to an additional average specific cost of 2073 EUR per person and year for severe cases in the first year and 1106 EUR per person and year in the second year for the public health care system. The predictive effect of non-specific costs was considerably smaller, but also significant. Compared to no cases, severe cases averaged 2.7-times the costs in the first and 1.9-times the costs in the second year. This amounts to additional average non-specific costs of 3513 EUR per person and year for severe cases in the first year and 2922 EUR per person and year in the second year for the public health care system. The significant relationship between mental distress and non-specific medical costs was mainly driven by specific medical costs. However, these results also imply that subclinical psychiatric symptoms are associated with non-psychiatric medical outcomes. This finding is consistent with other research indicating, for example, an association between psychotic symptoms and diabetes [61], loneliness and venous thromboembolic events [62], or depressive symptoms and blood pressure levels [63].
These results underline the socio-economic burden of mental distress for public health care systems. However, they also show that this burden can be predicted by self-reported mental distress at an early stage. This result is consistent with previous studies, which have identified subclinical symptoms in the general population as predictive for later mental disorders [21–29]. There is rising evidence for the importance of subclinical symptoms to recognize possible mental burden at an early stage and opening the possibility of prevention.
Although our data represent costs from a German population, these results can be seen as an indicator for other industrialized countries, since both the prevalence of mental disorders (Germany 18%, EU 17.3%) and the percentage of direct and indirect medical costs due to mental illness in Germany (Germany 4.8%, EU 4.0%) are comparable to other EU countries [9].
Most demographic characteristics of our sample showed no consistent effects across the different dependent variables. However, these have been included mainly as control variables to control possible confounding variables. Future studies should specifically focus on these variables to draw reliable conclusions about socio-demographic variables’ influence on absence days and medical costs. Only the participants’ age showed a consistent pattern with increased non-specific DIW and non-specific medical costs for both years, but no differences in specific DIW and specific medical costs. Lower education in our sample was significantly related to non-specific DIW. However, on specific DIW, the increase by lower education yielded significance only in the second year. These results are in line with prior studies showing that mental distress (anxiety symptoms), higher age, and lower education emerged as significant predictors of non-specific DIW [52]. Given these findings, it seems likely that lower educational status and higher age can be considered a risk factor for non-specific DIW. However, their effect on specific DIW or medical costs remains uncertain. Future studies should include large and representative samples to investigate the differential effects of age and education on specific and non-specific DIW and specific and non-specific medical costs.
Contrary to prior studies, in which female gender was found to be a significant predictor of specific DIW [53, 54], our analyses showed no differences of specific DIW between male and female participants. However, a closer look at the descriptive factors shows that the factors from our study (1.57) are comparable to those from previous studies (1.6) [53, 54]. Therefore, the non-significant differences in DIW depending on the sample characteristics in our study could result from a too-small sample size in the different subgroups, thus limiting the power for individual comparisons. With 89%, the proportion of female participants was considerably high. Interestingly, female participants showed higher specific medical costs in both years. This finding is in line with prior research, indicating a higher prevalence of anxiety and affective mental disorders in female populations [9, 64].
Strengths, limitations, and recommendations for future research
Our study’s major strengths relate to its longitudinal research design and the analysis of real DIW and medical cost data from a health insurance company in conjunction with psychometrically assessed mental distress from individuals. By including DIW and medical costs in the first and second year, we were able to show that self-reported mental distress was predictive for DIW and medical costs regardless of the DIW and medical costs occurring immediately after the HADS assessment, and this enabled us to show the long-term consequences of severe mental distress. By including specific and non-specific DIW and specific and non-specific costs as dependent variables, we were able to show the importance of mental health for general, occupational functioning and point to the consequences of mental distress for companies and the public health care systems. Furthermore, the available cut-off scores of the HADS to distinguish between no, mild, moderate, and severe cases allowed us to demonstrate clear, practical implications for the consequences of severe mental distress in applied settings. However, this study has some limitations, which should be considered when interpreting the results.
Firstly, we only investigated the main effects of the sample characteristics and mental distress. However, more complex interaction effects between the independent variables are conceivable and should be investigated in future studies using larger sample sizes. Secondly, although our total sample was reasonably large, it is not a representative sample of the German population. Accordingly, we have included sociodemographic variables including sex, age groups, employment status, education and marital status in the models. However, some socio-demographic subgroups might be too small, resulting in limited power to retrieve reliable conclusions about the effect of different sample characteristics on DIW and medical costs, respectively (e.g., n = 11 participants in the unemployment group). Third, in addition to the sample characteristics analyzed in this study, other variables might impact the relationship between mental distress and DIW, such as the quality of health management in organizations [65], subjectively perceived workplace characteristics (e.g., social support, leadership quality [66, 67]), or inter-individual differences in psychological conditions, such as self-efficacy or work attitude [68]. In addition, variables should be investigated, influencing the relationship between mental distress and medical costs, such as access to psychotherapy or stigmatization. Finally, we analyzed DIW and medical costs independently of each other. Given possible confounding factors between those dependent variables, a multivariate analysis would have been appropriate to control for these dependencies. However, due to the Tweedie distributions of both the cost and DIW data, which represents a serious deviation from the normal distribution, the prerequisite for a multivariate analysis was not given. The use of general linear models allowed us to model Tweedie distributions. Future studies should investigate how medical costs and DIW are related to each other over time (e.g., whether increased specific medical costs help reduce DIW). Future studies should also systematically investigate how prevention programs for distressed individuals and evidence-based treatments for individuals with mental disorders contribute to saving money by restoring occupational and social functioning.
Implications for practice
This study shows the extent to which self-reported mental distress is related to the subsequent inability to work and to medical costs. On an individual level, our results indicate that mental distress affects a person’s life after a span of 2 years by reducing occupational and social functioning. On a societal level, our results demonstrate the high socio-economic costs of mental distress through productivity losses due to reduced functional levels. The results, therefore, suggest that joint efforts should be made to effectively reduce mental distress [69]. Individuals with mild and moderate mental distress who do not yet suffer from a manifested mental illness should be given access to preventive services [70]. Preventive structures should be established within peoples’ everyday lives (e.g., at the workplace) to enable low-threshold access [15, 16]. Workplace health promotion programs play a special role here because occupational risk factors, such as emotional load or work-related stress, can contribute critically to increased mental distress, which often manifests itself in anxiety and depression symptoms as well as burnout conditions [71, 72]. This also refers to the importance of occupational health surveillance for the monitoring and early prevention of mental distress, since not recognizing mental distress, ignoring it, or not taking effective countermeasures might exacerbate the problem and result in significant negative financial impact [19, 20, 34, 73]. A preventive commitment from employers to the workforce’s mental health should ultimately lead to a better working atmosphere, a better quality of life for employees, and an increase in productivity [11].
Individuals with severe mental distress or those with manifested mental disorders should be given rapid access to specialized help in the form of evidence-based psychotherapeutic or psychiatric treatments [31]. Prior studies from the UK have shown that increasing access to psychological therapies would largely pay for itself by reducing other depression and anxiety-related public costs (e.g., medical costs and productivity loss) and increasing revenues (e.g., paying taxes [32]). Rapid access to mental health services should be enabled, since the time spent waiting to start psychological treatments was negatively associated with treatment outcome [31].
Conclusion
In summary, our study demonstrates the extent to which mental distress is associated with reduced occupational and social functioning. Accordingly, mental distress significantly impacts the number of DIW and medical costs for a span of 2 years following the initial HADS assessment. These results indicate that improving preventive structures for at-risk populations and increasing access to specialized treatments for individuals with mental disorders might reduce individual suffering as well as public costs.
Acknowledgements
Not applicable.
Abbreviations
- DIW
Days of Incapacity to Work
- HADS
Hospital Anxiety and Depression Scale
- EUR
Euro
- DALY
Disability Adjusted Life Years
- EU
European Union
- US
United States
- USD
US Dollar
- IAPT
English Improving Access to Psychological Therapies
- UK
United Kingdom
- DRKS
Deutsches Register Klinischer Studien (German Register of Clinical Studies)
- ICD
International Statistical Classification of Diseases and Related Health Problems
- SPSS
Statistical Package for Social Science
Authors’ contributions
GM, LL, MBoh and NK designed the study. LL, GM and RV collected the data. GM analyzed the data and discussed the results with RV. MBom and MHG provided statistical advice. GM and RV prepared the first draft of the manuscript. All authors reviewed the manuscript. The author(s) read and approved the final manuscript.
Funding
This study was financed by the health insurance fund AOK Baden-Württemberg. The compilation of health care costs directly from the insurance fund’s records required a close cooperation throughout all phases of the project. In order to ensure scientific objectivity and simultaneously comply with the data protection policy, the sponsor commissioned an internal research officer (GM) and signed a contractual agreement with the research facility (CIMH Mannheim) that all data may be published regardless of possible positive or negative results.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due to the data protection policy from the cooperating insurance fund but are available from the corresponding author on reasonable request (in anonymized form).
Declarations
Ethics approval and consent to participate
This study was approved by the ethical review committee at the University of Heidelberg (2013620NMA). Written informed consent to participate in the study was obtained from participants.
Consent for publication
Not applicable, no individual data.
Competing interests
G. Mueller and M. Bombana are employees of the sponsor. The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Spitzer RL, Kroenke K, Linzer M, Hahn SR, Williams JBW, Degruy FV, et al. Health-related quality of life in primary care patients with mental disorders: results from the PRIME-MD 1000 study. Jama. 1995;274:1511–1517. doi: 10.1001/jama.1995.03530190025030. [DOI] [PubMed] [Google Scholar]
- 2.Alonso J, Angermeyer MC, Bernert S, Bruffaerts R, Brugha TS, et al. Disability and quality of life impact of mental disorders in Europe: results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatr Scand. 2004;109:38–46. [DOI] [PubMed]
- 3.Statistisches Bundesamt [Federal Statistical Office of Germany]. Krankheitskostenrechnung [disease-related cost accounts]. www.gbe-bund.de. Accessed 27 Apr 2020.
- 4.World Health Organization WHO. Mental health: facing the challenges, building solutions: report from the WHO European Ministerial Conference: WHO Regional Office Europe; 2005.
- 5.Vos T, Barber RM, Bell B, Bertozzi-Villa A, Biryukov S, Bolliger I, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the global burden of disease study 2013. Lancet. 2015;386:743–800. doi: 10.1016/S0140-6736(15)60692-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Patel V, Saxena S, Lund C, Thornicroft G, Baingana F, Bolton P, et al. The lancet commission on global mental health and sustainable development. Lancet. 2018;392:1553–98. [DOI] [PubMed]
- 7.James SL, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet. 2018;392:1789–1858. doi: 10.1016/S0140-6736(18)32279-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Steel Z, Marnane C, Iranpour C, Chey T, Jackson JW, Patel V, et al. The global prevalence of common mental disorders: a systematic review and meta-analysis 1980-2013. Int J Epidemiol. 2014;43:476–93. [DOI] [PMC free article] [PubMed]
- 9.OECD. Health at a Glance: Europe 2018: State of Health in the EU Cycle. Paris, France: OECD Publishing; 2018. 10.1787/health_glance_eur-2018-en. Accessed 10 Jul 2020. [DOI]
- 10.Bloom DE, Cafiero E, Jané-Llopis E, Abrahams-Gessel S, Bloom LR, Fathima S, et al. The global economic burden of noncommunicable diseases. Geneva: World Economic Forum; 2011. http://www3.weforum.org/docs/WEF_Harvard_HE_GlobalEconomicBurdenNonCommunicableDiseases_2011.pdf. Accessed 22 Apr 2020.
- 11.Eaton J, Qureshi O, Salaria N, Ryan G. The Lancet Commission on Mental Health and Sustainable Development: Evidence for action on mental health and global development. Mental Health Innovation Network, Centre for Global Mental Health, London, UK: London School of Hygiene and Tropical Medicine; 2018. https://globalmentalhealthcommission.org/wp-content/uploads/2018/10/Lancet-Commission_policy-brief_MHIN2.pdf.pdf. Accessed 4 Aug 2020.
- 12.Johns G. Presenteeism in the workplace: a review and research agenda. J Organ Behav. 2010;31:519–542. doi: 10.1002/job.630. [DOI] [Google Scholar]
- 13.Goetzel RZ, Long SR, Ozminkowski RJ, Hawkins K, Wang S, Lynch W. Health, absence, disability, and presenteeism cost estimates of certain physical and mental health conditions affecting US employers. J Occup Environ Med. 2004;46:398–412. doi: 10.1097/01.jom.0000121151.40413.bd. [DOI] [PubMed] [Google Scholar]
- 14.Campion J, Bhui K, Bhugra D. European psychiatric association (EPA) guidance on prevention of mental disorders. Eur Psychiatry. 2012;27:68–80. doi: 10.1016/j.eurpsy.2011.10.004. [DOI] [PubMed] [Google Scholar]
- 15.Mack S, Jacobi F, Gerschler A, Strehle J, Höfler M, Busch MA, et al. Self-reported utilization of mental health services in the adult German population–evidence for unmet needs? Results of the DEGS1-mental health module (DEGS1-MH) Int J Methods Psychiatr Res. 2014;23:289–303. doi: 10.1002/mpr.1438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kohn R, Saxena S, Levav I, Saraceno B. The treatment gap in mental health care. Bull World Health Organ. 2004;82:858–866. [PMC free article] [PubMed] [Google Scholar]
- 17.Font H, Roelandt J-L, Behal H, Geoffroy P-A, Pignon B, Amad A, et al. Prevalence and predictors of no lifetime utilization of mental health treatment among people with mental disorders in France: findings from the ‘mental health in general population’(MHGP) survey. Soc Psychiatry Psychiatr Epidemiol. 2018;53:567–576. doi: 10.1007/s00127-018-1507-0. [DOI] [PubMed] [Google Scholar]
- 18.Ekman M, Granström O, Omérov S, Jacob J, Landén M. The societal cost of depression: evidence from 10,000 Swedish patients in psychiatric care. J Affect Disord. 2013;150:790–797. doi: 10.1016/j.jad.2013.03.003. [DOI] [PubMed] [Google Scholar]
- 19.Hakanen JJ, Schaufeli WB, Ahola K. A three-year cross-lagged panel study on the job demands-resources model: do home demands and resources play a role. Work Stress. 2008;22:224–241. doi: 10.1080/02678370802379432. [DOI] [Google Scholar]
- 20.Guthier C, Dormann C, Voelkle MC. Reciprocal effects between job stressors and burnout: a continuous time meta-analysis of longitudinal studies. Psychol Bull. 2020;146:1146. doi: 10.1037/bul0000304. [DOI] [PubMed] [Google Scholar]
- 21.Bijl RV, de Graaf R, Hiripi E, Kessler RC, Kohn R, Offord DR, et al. The prevalence of treated and untreated mental disorders in five countries. Health Aff. 2003;22:122–133. doi: 10.1377/hlthaff.22.3.122. [DOI] [PubMed] [Google Scholar]
- 22.Strauss JS. Hallucinations and delusions as points on continua function: rating scale evidence. Arch Gen Psychiatry. 1969;21:581–586. doi: 10.1001/archpsyc.1969.01740230069010. [DOI] [PubMed] [Google Scholar]
- 23.van Os J, Hanssen M, Bijl RV, Ravelli A. Strauss (1969) revisited: a psychosis continuum in the general population? Schizophr Res. 2000;45:11–20. doi: 10.1016/S0920-9964(99)00224-8. [DOI] [PubMed] [Google Scholar]
- 24.Verdoux H, van Os J. Psychotic symptoms in non-clinical populations and the continuum of psychosis. Schizophr Res. 2002;54:59–65. doi: 10.1016/S0920-9964(01)00352-8. [DOI] [PubMed] [Google Scholar]
- 25.Poulton R, Caspi A, Moffitt TE, Cannon M, Murray R, Harrington H. Children’s self-reported psychotic symptoms and adult schizophreniform disorder: a 15-year longitudinal study. Arch Gen Psychiatry. 2000;57:1053–1058. doi: 10.1001/archpsyc.57.11.1053. [DOI] [PubMed] [Google Scholar]
- 26.Hanssen M, Bak M, Bijl R, Vollebergh W, van Os J. The incidence and outcome of subclinical psychotic experiences in the general population. Br J Clin Psychol. 2005;44:181–191. doi: 10.1348/014466505X29611. [DOI] [PubMed] [Google Scholar]
- 27.Pignon B, Schürhoff F, Szöke A, Geoffroy PA, Jardri R, Roelandt J-L, et al. Sociodemographic and clinical correlates of psychotic symptoms in the general population: findings from the MHGP survey. Schizophr Res. 2018;193:336–342. doi: 10.1016/j.schres.2017.06.053. [DOI] [PubMed] [Google Scholar]
- 28.Bourgin J, Tebeka S, Mallet J, Mazer N, Dubertret C, Le Strat Y. Prevalence and correlates of psychotic-like experiences in the general population. Schizophr Res. 2020;215:371–377. doi: 10.1016/j.schres.2019.08.024. [DOI] [PubMed] [Google Scholar]
- 29.Tebeka S, Pignon B, Amad A, Le Strat Y, Brichant-Petitjean C, Thomas P, et al. A study in the general population about sadness to disentangle the continuum from well-being to depressive disorders. J Affect Disord. 2018;226:66–71. doi: 10.1016/j.jad.2017.08.085. [DOI] [PubMed] [Google Scholar]
- 30.Tebeka S, Geoffroy PA, Dubertret C, Le Strat Y. Sadness and the continuum from well-being to depressive disorder: findings from a representative US population sample. J Psychiatr Res. 2020;132:50–54. doi: 10.1016/j.jpsychires.2020.10.004. [DOI] [PubMed] [Google Scholar]
- 31.Clark DM, Canvin L, Green J, Layard R, Pilling S, Janecka M. Transparency about the outcomes of mental health services (IAPT approach): an analysis of public data. Lancet. 2018;391:679–686. doi: 10.1016/S0140-6736(17)32133-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Laynard R, Clark D, Knapp M, Mayraz G. Cost-benefit analysis of psychological therapy. Natl Inst Econ Rev. 2007;202:90–98. doi: 10.1177/0027950107086171. [DOI] [Google Scholar]
- 33.Clark DM. Realizing the mass public benefit of evidence-based psychological therapies: the IAPT program. Annu Rev Clin Psychol. 2018;14:159–83. [DOI] [PMC free article] [PubMed]
- 34.Chirico F, Heponiemi T, Pavlova M, Zaffina S, Magnavita N. Psychosocial risk prevention in a global occupational health perspective. A descriptive analysis. Int J Environ Res Public Health. 2019;16:2470. doi: 10.3390/ijerph16142470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lyssenko L, Muller G, Kleindienst N, Schmahl C, Berger M, Eifert G, et al. Life balance - a mindfulness-based mental health promotion program: conceptualization, implementation, compliance and user satisfaction in a field setting. BMC Public Health. 2015;15:740. [DOI] [PMC free article] [PubMed]
- 36.Lyssenko L, Müller G, Kleindienst N, Schmahl C, Berger M, Eifert G, et al. Effectiveness of a mindfulness-based mental health promotion program provided by health coaches: a controlled multisite field trial. Psychother Psychosom. 2016;85:375–377. doi: 10.1159/000447012. [DOI] [PubMed] [Google Scholar]
- 37.Müller G, Pfinder M, Schmahl C, Bohus M, Lyssenko L. Cost-effectiveness of a mindfulness-based universal mental health promotion program. BMC Public Health. 2019;19:1309. [DOI] [PMC free article] [PubMed]
- 38.Herrmann-Lingen C, Buss U, Snaith P. Hospital Anxiety and Depression Scale-Deutsche Version (HADS-D): Huber. 2011. [Google Scholar]
- 39.Bjelland I, Dahl AA, Haug TT, Neckelmann D. The validity of the hospital anxiety and depression scale: an updated literature review. J Psychosom Res. 2002;52:69–77. doi: 10.1016/S0022-3999(01)00296-3. [DOI] [PubMed] [Google Scholar]
- 40.Spinhoven PH, Ormel J, Sloekers PPA, Kempen G, Speckens AE, van Hemert AM. A validation study of the hospital anxiety and depression scale (HADS) in different groups of Dutch subjects. Psychol Med. 1997;27:363–370. doi: 10.1017/S0033291796004382. [DOI] [PubMed] [Google Scholar]
- 41.Snaith RP, Zigmond AS. The hospital Anxiey and depression scale with the irritability-depression-anxiety scale and the Leeds situational anxiety scale. Windsor: NFER Nelson; 1994.
- 42.Hinz A, Brähler E. Normative values for the hospital anxiety and depression scale (HADS) in the general German population. J Psychosom Res. 2011;71:74–78. doi: 10.1016/j.jpsychores.2011.01.005. [DOI] [PubMed] [Google Scholar]
- 43.Geue K, Strauß B, Brähler E. Diagnostische Verfahren in der Psychotherapie [Diagnostic procedures in psychotherapy]: Göttingen, Germany: Hogrefe Verlag GmbH & Co. KG; 2016.
- 44.Brennan C, Worrall-Davies A, McMillan D, Gilbody S, House A. The hospital anxiety and depression scale: a diagnostic meta-analysis of case-finding ability. J Psychosom Res. 2010;69:371–378. doi: 10.1016/j.jpsychores.2010.04.006. [DOI] [PubMed] [Google Scholar]
- 45.Hasan MM, Dunn PK. Two Tweedie distributions that are near-optimal for modelling monthly rainfall in Australia. Int J Climatol. 2011;31:1389–1397. doi: 10.1002/joc.2162. [DOI] [Google Scholar]
- 46.König U, Heinzel-Gutenbrunner M, Meinlschmidt G, Maier W, Bachmann CJ. Einfluss des sozioökonomischen Status auf Gesundheitskosten für Kinder und Jugendliche mit Störungen des Sozialverhaltens: Eine Analyse von Routinedaten einer gesetzlichen Krankenversicherung [Socioeconomic status and health insurance expenditures for children and adolescents with conduct disorder: An analysis of statutory health insurance data]. Bundesgesundheitsblatt Gesundheitsforschung Gesundheitsschutz. 2019;62:1057–66. [DOI] [PubMed]
- 47.Bonat WH, Jørgensen B, Kokonendji CC, Hinde J, Demétrio CGB. Extended Poisson–Tweedie: properties and regression models for count data. Stat Model. 2018;18:24–49. doi: 10.1177/1471082X17715718. [DOI] [Google Scholar]
- 48.Kurz CF. Tweedie distributions for fitting semicontinuous health care utilization cost data. BMC Med Res Methodol. 2017;17:171. doi: 10.1186/s12874-017-0445-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zavras D. Testing the dual-state-process assumption in the preventive care services use. J Health Soc Sci. 2020;5:127–140. [Google Scholar]
- 50.Nelder J, Wedderburn R. Generalized Linear Models. J R Stat Soc. 1972;135:370–84.
- 51.McCullagh P, Nelder J. Generalized linear models (2nd ed). Boca Raton: Chapman and Hall; 1989.
- 52.Schneider A, Hilbert S, Hamann J, Skadsem S, Glaser J, Löwe B, et al. The implications of psychological symptoms for length of sick leave. Dtsch Arztebl Int. 2017;114:291–7. [DOI] [PMC free article] [PubMed]
- 53.Rennert D, Kliner K, Richter, M. Arbeitsunfähigkeit [Incapacity to work], In: Knieps F, Pfaff H, editors. Psychische Gesundheit und Arbeit: Zahlen, Daten, Fakten [Mental health and work: figures, data, facts]. Berlin, Germany: MWV Medizinisch Wissenschaftliche Verlagsgesellschaft mbH & Co. KG; 2019. p. 55–150.
- 54.DAK Psychoreport. Entwicklung der psychischen Erkrankungen im Job: Langzeitanalyse 1997-2018 [Development of mental illness in the workplace: long-term analysis 1997-2018]; 2019. https://www.dak.de/dak/bundesthemen/dak-psychoreport-2019-dreimal-mehr-fehltage-als-1997-2125486.html. Accessed 20 Jul 2020.
- 55.Hannula JA, Lahtela K, Järvikoski AK, Salminen J, Mäkelä P. Occupational functioning scale (OFS)–an instrument for assessment of work ability in psychiatric disorders. Nordic J Psychiatry. 2006;60:372–378. doi: 10.1080/08039480600937140. [DOI] [PubMed] [Google Scholar]
- 56.Bundesanstalt für für Arbeitsschutz und Arbeitsmedizin [German Federal Institute for Occupational Safety and Health]. Sicherheit und Gesundheit bei der Arbeit 2014: Unfallverhütungsbericht Arbeit [Safety and health at work 2014: Accident prevention report on work]; Bönen, Germany: Druck & Verlag Kettler GmbH; 2014. https://www.baua.de/DE/Angebote/Publikationen/Berichte/Suga-2014.pdf?__blob=publicationFile&v=17. Accessed 12 Jul 2020.
- 57.Kwon MJ. Occupational health inequalities by issues on gender and social class in labor market: absenteeism and Presenteeism across 26 OECD countries. Front Public Health. 2020;8:84. doi: 10.3389/fpubh.2020.00084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lohaus D, Habermann W. Presenteeism: a review and research directions. Hum Resour Manag Rev. 2019;29:43–58. doi: 10.1016/j.hrmr.2018.02.010. [DOI] [Google Scholar]
- 59.Robertson I, Leach D, Doerner N, Smeed M. Poor health but not absent: prevalence, predictors, and outcomes of presenteeism. J Occup Environ Med. 2012;54:1344–1349. doi: 10.1097/JOM.0b013e31825dff4b. [DOI] [PubMed] [Google Scholar]
- 60.Lohaus D, Habermann W, Kertoubi IE, Röser F. Working while ill is not always bad–positive effects of Presenteeism. Front Psychol. 2020;11:4059. doi: 10.3389/fpsyg.2020.620918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Nuevo R, Chatterji S, Fraguas D, Verdes E, Naidoo N, Arango C, Ayuso-Mateos JL. Increased risk of diabetes mellitus among persons with psychotic symptoms: results from the WHO world health survey. J Clin Psychiatry. 2011;72:1592–1599. doi: 10.4088/JCP.10m06801. [DOI] [PubMed] [Google Scholar]
- 62.Enga KF, Brækkan SK, Hansen-Krone IJ, Hansen J-B. Emotional states and future risk of venous thromboembolism. Thromb Haemost. 2012;107:485–493. doi: 10.1160/TH11-09-0667. [DOI] [PubMed] [Google Scholar]
- 63.Vallée A, Wiernik E, Kab S, Lemogne C, Goldberg M, Zins M, Blacher J. Association of depressive symptoms and socioeconomic status in determination of blood pressure levels and hypertension: the CONSTANCES population based study. J Affect Disord. 2020;279:282–291. doi: 10.1016/j.jad.2020.10.018. [DOI] [PubMed] [Google Scholar]
- 64.Seedat S, Scott KM, Angermeyer MC, Berglund P, Bromet EJ, Brugha TS, et al. Cross-national associations between gender and mental disorders in the World Health Organization world mental health surveys. Arch Gen Psychiatry. 2009;66:785–795. doi: 10.1001/archgenpsychiatry.2009.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Cullen KL, Irvin E, Collie A, Clay F, Gensby U, Jennings PA, et al. Effectiveness of workplace interventions in return-to-work for musculoskeletal, pain-related and mental health conditions: an update of the evidence and messages for practitioners. J Occup Rehabil. 2018;28:1–15. doi: 10.1007/s10926-016-9690-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lysaght RM, Larmour-Trode S. An exploration of social support as a factor in the return-to-work process. Work. 2008;30:255–266. [PubMed] [Google Scholar]
- 67.Aas RW, Ellingsen KL, Lindøe P, Möller A. Leadership qualities in the return to work process: a content analysis. J Occup Rehabil. 2008;18:335. doi: 10.1007/s10926-008-9147-y. [DOI] [PubMed] [Google Scholar]
- 68.Brouwer S, Reneman MF, Bültmann U, der Klink V, Jac JL, Groothoff JW. A prospective study of return to work across health conditions: perceived work attitude, self-efficacy and perceived social support. J Occup Rehabil. 2010;20:104–112. doi: 10.1007/s10926-009-9214-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Saxena S, Jané-Llopis EVA, Hosman C. Prevention of mental and behavioural disorders: implications for policy and practice. World Psychiatry. 2006;5:5. [PMC free article] [PubMed] [Google Scholar]
- 70.World Health Organization. Prevention and promotion in mental health. Geneva, Switzerland: World Health Organization; 2002. https://apps.who.int/iris/bitstream/handle/10665/42539/9241562161.pdf. Accessed 14 Jul 2020.
- 71.Chirico F. Is burnout a syndrome or an occupational disease? Instructions for occupational physicians. Epidemiologia e prevenzione. 2017;41:294. doi: 10.19191/EP17.5-6.P294.089. [DOI] [PubMed] [Google Scholar]
- 72.Chirico F. The forgotten realm of the new and emerging psychosocial risk factors. J Occup Health. 2017;59:433–435. doi: 10.1539/joh.17-0111-OP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Magnavita N. Medical surveillance, continuous health promotion and a participatory intervention in a small company. Int J Environ Res Public Health. 2018;15:662. doi: 10.3390/ijerph15040662. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analyzed during the current study are not publicly available due to the data protection policy from the cooperating insurance fund but are available from the corresponding author on reasonable request (in anonymized form).