Abstract
Objectives
This study aims to identify older adult malnutrition in Texas, examine county-level characteristics associated with crude malnutrition death rates, and describe assets and opportunities available to address and improve malnutrition among the older population.
Design
Secondary data analysis using the Centers for Disease Control and Prevention’s WONDER online database, the U.S. Census 2014–2018 American Community Survey, and the U.S. Department of Agriculture’s Food Access Research Atlas data.
Setting
All 254 counties in the state of Texas.
Participants
Individuals aged 65 years and older.
Measurement
The dependent variable was the proportion of county-level malnutrition crude death rates. Independent variables included Health Provider Shortage Area designations, rurality, poverty status, food access, age, race, ethnicity, and education.
Results
The overall malnutrition crude death rate in Texas was 65.6 deaths per 100,000 older Texans, ranging from 0 to 414.46 deaths per 100,000 depending on the county. Higher malnutrition crude death rates were associated with non-metropolitan counties (P=0.018), lower education (P=0.047), greater household poverty (P=0.010), and low food access (P<0.001).
Conclusion
Socioeconomic disadvantages at the county-level appear to be one of the root causes of malnutrition crude death rates in Texas.
Key words: Malnutrition, death rates, Texas, older population, assets
Introduction
More than four million people ages 65 years or older live in the 254 counties that form the state of Texas in the United States (U.S.) (1, 2). In the past 12 months, close to 20% of older adults living in Texas were considered food insecure and experienced food intake disruptions because of lack of money or other resources financial constraints and lack of resources (3, 4). Consequently, food insecurity significantly increases the risks of malnutrition among older adults (5, 6).
Defined as deficiencies, excesses, or imbalances in a person’s consumption of nutrients (7), malnutrition is caused by a combination of social, psychological, physical, and medical factors, including impaired oral health and polypharmacy (8–12). Malnutrition can have severe consequences on older adults’ health, causing diminished physical health, loss of independence, increased hospitalizations and healthcare costs, and related death (13–18). Malnutrition and related risk factors can be detected in many ways at the individual-level, including the use of several validated screening tools for older adults (19–21). However, not much is known on related factors associated with county-level malnutrition death rates among older adults living in Texas.
As the older population grows and continues to age, more attention is needed to better understand older adult malnutrition and the factors that contribute to malnutrition-related death at the Texas county-level. While the individual-level contributors to and consequences of malnutrition are known and important (as referenced above), less is known about the communitylevel influences on malnutrition death among older adults (22). An abundance of available studies about malnutrition examine school-aged youth (23–25); however, when older adults are specifically examined, studies typically target individual-level variables among mostly community-dwelling older adults (26). Unfortunately, such studies do not consider the totality of the aging population in a particular geographic area within the context of available resources young AND MIDDLE AGED ADULTS residents residing in the same geographic area. A community’s composition of residents by sociodemographics, affluence, and utilization of subsidized benefits and programs can reveal protective and harmful community-level aspects for malnutrition risk and associated death (27–29). Because resource and service availability and accessibility differ by community such that older adults may experience longer distances and drive times to access food in rural communities (30, 31), and are driven in part by available funding and population need (32), research is needed that examines malnutrition in a community context.
The purposes of this study were to identify the overall crude malnutrition death rates among older adults ages 65 years and older living in Texas, and examine county-level characteristics associated with the related death rates. Texas was purposively selected for this investigation because of its large geospatial region, diverse population, and large number of counties. This “state of the state” on malnutrition of older adults living in Texas can be used to guide and inform future state-level public health and nutrition programs, services, and policy efforts. The present study also reveals assets and opportunities available to address and improve malnutrition among the older population. Therefore, the present study serves as a potential model to be replicated by other U.S. States states to better understand the risks, disparities, and inequities associated with malnutrition and associated deaths among older adults.
Methods
Data were gathered from secondary, publicly available sources and compiled into a single dataset. Counties served as the unit of analysis, of which there are 254 in Texas. Data available by Census track were aggregated at the county-level for consistency. Considering Census tracks do not cross county boundaries, summing these more granular components was capable of accurately yielding county-level totals.
Measures
Malnutrition
The dependent variable for this study was the proportion of county-level malnutrition crude death rates. Malnutrition deaths counts were obtained from the Centers for Disease Control and Prevention’s WONDER online database (33). County-level 2018 malnutrition death counts and crude death rates for individuals ages 65 years and older were identified using International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM) Codes E40–E46 (34). Statistical tertiles were calculated by county-level crude death rates to divide the counties for comparison purposes.
Rural and underserved designations
Of the many available designations to classify rural and underserved areas (35), two were selected: 1) Health Provider Shortage Areas (HPSA) and 2) Rural-Urban Continuum Codes (RUCC). HPSA, developed by the U.S. Health Resources Administration, are calculated based on the ratio of primary care providers to the population (36). HPSA are used as an indicator of access to healthcare services and can be applied to the entire county or specific parts of a county (i.e., any census tract or minor civil division). As a conservative measure and for ease of interpretation, partial and full county HPSA designations were collapsed into one category for analyses (i.e., 0=no HPSA designation; 1=partial/full county HPSA designation). RUCC, developed by the U.S. Department of Agriculture, are calculated based on commuting distance and proximity to populated areas (37). This 9-point scale categorizes counties into three metropolitan and six non-metropolitan rankings. Analyses treated RUCC as a binary variable comparing metropolitan (=0) to non-metropolitan (=1) areas.
Population demographics
U.S. Census data from the 5-Year American Community Survey (ACS, 2014–2018) were used for population-level age, race, ethnicity, and education level (38). Data were available at the Census Track level, but aggregated to the county-level. Given the present study focus on older adults, age was examined in two ways: the percent of the county population 1) ages 65 years and older; and 2) ages 85 years and older. For race, percentages for race were identified for: white, Black/African American, American Indian/Native American; Asian/Pacific Islander, Native Hawaiian/Alaska Native; other race, and two or more (i.e., multiple) races. Similarly, percentages were identified for the Hispanic population and adults who did not graduate from high school.
Poverty status
U.S. Census data from the 5-Year ACS (2014–2018) were also used for household-level poverty status and receipt of Supplemental Nutrition Assistance Program (SNAP) benefits (38). The percentage of households in poverty, i.e., living at or below the poverty level threshold in the past 12 months, was identified and calculated while considering household size and composition (39). The percentage of households with a resident age 60 years or older that received SNAP benefits was also identified (40).
Food access
Food Access Research Atlas data from the U.S. Department of Agriculture Economic Research Service was used to identify the percentage of adults age 65 years and older with low access to food stores. This proportion was calculated in two ways: those that resided 1 mile or farther from a food store; those that resided 10 miles or farther from a food store.
Other Data
In addition to the variables identified above, additional organizations were identified to assist in the development of a risk and asset map for malnutrition risk. Using available data sources, asset addresses were gathered for purposes of geospatial mapping. More specifically, addresses were compiled for the Texas Area Agencies on Aging (n=28), foodbanks and food pantries across the state (n=72), and all retail food stores (n=6,476). Food stores were identified by their standard industrial classification (SIC) code and included retailers labeled as food markets, grocers, meat, fruit/vegetable/produce, farm markets, and health/diet foods (41).
Statistical Analyses
Data were analyzed using SPSS version 27. Descriptive statistics were created for all variables of interest, which were compared across malnutrition crude death rate tertiles. Pearson chi-square tests were used for categorical variables and one-way analysis of variance (ANOVA) tests were used for continuous variables. Then, an ordinal regression model was fitted to examine county-level factors associated with higher malnutrition crude death rates. Statistical significance for all analyses was identified at P<0.05.
Results
Overall, across the 254 counties in Texas, there were 25,195 malnutrition-related deaths among adults ages 65 years and older. The average number of malnutrition deaths by county was 99.19 deaths, which ranged from 0 to 3,796 deaths. As seen in Figure 1, the overall malnutrition crude death rate in Texas was 65.6 deaths per 100,000 older adults, which ranged by county from 0 to 414.46 deaths per 100,000 older adults.
Figure 1.
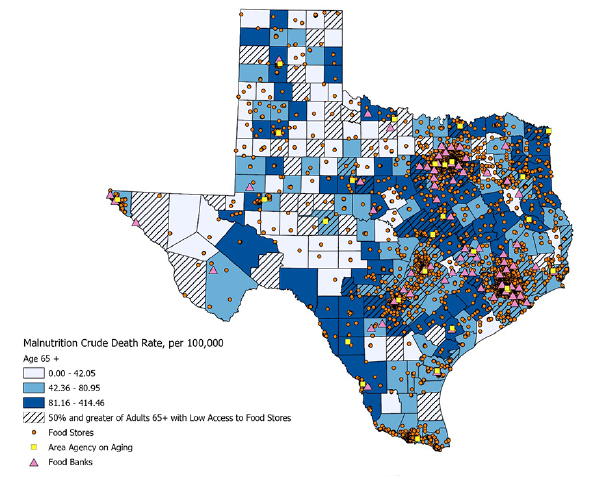
Risk and asset map for malnutrition
Of the 254 counties, 67.7% were classified as non-metropolitan areas, and 81.5% were determined as a HPSA in parts of the county (5.5%) or the entire county (76.0%). In addition to depicting malnutrition risk, Figure 1 also displays the various assets available in these geographic areas.
Table 1 displays county-level characteristics. On average, 17.53% (±5.31) of county residents were ages 65 years or older and 2.00% (±0.82) were ages 85 years or older. On average, 83.90% (±10.20) of county residents were white and 6.34% (±6.61) were Black/African American; 34.84% (±23.27) were of Hispanic origin. On average, 21.20% (±9.37) of county residents had less than a high school education, 61.58% (±9.37) of county households were at or below the poverty threshold, and 33.64% (±13.68) of county households with one or more resident age 60 years or older received SNAP benefits. On average, 62.37% (±21.25) and 19.06% (±26.58) of county residents ages 65 years and older had low access to food stores within 1 mile and 10 miles of their residence, respectively.
Table 1.
County-Level Characteristics by Malnutrition Crude Death Rates (in tertiles)
| County Malnutrtion Crude Death Rates for Age 65+ | ||||||
|---|---|---|---|---|---|---|
| Total (n = 254) | Tertile 1 (n = 84) | Tertile 2 (n = 85) | Tertile 3 (n = 85) | χ2 or f | P | |
| Malnutrition | ||||||
| Number of Malnutrition Deaths (65+ years) | 99.19 (±324.26) | 3.35 (±9.37) | 92.21 (±147.62) | 200.89 (±524.51) | 8,33 | <0.001 |
| Malnutrition Crude Death Rates (65+ years) | 65.62 (±60.39) | 4.93 (±12.94) | 63.08 (±11.24) | 128.14 (±55.21) | 287,27 | <0.001 |
| Rural-Urban Continuum Code (RUCC) | 14,43 | 0,001 | ||||
| Metro | 32,30% | 16,70% | 42,40% | 37,60% | ||
| Non-Metro | 67,70% | 83,30% | 57,60% | 62,40% | ||
| Health Provider Shortage Area (HPSA) | 5,67 | 0,059 | ||||
| None | 18,50% | 10,70% | 20,00% | 24,70% | ||
| Partial/Full | 81,50% | 89,30% | 80,00% | 75,30% | ||
| Percent of County Population Older Adult | ||||||
| Age 65 Years and Older | 17.53 (±5.31) | 19.01 (±5.54) | 16.86 (±5.50) | 16.75 (±4.59) | 5,01 | 0,007 |
| Age 85 Years and Older | 2.00 (±0.82) | 2.06 (±0.92) | 1.88 (±0.78) | 2.05 (±0.75) | 1,32 | 0,268 |
| Percent of County Population by Race | ||||||
| White | 83.90 (±10.20) | 85.66 (±12.25) | 83.66 (±9.07) | 82.40 (±8.80) | 2,22 | 0,111 |
| Black/African American | 6.34 (±6.61) | 2.96 (±3.57) | 7.25 (±6.73) | 8.78 (±7.44) | 20,25 | <0.001 |
| American Indian/Native American | 0.58 (±0.56) | 0.53 (±0.62) | 0.53 (±0.43) | 0.67 (±0.62) | 1,67 | 0,191 |
| Asian/Pacific Islander | 1.09 (±2.01) | 0.45 (±0.59) | 1.70 (±3.03) | 1.11 (±1.36) | 8,65 | <0.001 |
| Native Hawaiian/Alaska Native | 0.06 (±0.14) | 0.03 (±0.13) | 0.06 (±0.09) | 0.09 (±0.19) | 3,67 | 0,027 |
| Other Race | 5.77 (±8.00) | 8.38 (±12.17) | 4.43 (±4.53) | 4.53 (±3.94) | 7,00 | 0,001 |
| Two or More Races | 2.27 (±1.48) | 1.99 (±1.70) | 2.38 (±1.15) | 2.43 (±1.53) | 2,25 | 0,107 |
| Percent of County Population Hispanic | 34.84 (±23.27) | 37.94 (±23.74) | 33.54 (±23.44) | 33.06 (±22.58) | 1,13 | 0,325 |
| Percent of County Population Without High School Education | 21.20 (±9.20) | 24.46 (±11.58) | 19.16 (±7.39) | 20.01 (±7.16) | 8,55 | <0.001 |
| Percent of County Households In Poverty | 61.58 (±9.37) | 62.17 (±10.07) | 62.74 (±9.48) | 59.83 (±8.35) | 2,33 | 0,099 |
| Percent of County Households Receiving SNAP Benefits (60+) | 33.64 (±13.68) | 37.21 (±19.77) | 32.26 (±7.05) | 31.47 (±10.42) | 4,49 | 0,012 |
| Percent of County Population 65+ with Low Access to Food | ||||||
| Within 1 Mile of Residence | 62.37 (±21.25) | 66.44 (±25.40) | 61.04 (±18.41) | 59.69 (±18.91) | 2,41 | 0,092 |
| Within 10 Miles of Residence | 19.06 (±26.58) | 37.62 (±36.68) | 9.44 (±11.05) | 10.32 (±12.66) | 40,12 | <0.001 |
Table 1 also compares county-level characteristics across malnutrition crude death rate tertiles. Tertile 1 consisted of 84 counties with the lowest malnutrition-related crude death rates, which ranged from 0 to 42.05 malnutrition deaths per 100,000 older adults living in Texas. Tertile 2 consisted of 85 counties with moderate malnutrition-related crude death rates, which ranged from 42.36 to 80.95 malnutrition deaths per 100,000 older adults living in Texas. Tertile 3 consisted of 85 counties with the highest malnutrition-related crude death rates, which ranged from 81.16 to 414.46 malnutrition deaths per 100,000 older adults living in Texas.
When comparing county-level characteristics by the three statistical tertiles for malnutrition crude death rates, a significantly larger proportion of non-metropolitan counties were in Tertile 1 (χ2=14.43, P=0.001). Relative to Tertiles 2 and 3 with higher malnutrition crude death rates, on average, Tertile 1 had a larger proportion of residents ages 65 years and older (f=5.01, P=0.007) and without a high school education (f=8.55, P<0.001).
Relative to Tertile 1, Tertiles 2 and 3 with higher malnutrition crude death rates, on average, had larger proportions of residents who identified as Black/African American (f=20.25, P<0.001), Asian/Pacific Islander (f=8.65, P<0.001), and Native Hawaiian/Alaska Native (f=3.67, P=0.027). Conversely, on average, Tertile 1 had a larger proportion of residents who identified as another race not listed than Tertiles 2 and 3 (f=7.00, P=0.001). On average, compared to Tertiles 2 and 3, Tertile 1 had a larger proportion of households receiving SNAP benefits (f=4.49, P=0.012) and a larger proportion of residents ages 65 years and older with low access to food within 10 miles of their residence (f=40.12, P<0.001).
Table 2 shows the results of the ordinal regression model that assessed the association between county-level characteristics and levels of malnutrition crude death rates. Across Tertile levels, non-metropolitan RUCC classifications were associated with higher malnutrition crude death rates (β=0.86, P=0.018). Counties with larger proportions of residents who identified as another race (β=0.05, P=0.025), did not obtain a high school education (β=0.07, P=0.047), and lived in households at or below the poverty threshold (β=5.69, P=0.010) had higher malnutrition crude death rates. Counties with larger proportions of residents ages 65 years and older with low access to food stores within 10 miles had higher malnutrition crude death rates (β=0.04, P<0.001). Counties with larger proportions of residents ages 85 years and older (β=−0.52, P=0.015), and those who identified as Black/African American race (β=−0.12, P<0.001) and of Hispanic origin (β=−0.03, P=0.025) had lower malnutrition crude death rates.
Table 2.
Ordinal Regression for Malnutrition Crude Death Rate Tertiles
| Beta | SE | Wald | P | 95% CI | ||
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| RUCC: Non-Metro | 0,86 | 0,36 | 5,56 | 0,018 | 0,14 | 1,57 |
| HPSA: Partial/Full | 0,22 | 0,36 | 0,36 | 0,546 | −0,48 | 0,92 |
| Percent of County Population: Age 85+ | −0,52 | 0,21 | 5,88 | 0,015 | −0,93 | −0,10 |
| Percent of County Population: Black/African American | −0,12 | 0,03 | 17,62 | <0.001 | −0,17 | −0,06 |
| Percent of County Population: American Indian/Native American | −0,39 | 0,27 | 2,16 | 0,142 | −0,91 | 0,13 |
| Percent of County Population: Asian/Pacific Islander | 0,06 | 0,07 | 0,62 | 0,430 | −0,09 | 0,20 |
| Percent of County Population: Native Hawaiian | −1,20 | 1,05 | 1,31 | 0,253 | −3,27 | 0,86 |
| Percent of County Population: Other Race | 0,05 | 0,02 | 5,04 | 0,025 | 0,01 | 0,10 |
| Percent of County Population: Two or More Races | −0,08 | 0,10 | 0,64 | 0,424 | −0,28 | 0,12 |
| Percent of County Population: Hispanic | −0,03 | 0,01 | 5,00 | 0,025 | −0,05 | −0,01 |
| Percent of County Population: Without High School Education | 0,07 | 0,04 | 3,95 | 0,047 | 0,01 | 0,14 |
| Percent of County Households In Poverty | 5,69 | 2,22 | 6,56 | 0,010 | 1,34 | 10,04 |
| Percent of County Households with 60+ Resident: Receiving SNAP Benefits | 0,02 | 0,01 | 3,15 | 0,076 | 0,00 | 0,05 |
| Percent of County Population 65+: Low Access to Food within 10 Miles | 0,04 | 0,01 | 20,34 | <0.001 | 0,02 | 0,06 |
Nagelkerke R2 = 0.426
Discussion
The current study demonstrates that malnutrition remains an important issue for older adults living in Texas. Findings expand on previous research (3) and offer a deeper understanding of the context of malnutrition-related deaths by examining county-level characteristics, which may be addressed to mitigate the burden.
While malnutrition-related deaths occurred in many Texas counties, crude death rates showed related deaths are particularly higher in non-metropolitan counties. Findings also suggest that proxies of lower, community-level socioeconomic status including less educated and more impoverished communities in rural areas in Texas were more vulnerable to food insecurity (i.e., low access to food within 10 miles) and other issues contributing to malnutrition deaths. A recent systematic review and meta-analysis of factors associated with malnutrition and malnutrition risk among older adults found that low education level and low socioeconomic status were strongly associated with malnutrition risk (42). Poor rural households often have lower access to food in general (43), and lower utilization of the redistribution economy, which are government programs and charities that provide food resources such as food stamps, food banks, and senior meal programs (43). Interestingly, in this study, more older adults in Tertile 1 with the lowest malnutrition-related mortality received SNAP benefits compared to Tertiles 2 and 3. However, access to SNAP does not appear protective of malnutrition deaths. This may be attributed to the proportion of households seeking this benefit relative to those eligible, the composition of the household, and other challenges and resources that the household experiences (44–46). Further investigation at the family- and household-levels is needed to better understand the household circumstances associated with receiving SNAP benefits, and how these household characteristics influence malnutrition death among older adults.
Findings also indicate that the community infrastructure such as food access and household income may be more predictive of malnutrition death than access to healthcare services (4, 47). While parts of most counties were considered to be HPSA where access to healthcare facilities and professionals are partially or fully scarce, socioeconomic disadvantages were found to be at the root causes of malnutrition crude death rates in Texas (48).
Communities with larger proportions of older adults aged 85 years and over were found to have lower malnutrition crude death rates. While this may seem counterintuitive, it is possible that other supports or characteristics help the oldest county residents meet their nutrition needs. This older age group may have greater access to home-delivered meals such as Meals on Wheels (49). Those who are not homebound may attend senior centers or adult day cares where they can partake in congregate or individual meals. A 2010 Institute of Medicine workshop summary revealed that in 60 percent of the cases, the meals provided by a senior center or at home represents more than half of the older person’s daily food intake (50). Adults ages 85 years and older may also be residing in multigenerational households (51, 52), or have caregivers or family members who help them with meal shopping and preparation to stay well nourished (51). Some communities with large populations of adults ages 85 years and older may have specific resources and policies in place that better support older adults. This may include the needs of the oldest old, contributing to their longevity while protecting them against malnutrition risk and related death. Such examples may include a greater sense of community, coherence, and inclusion of older people (53–55), as well as informal support networks where meals are encouraged and modeled (56).
Communities with larger proportions of Black/African American and Hispanic residents also seemed protected against malnutrition death. One potential explanation is that food is an important symbol associated with cultural and social identities of African Americans and Hispanics (57). For example, prior research found that food is an opportunity for African American women to express their cultural values of responsibility, caretaking, and social connection with others (58), which may help to buffer malnutrition risk and associated deaths among the older population as seen in this study. Multigenerational living arrangements, which are more common among minority populations (59, 60), may also play a key role in lowering malnutrition death rates.
The current study is not without limitations. First, the study focused specifically on older adults ages 65 years and older. Examining malnutrition crude death rates before entering older adulthood may help to better understand specific upstream socioeconomic status factors needed for prevention. Second, additional variables associated with food access, such as transportation, may have helped to provide a more comprehensive overview of the root causes of malnutrition crude death rates. Future studies should consider adding additional relevant individual-level measures and data sources. Third, because secondary data from 2018 were used, findings may not represent the most current situation in these counties. Further, the state of malnutrition risk examined in these counties was before the COVID-19 pandemic; therefore, additional investigation is needed to identify the protective and risk characteristics associated with community changes (e.g., increasing poverty and death rates generally, closing of retail stores).
Despite these possible shortcomings, this study maps malnutrition crude death rates across all 254 counties in Texas, to identify county-level factors associated with malnutrition among the older adult population. Findings can be useful for simultaneously identifying county-level malnutrition risk alongside protective community aspects. This “state of the state” about malnutrition older adults experience in Texas can be used to guide and inform funding and service allocation for public health and nutrition programs across the state. It can be used to proactively identify need and support communities and organizations to better serve their older adult residents, especially among those residing in disadvantaged counties as identified in this study. Further, this study serves as a potential model to be replicated by other states to better understand the county-level risks, disparities, and inequities associated with malnutrition and associated deaths among older adults.
Acknowledgement
None.
Funding: None.
Ethical standards: The research team followed ethical standards based on the publicly available and accessible data sources used for the analyses.
Disclosure: Caroline D. Bergeron has no conflict of interest to disclose. Jessica Mary John has no conflict of interest to disclose. Mitali Sribhashyam has no conflict of interest to disclose. Gloria Odonkor has no conflict of interest to disclose. Oluyomi Oloruntoba has no conflict of interest to disclose. Ashley L. Merianos has no conflict of interest to disclose. Scott Horel has no conflict of interest to disclose. Matthew Lee Smith has no conflict of interest to disclose.
References
- 1.Texas Demographic Center. Demographics of Texas and the Aging of the Population [Internet]. 2018 [cited 2020 Jul 11]. Available from: https://demographics.texas.gov/Resources/Presentations/OSD/2018/2018_02_22_JLLSeniorsHousingOutlook.pdf
- 2.Texas Health and Human Services. Center for Health Statistics Texas County Numbers and Public Health Regions [Internet]. 2014 [cited 2020 Jul 11]. Available from: https://www.dshs.texas.gov/chs/info/info_txco.shtm#:∼:text=Each%20of%20the%20254%20Texas,assigned%20sequentially%20in%20alphabetical%20order.
- 3.America’s Health Rankings. Food Insecurity — Ages 60+ in Texas [Internet]. 2020 [cited 2020 Jul 11]. Available from: https://www.americashealthrankings.org/explore/senior/measure/food_insecurity_sr/state/TX
- 4.Office of Disease Prevention and Health Promotion. Food Insecurity [Internet]. 2020 [cited 2021 Feb 5]. Available from: https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-health/interventions-resources/food-insecurity
- 5.Grammatikopoulou MG, Gkiouras K, Theodoridis X, Tsisimiri M, Markaki AG, Chourdakis M, et al. Food insecurity increases the risk of malnutrition among community-dwelling older adults. Maturitas. 2019;119:8–13. doi: 10.1016/j.maturitas.2018.10.009. [DOI] [PubMed] [Google Scholar]
- 6.Hall B, Brown JL. Food security among older adults in the United States. Top Clin Nutr. 2005;20(4):329–38. doi: 10.1097/00008486-200510000-00006. [DOI] [Google Scholar]
- 7.World Health Organization. Malnutrition [Internet]. 2020 [cited 2020 Jul 11]. Available from: https://www.who.int/news-room/fact-sheets/detail/malnutrition
- 8.Fávaro-Moreira NC, Krausch-Hofmann S, Matthys C, Vereecken C, Vanhauwaert E, Declercq A, et al. Risk Factors for Malnutrition in Older Adults: A Systematic Review of the Literature Based on Longitudinal Data. Adv Nutr. 2016;7(3):507–22. doi: 10.3945/an.115.011254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Azzolino D, Passarelli PC, De Angelis P, Piccirillo GB, D’Addona A, Cesari M. Poor Oral Health as a Determinant of Malnutrition and Sarcopenia. Nutrients. 2019;11(12):2898. doi: 10.3390/nu11122898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jyrkkä J, Mursu J, Enlund H, Lönnroos E. Polypharmacy and nutritional status in elderly people. Curr Opin Clin Nutr Metab Care. 2012;15(1):1–6. doi: 10.1097/MCO.0b013e32834d155a. [DOI] [PubMed] [Google Scholar]
- 11.Little MO. Updates in nutrition and polypharmacy. Curr Opin Clin Nutr Metab Care. 2018;21(1):4–9. doi: 10.1097/MCO.0000000000000425. [DOI] [PubMed] [Google Scholar]
- 12.the PreMiO Study Group. Muscaritoli M, Lucia S, Farcomeni A, Lorusso V, Saracino V, et al. Prevalence of malnutrition in patients at first medical oncology visit: the PreMiO study. Oncotarget. 2017;8(45):79884–96. doi: 10.18632/oncotarget.20168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Norman K, Pichard C, Lochs H, Pirlich M. Prognostic impact of disease-related malnutrition. Clin Nutr. 2008;27(1):5–15. doi: 10.1016/j.clnu.2007.10.007. [DOI] [PubMed] [Google Scholar]
- 14.Deutz NEP, Ashurst I, Ballesteros MD, Bear DE, Cruz-Jentoft AJ, Genton L, et al. The Underappreciated Role of Low Muscle Mass in the Management of Malnutrition. J Am Med Dir Assoc. 2019;20(1):22–7. doi: 10.1016/j.jamda.2018.11.021. [DOI] [PubMed] [Google Scholar]
- 15.Abizanda P, Sinclair A, Barcons N, Lizán L, Rodríguez-Mañas L. Costs of Malnutrition in Institutionalized and Community-Dwelling Older Adults: A Systematic Review. J Am Med Dir Assoc. 2016;17(1):17–23. doi: 10.1016/j.jamda.2015.07.005. [DOI] [PubMed] [Google Scholar]
- 16.Martínez-Reig M, Aranda-Reneo I, Peña-Longobardo LM, Oliva-Moreno J, Barcons-Vilardell N, Hoogendijk EO, et al. Use of health resources and healthcare costs associated with nutritional risk: The FRADEA study. Clin Nutr. 2018;37(4):1299–305. doi: 10.1016/j.clnu.2017.05.021. [DOI] [PubMed] [Google Scholar]
- 17.Sparre-Sørensen M, Kristensen GN. Malnutrition related deaths. Clin Nutr ESPEN. 2016;15:63–8. doi: 10.1016/j.clnesp.2016.06.001. [DOI] [PubMed] [Google Scholar]
- 18.Shakersain B, Santoni G, Faxén-Irving G, Rizzuto D, Fratiglioni L, Xu W. Nutritional status and survival among old adults: an 11-year population-based longitudinal study. Eur J Clin Nutr. 2016;70(3):320–5. doi: 10.1038/ejcn.2015.109. [DOI] [PubMed] [Google Scholar]
- 19.Todorovic V, Russell C, Elia M. The “MUST” Explanatory Booklet: A Guide to the Malnutrition Universal Screening Tool (MUST) for Adults [Internet] Redditch, UK: BAPEN; 2003. [Google Scholar]
- 20.Rubenstein LZ, Harker JO, Salva A, Guigoz Y, Vellas B. Screening for Undernutrition in Geriatric Practice: Developing the Short-Form Mini-Nutritional Assessment (MNA-SF) J Gerontol A Biol Sci Med Sci. 2001;56(6):M366–72. doi: 10.1093/gerona/56.6.M366. [DOI] [PubMed] [Google Scholar]
- 21.Keller HH, Goy R, Kane S-L. Validity and reliability of SCREEN II (Seniors in the Community: Risk evaluation for eating and nutrition, Version II) Eur J Clin Nutr. 2005;59(10):1149–57. doi: 10.1038/sj.ejcn.1602225. [DOI] [PubMed] [Google Scholar]
- 22.Lee MR, Berthelot ER. Community Covariates of Malnutrition Based Mortality Among Older Adults. Ann Epidemiol. 2010;20(5):371–9. doi: 10.1016/j.annepidem.2010.01.008. [DOI] [PubMed] [Google Scholar]
- 23.Herrador Z, Sordo L, Gadisa E, Moreno J, Nieto J, Benito A, et al. Cross-Sectional Study of Malnutrition and Associated Factors among School Aged Children in Rural and Urban Settings of Fogera and Libo Kemkem Districts, Ethiopia. PLoS ONE. 2014;9(9):e105880. doi: 10.1371/journal.pone.0105880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhou S, Ye B, Fu P, Li S, Yuan P, Yang L, et al. Double Burden of Malnutrition: Examining the Growth Profile and Coexistence of Undernutrition, Overweight, and Obesity among School-Aged Children and Adolescents in Urban and Rural Counties in Henan Province, China. J Obes. 2020;2020:1–11. doi: 10.1155/2020/2962138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Spoede E, Corkins MR, Spear BA, Becker PJ, Gunnell Bellini S, Hoy MK, et al. Food Insecurity and Pediatric Malnutrition Related to Under- and Overweight in the United States: An Evidence Analysis Center Systematic Review. J Acad Nutr Diet. 2020 May;S2212267220302835. [DOI] [PubMed]
- 26.Harris PS, Payne L, Morrison L, Green SM, Ghio D, Hallett C, et al. Barriers and facilitators to screening and treating malnutrition in older adults living in the community: a mixed-methods synthesis. BMC Fam Pract. 2019;20(1):100. doi: 10.1186/s12875-019-0983-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Elia M, Stratton RJ. Geographical inequalities in nutrient status and risk of malnutrition among English people aged 65 y and older. Nutrition. 2005;21(11–12):1100–6. doi: 10.1016/j.nut.2005.03.005. [DOI] [PubMed] [Google Scholar]
- 28.Donini LM, Scardella P, Piombo L, Neri B, Asprino R, Proietti AR, et al. Malnutrition in elderly: Social and economic determinants. J Nutr Health Aging. 2013;17(1):9–15. doi: 10.1007/s12603-012-0374-8. [DOI] [PubMed] [Google Scholar]
- 29.Nakade M, Kondo K. Malnutrition in Older People. In: Kondo K, editor. Social Determinants of Health in Non-communicable Diseases [Internet]. Singapore: Springer Singapore; 2020 [cited 2021 Feb 13]. p. 147–58. (Springer Series on Epidemiology and Public Health). Available from: 10.1007/978-981-15-1831-7_13
- 30.Chung WT, Gallo WT, Giunta N, Canavan ME, Parikh NS, Fahs MC. Linking Neighborhood Characteristics to Food Insecurity in Older Adults: The Role of Perceived Safety, Social Cohesion, and Walkability. J Urban Health. 2012;89(3):407–18. doi: 10.1007/s11524-011-9633-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Levasseur M, Généreux M, Bruneau J-F, Vanasse A, Chabot É, Beaulac C, et al. Importance of proximity to resources, social support, transportation and neighborhood security for mobility and social participation in older adults: results from a scoping study. BMC Public Health. 2015;15(1):503. doi: 10.1186/s12889-015-1824-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Fricke HE, Hughes AG, Schober DJ, Pinard CA, Bertmann FMW, Smith TM, et al. An Examination of Organizational and Statewide Needs to Increase Supplemental Nutrition Assistance Program (SNAP) Participation. J Hunger Environ Nutr. 2015;10(2):271–83. doi: 10.1080/19320248.2015.1004217. [DOI] [Google Scholar]
- 33.Centers for Disease Control and Prevention. CDC WONDER [Internet]. 2020 [cited 2021 Jan 7]. Available from: https://wonder.cdc.gov/
- 34.Centers for Medicare & Medicaid Services. 2018 ICD-10 CM and GEMS [Internet]. 2017 [cited 2020 Dec 20]. Available from: https://www.cms.gov/Medicare/Coding/ICD10/2018-ICD-10-CM-and-GEMs
- 35.Smith ML, Dickerson JB, Wendel ML, Ahn S, Pulczinski JC, Drake KN, et al. The Utility of Rural and Underserved Designations in Geospatial Assessments of Distance Traveled to Healthcare Services: Implications for Public Health Research and Practice. J Environ Public Health. 2013;2013:1–11. doi: 10.1155/2013/960157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Health Resources & Services Administration. Data Downloads [Internet]. 2021 [cited 2021 Jan 10]. Available from: https://data.hrsa.gov/data/download
- 37.United States Department of Agriculture. Rural-Urban Continuum Codes [Internet]. 2020 [cited 2021 Jan 10]. Available from: https://www.ers.usda.gov/data-products/rural-urban-continuum-codes/
- 38.United States Census Bureau. Standard Hierarchy of Census Geographic Entities [Internet]. 2020 [cited 2021 Jan 10]. Available from: https://www2.census.gov/geo/pdfs/reference/geodiagram.pdf?#
- 39.United States Census Bureau. How the Census Bureau Measures Poverty [Internet]. 2020 [cited 2021 Jan 10]. Available from: https://www.census.gov/topics/income-poverty/poverty/guidance/poverty-measures.html
- 40.Feeding America. Understanding SNAP, the Supplemental Nutrition Assistance Program [Internet]. 2021 [cited 2021 Jan 10]. Available from: https://www.feedingamerica.org/take-action/advocate/federal-hunger-relief-programs/snap
- 41.North American Industry Classification System Association. Search SIC Codes by Industry [Internet]. 2018 [cited 2021 Feb 13]. Available from: https://www.naics.com/sic-codes-industry-drilldown/
- 42.Besora-Moreno M, Llauradó E, Tarro L, Solà R. Social and Economic Factors and Malnutrition or the Risk of Malnutrition in the Elderly: A Systematic Review and Meta-Analysis of Observational Studies. Nutrients. 2020;12(3):737. doi: 10.3390/nu12030737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Morton LW, Bitto EA, Oakland MJ, Sand M. Accessing food resources: Rural and urban patterns of giving and getting food. Agric Hum Values. 2007;25(1):107–19. doi: 10.1007/s10460-007-9095-8. [DOI] [Google Scholar]
- 44.U.S. Department of Agriculture, Food and Nutrition Service. SNAP Eligibility [Internet]. 2021 [cited 2021 Jan 31]. Available from: https://www.fns.usda.gov/snap/recipient/eligibility
- 45.Center on Budget and Policy Priorities. Chart Book: SNAP Helps Struggling Families Put Food on the Table [Internet]. 2019 [cited 2021 Jan 31]. Available from: https://www.cbpp.org/research/food-assistance/chart-book-snap-helps-struggling-families-put-food-on-the-table
- 46.Cohen N. SNAP at the Community Scale: How Neighborhood Characteristics Affect Participation and Food Access. Am J Public Health. 2019;109(12):1646–51. doi: 10.2105/AJPH.2019.305363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Samuel LJ, Szanton SL, Weiss CO, Thorpe RJ, Semba RD, Fried LP. Financial Strain Is Associated with Malnutrition Risk in Community-Dwelling Older Women. Epidemiol Res Int. 2012;2012:696518. doi: 10.1155/2012/696518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.National Academies of Sciences, Engineering, and Medicine, Health and Medicine Division, Board on Population Health and Public Health Practice, Committee on Community-Based Solutions to Promote Health Equity in the United States. Weinstein JN, Geller A, et al. Communities in Action: Pathways to Health Equity. Washington, D.C.: The National Academies Press; 2017. The Root Causes of Health Inequity. [PubMed] [Google Scholar]
- 49.Shan M, Gutman R, Dosa D, Gozalo PL, Ogarek JA, Kler S, et al. A New Data Resource to Examine Meals on Wheels Clients’ Health Care Utilization and Costs. Med Care. 2019;57(3):e15–21. doi: 10.1097/MLR.0000000000000951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Institute of Medicine. Providing Healthy and Safe Foods As We Age: Workshop Summary [Internet] Washington, D.C.: National Academies Press; 2010. [PubMed] [Google Scholar]
- 51.Bernstein M, Munoz N. Position of the Academy of Nutrition and Dietetics: Food and Nutrition for Older Adults: Promoting Health and Wellness. J Acad Nutr Diet. 2012;112(8):1255–77. doi: 10.1016/j.jand.2012.06.015. [DOI] [PubMed] [Google Scholar]
- 52.United States Census Bureau. Family Gatherings: Percent of Households that are Multigenerational [Internet]. 2019 [cited 2021 Jan 31]. Available from: https://www.census.gov/library/visualizations/2019/comm/family-gatherings.html
- 53.Eskelinen K, Hartikainen S, Nykänen I. Is Loneliness Associated with Malnutrition in Older People? Int J Gerontol. 2016;10(1):43–5. doi: 10.1016/j.ijge.2015.09.001. [DOI] [Google Scholar]
- 54.Koelen M, Eriksson M, Cattan M, et al. Older People, Sense of Coherence and Community. In: Mittelmark MB, Sagy S, Eriksson M, Bauer GF, Pelikan JM, Lindström B, et al., editors. The Handbook of Salutogenesis [Internet] Cham: Springer International Publishing; 2017. [Google Scholar]
- 55.Callen BL, Wells TJ. Views of Community-Dwelling, Old-Old People on Barriers and Aids to Nutritional Health. J Nurs Scholarsh. 2003;35(3):257–62. doi: 10.1111/j.1547-5069.2003.00257.x. [DOI] [PubMed] [Google Scholar]
- 56.Stroebele-Benschop N, Depa J, de Castro JM. Environmental Strategies to Promote Food Intake in Older Adults: A Narrative Review. J Nutr Gerontol Geriatr. 2016;35(2):95–112. doi: 10.1080/21551197.2016.1173614. [DOI] [PubMed] [Google Scholar]
- 57.Bermudez OI, Tucker KL. Cultural Aspects of Food Choices in Various Communities of Elders. Generations. 2004;28(3):22–7. [Google Scholar]
- 58.Ahye BA, Devine CM, Odoms-Young AM. Values Expressed Through Intergenerational Family Food and Nutrition Management Systems Among African American Women. Fam Community Health. 2006;29(1):5–16. doi: 10.1097/00003727-200601000-00003. [DOI] [PubMed] [Google Scholar]
- 59.Cohn D, Passel JS. A record 64 million Americans live in multigenerational households [Internet]. Pew Research Center. 2018 [cited 2021 Jan 31]. Available from: https://www.pewresearch.org/fact-tank/2018/04/05/a-record-64-million-americans-live-in-multigenerational-households/
- 60.Guzman S. Multigenerational Housing on the Rise, Fueled by Economic and Social Changes [Internet]. AARP Public Policy Institute. 2019 [cited 2021 Jan 31]. Available from: https://www.aarp.org/content/dam/aarp/ppi/2019/06/multigenerational-housing.doi.org.10.26419-2Fppi.00071.001.pdf


