Figure 2.
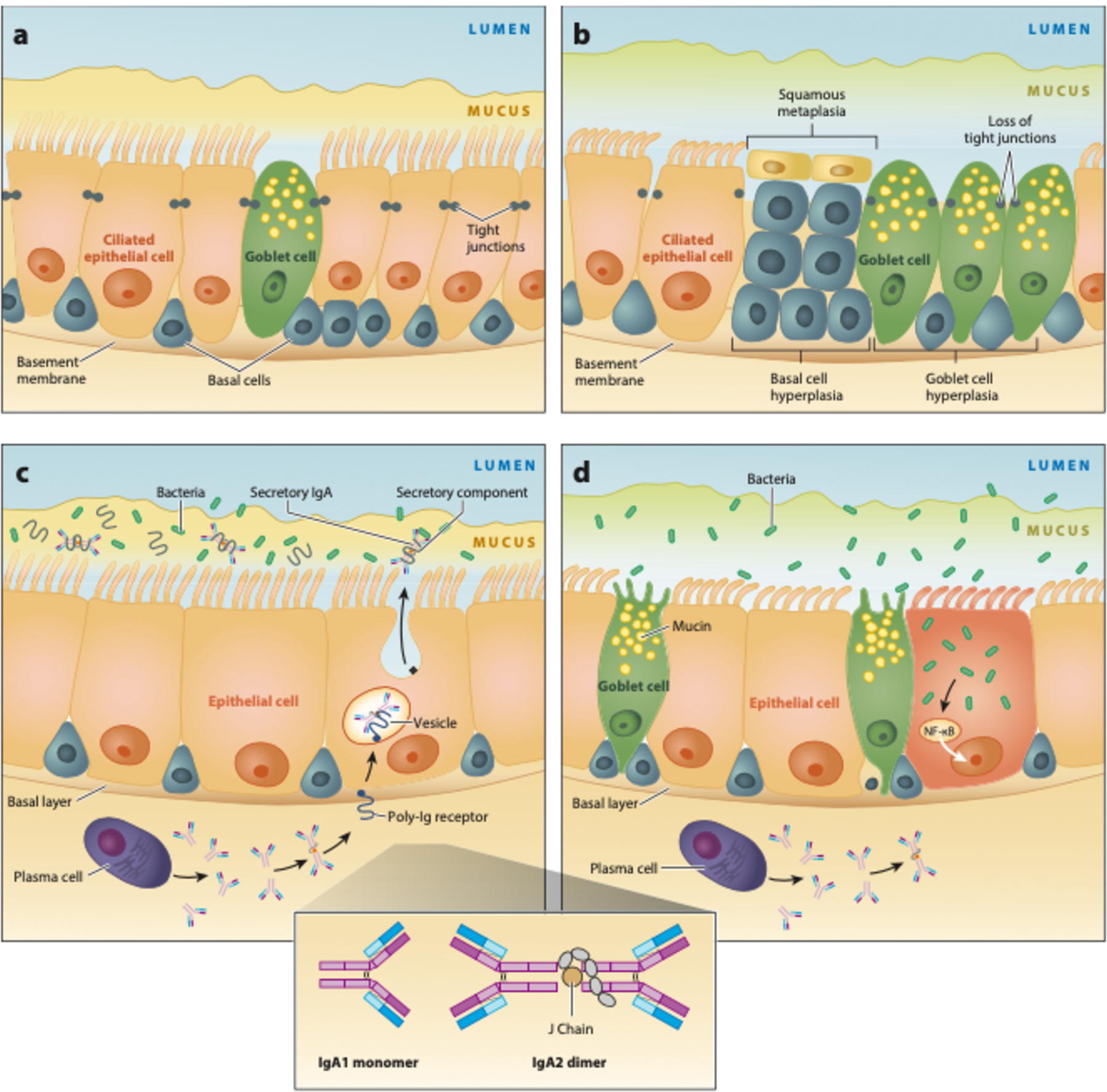
Small airway damage induced by epigenetic changes in chronic obstructive pulmonary disease (COPD). (a) Normal distal respiratory epithelium. Its self-renewing basal cells differentiate into ciliated and mucus-producing goblet cells, which are joined by tight junctions forming an impermeable barrier. Mucus is separated from the epithelial surface by an aqueous periciliary layer. (b) Smoking-related abnormalities: basal and goblet cell hyperplasia, squamous metaplasia, loss of ciliated cells, decrease in the periciliary layer with ciliary damage and crowding, and junctional barrier loss. (c) In normal small airways, dimeric IgA (structure shown in inset) is transcytosed by the polymeric Ig receptor (pIgR) into the mucosal lumen. Liberation of secretory IgA after pIgR cleavage at the luminal surface prevents bacterial invasion. (d) Expression of pIgR is reduced by smoking, which leads to a localized secretory IgA deficiency in small airways and allows bacteria to invade and induce sustained airway inflammation. Abbreviations: Ig, immunoglobulin; NF-κB, nuclear factor-κB. (Figure adapted with permission from Reference 16. Copyright © 2020 American Thoracic Society. All rights reserved. The American Journal of Respiratory and Critical Care Medicine is an official journal of the American Thoracic Society. Readers are encouraged to read the entire article for the correct context at https://doi.org/10.1164/rccm.201710-2028PP. The authors, editors, and The American Thoracic Society are not responsible for errors or omissions in adaptations.)
