Abstract
Background
Coronavirus disease 2019 (COVID‐19) has wreaked health and economic damage globally. A thorough understanding of the characteristics of COVID‐19 patients in Australia plus the strategies that successfully ‘flatten the curve’ are vitally important to contain this pandemic.
Aim
To describe the clinical characteristics and outcomes of COVID‐19 patients in the Sutherland Shire, and the management model adopted to manage these patients.
Methods
A retrospective case series of COVID‐19 patients monitored in the Sutherland Shire between 19 March and 15 May 2020 was performed. Demographic, clinical and outcome data of COVID‐19 inpatients at the Sutherland Hospital and demographic data of COVID‐19 patients in the Sutherland Shire community were obtained. The Sutherland Hospital COVID‐19 Management Model involved close collaboration among the Sutherland Fever Clinic, Sutherland COVID‐19 community telemonitoring team (CTAC) and Sutherland COVID‐19 inpatient team.
Results
Ninety‐nine COVID‐19 cases (median age, 49 years, 50 (51%) male) were monitored in Sutherland Shire, with 19 cases (median age, 54 years, 10 (53%) male) requiring inpatient management. Common comorbidities included obesity, asthma, hypertension and Type 2 diabetes mellitus. Six (32%) patients required supplemental oxygen and three (16%) patients required intensive care admission. There was one mortality. The CTAC team identified five (5%) patients requiring admission, and three (3%) patients requiring re‐admission. The majority of COVID‐19 source was from overseas travel (67%), with nine (9%) cases having unknown source.
Conclusion
A comprehensive COVID‐19 management model is needed to successfully manage COVID‐19 patients in both outpatient and inpatient settings in order to ‘squash the curve’.
Keywords: COVID‐19, community management, Sutherland Shire
Introduction
The current severe acute respiratory syndrome coronavirus 2 (SARS‐CoV‐2) pandemic has resulted in unprecedented morbidity and mortality throughout the world. 1 Important risk factors associated with mortality includes advanced age, cardiorespiratory comorbidities, immunosuppression and diabetes mellitus. 2 , 3 The Sutherland Shire in New South Wales (NSW), Australia, has approximately 220 000 residents in 2016 National census. 4 It has a unique population with a higher proportion of those age 65 years and older, 4 85 years and older and coronary disease hospitalisations 5 compared to the rest of New South Wales. As such, when the first case of novel coronavirus disease 2019 (COVID‐19) was identified in Australia on 25 January 2020, 6 it was vitally important to have a comprehensive strategy in place to protect this vulnerable population.
Currently, the trajectory of COVID‐19 cases in Australia has compared favourably with the rest of the world. 7 However, there remains limited information regarding the clinical characteristics of COVID‐19 inpatients in Australia and the strategies undertaken to manage community COVID‐19 patients. Our Sydney hospital was among the first to manage such patients in Australia with our numbers also among the highest in NSW. We were therefore required to promptly implement our pre‐prepared comprehensive inpatient and outpatient strategy in March and now report on our first 8 weeks' experience.
This study will describe the demographics, clinical characteristics and outcomes of confirmed COVID‐19 patients in both the inpatient and outpatient setting and reports patients of all severities including their trajectory through intensive care unit (ICU). It also describes the COVID‐19 management model that integrated both hospital and community care, which was implemented at the Sutherland Shire.
Methods
Study design
This is a retrospective case series of all patients diagnosed with COVID‐19 in the Sutherland Shire between 19 March and 15 May 2020. All patients with confirmed COVID‐19 identified by positive results on reverse transcription polymerase chain reaction (RT‐PCR) of nasopharyngeal swabs in the Sutherland Shire were included.
The study was reviewed by South Eastern Sydney Local Health District (SESLHD) Ethics board and deemed to be a quality assurance project; hence, ethics was not required.
Data collection
Epidemiological, clinical, laboratory, radiological, treatment and outcome data from COVID‐19 inpatients were obtained from electronic medical records and recorded on a standardised data collection form, modified from the World Health Organization (WHO)/International Severe Acute Respiratory and Emerging Infection Consortium COVID‐19 case record form. 8 The total number of COVID‐19 patients in the Sutherland Shire was obtained from the NSW Ministry of Health and SESLHD COVID‐19 public health unit database, which included patients' postcodes, age, gender and source of COVID‐19.
Categorical variables were reported as frequency rates and percentages, and continuous variables were reported using median and interquartile range or range. All statistical analyses were performed using Statistical Package for the Social Sciences (SPSS), version 26.
COVID‐19 inpatients were classified based on severity adapted from definitions obtained from WHO guidelines. 9 , 10 Mild disease included patients with uncomplicated upper respiratory tract viral infection, non‐specific symptoms like fever, cough (with or without sputum production), anorexia, malaise, muscle pain, sore throat, dyspnoea, nasal congestion or headache, patients with pneumonia but no signs of severe pneumonia and no need for supplemental oxygen. Severe disease included patients with fever or suspected respiratory infection with one of the following: respiratory rate ≥30 breaths/min, severe respiratory distress, or oxygen saturation ≤93%. Patients with critical illness included patients with acute respiratory distress syndrome, septic shock or multiple organ dysfunctions.
Sutherland Hospital COVID‐19 response
Following the first cases of COVID‐19 in Australia, the Sutherland Hospital Respiratory Department began preparing a comprehensive strategy to manage a potential outbreak. This strategy was implemented even before the first COVID‐19 patient was admitted to hospital on 19 March 2020. The pathway for management of COVID‐19 patients is summarised in Figure 1.
Figure 1.
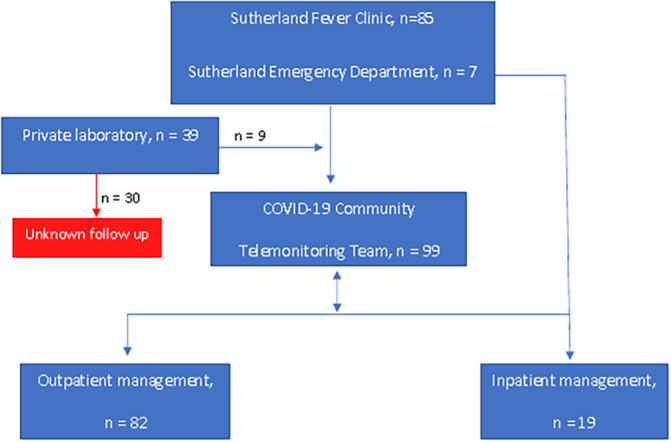
COVID‐19 management model.
Sutherland Hospital fever clinic
A daily outpatient clinic which was operated by the Sutherland Hospital Emergency team, with assistance from the Respiratory department, was implemented from 13 March 2020. Patients were tested for COVID‐19 based on NSW Ministry of Health (MoH) guidelines. Those who required further review were directed to the Emergency department. All patients received information regarding COVID‐19 and were instructed to self‐quarantine at home. They would be notified by public health regarding their results.
COVID‐19 community telemonitoring team
A COVID‐19 community telemonitoring team (CTAC) was formed consisting of one full‐time equivalent (FTE) respiratory specialists and two FTE registered nurses. This team was provided with a daily list of patients who had tested positive for COVID‐19 in the community by SESLHD public health unit. Their responsibilities were to review patients daily through Telehealth. This process involved a detailed medical and exposure history, dyspnoea score and regular review of symptom progression. The CTAC team liaised daily with the inpatient COVID‐19 team through scheduled phone calls regarding patients at risk of deterioration and facilitated direct transfers to the ward as necessary. Follow up by CTAC on all COVID‐19 patients continued until released from isolation according to the NSW MoH guidelines. Release from isolation was determined by the CTAC team.
COVID‐19 inpatient team
A COVID‐19 inpatient team was formed consisting of a weekly rotating roster of 2−3 respiratory consultants, registrar and intern/resident. This team was responsible for reviewing all confirmed COVID‐19 patients daily on a dedicated COVID‐19 respiratory ward and intensive care unit. The inpatient COVID‐19 team liaised closely with the CTAC team regarding discharges for ongoing follow up.
A COVID‐19 Respiratory Failure Protocol (Fig. S1) was devised with collaboration from the Respiratory, Intensive care and Emergency departments. This protocol was aimed to promptly manage both confirmed and unconfirmed COVID‐19 patients with respiratory failure in the most appropriate setting, and to reduce the risk of healthcare worker exposure. Due to concerns over transmission through inhalation of the virus aerosolised during high flow nasal prongs (HFNP) or non‐invasive ventilation (NIV), 11 our guidelines for respiratory failure patients was to avoid both HFNP and NIV. This decision was also based on overseas experience regarding the limited role of NIV in the setting of COVID‐19 and the initial support for early intubation in patients with respiratory failure. 9 , 12
Results
Baseline demographics and clinical characteristics of COVID‐19 patients
There was a total of 101 COVID‐19 cases identified, with 87 cases belonging to the Sutherland Shire based on postcodes, including all but three of the inpatients (Table 1). The COVID‐19 cases based on postcodes from NSW government 13 identified 117 COVID‐19 cases in the Sutherland Shire, showing 30 cases diagnosed by private laboratory who were not followed up by the CTAC team. Ninety‐nine COVID‐19 cases were followed up by the CTAC team, which identified five patients requiring admission and three patients requiring re‐admission. Two COVID‐19 inpatients were not followed up by the CTAC team, with one mortality and another being cleared from COVID‐19 during rehabilitation.
Table 1.
Baseline demographics and clinical characteristics of COVID‐19 patients
| Demographics | Community (n = 82) | Inpatients: total (n = 19) | Inpatients: mild (n = 11) | Inpatients: severe (n = 6) | Inpatients: critical (n = 2) |
|---|---|---|---|---|---|
| Age, median (interquartile range) (years) | 48 (31–63) | 54 (45–68) | 50 (39–54) | 68 (65–69) | 83 (79–87)† |
| Male sex, n (%) | 41 (50) | 10 (53) | 6 (55) | 3 (50) | 1 (50) |
| Comorbidities | |||||
| Cardiovascular disease, n (%) | |||||
| Hypertension | 9 (11) | 5 (26) | 1 (9) | 4 (67) | 0 |
| Ischaemic heart disease | 4 (5) | 1 (5) | 0 | 0 | 1 (50) |
| Respiratory disease, n (%) | |||||
| Asthma | 5 (6) | 5 (26) | 3 (27) | 2 (33) | 0 |
| Chronic obstructive pulmonary disease | 2 (2) | 2 (11) | 0 | 2 (33) | 0 |
| Type 2 diabetes mellitus, n (%) | 3 (4) | 5 (26) | 1 (9) | 2 (33) | 2 (100) |
| Chronic kidney disease, n (%) | 0 | 1 (5) | 1 (9) | 0 | 0 |
| Obesity (body mass index >30), n (%) | N/A | 7 (37) | 3 (27) | 4 (67) | 0 |
| Symptom onset to admission, median (days) | N/A | 9 | 9 | 9 | 3.5 |
†Median (range). N/A, not available.
Nineteen patients with confirmed COVID‐19 were admitted to Sutherland Hospital between 19 March and 15 May 2020. The median age was 54 years, ranging between 17 and 87 years. Approximately half (53%) of the patients were male. Four inpatients did not have any comorbidities. Similar to previous studies, 2 , 14 comorbidities of diabetes, hypertension and obesity were common in our series, although we had a larger proportion of patients with asthma comparatively. 15 The median time from symptom onset to hospital admission was 9 days for 18 patients. One patient was excluded as the time of symptom onset was not clear. Two patients were found to be co‐infected with influenza A. Eleven patients had mild disease, six patients had severe disease and two patients had critical disease. Older patients tended to have more severe and critical illness compared to younger patients, which is consistent with previous studies identifying older age as a risk factor for poor prognosis in COVID‐19 patients. 2 , 3 One patient had an initially negative test, with repeat testing (conducted based on clinical suspicion) being positive.
Clinical presentation and investigations
The most common self‐reported symptoms on hospital admission were dyspnoea (89%), cough (79%), lethargy (63%) and fever (58%) (Table 2), and this is comparable with data reported from recent studies. 2 , 14 Gastrointestinal symptoms, particularly diarrhoea (32%), had a higher prevalence in our cohort compared to China 14 (3%). This was significant in a few of our patients with concurrent anorexia, as they required intravenous fluids for hydration. This suggests that the severity classification of COVID‐19 based on respiratory signs may not accurately reflect the need for hospital admission. One patient presented primarily with a severe headache requiring further investigations with a computed tomography (CT) venogram, neurological review and treatment with amitriptyline. Dyspnoea was not as common among community COVID‐19 patients (15%), with cough, fever and sore throat being predominant symptoms.
Table 2.
Clinical presentation
| Symptoms on presentation | Community (n = 82) | Inpatient: total (n = 19) | Inpatient: mild (n = 11) | Inpatient: severe (n = 6) | Inpatient: critical (n = 2) |
|---|---|---|---|---|---|
| Constitutional, n (%) | |||||
| Fever | 30 (37) | 11 (58) | 4 (36) | 5 (83) | 2 (100) |
| Lethargy | 15 (18) | 12 (63) | 7 (64) | 5 (83) | 0 |
| Anorexia | 1 (1) | 8 (42) | 3 (27) | 5 (83) | 0 |
| Respiratory, n (%) | |||||
| Cough | 54 (66) | 15 (79) | 8 (73) | 5 (83) | 2 (100) |
| Dyspnoea | 12 (15) | 17 (89) | 10 (91) | 6 (100) | 1 (50) |
| Rhinorrhoea | 33 (40) | 2 (11) | 1 (9) | 1 (17) | 0 |
| Sore throat | 37 (45) | 5 (26) | 2 (18) | 2 (33) | 1 (50) |
| Chest pain | 6 (7) | 9 (47) | 7 (64) | 1 (17) | 1 (50) |
| Gastrointestinal, n (%) | |||||
| Diarrhoea | 8 (10) | 9 (47) | 3 (27) | 5 (83) | 1 (50) |
| Nausea | 2 (2) | 5 (26) | 1 (9) | 3 (50) | 1 (50) |
| Neurological, n (%) | |||||
| Lightheadedness | 2 (2) | 5 (26) | 3 (27) | 2 (33) | 0 |
| Headache | 28 (34) | 3 (16) | 3 (27) | 0 | 0 |
Initial vital signs and laboratory findings of inpatients are summarised in Supporting Information Table S1. D‐dimer was collected early in admission in 16 patients and ferritin was collected in 14 patients. On room air, patients in the critical group tended to have lower admission oxygen saturation (91%) compared to the mild group (96%) and higher temperature. Lymphopenia and elevated ferritin and D dimer were noted in the severe and critical group.
All inpatients received an admission chest X‐ray and initial abnormal findings were identified in 10 patients. Two patients had initially normal chest X‐rays but developed abnormalities during their admission. Eight patients had a CT chest during admission, with the most common abnormalities being bilateral ground glass opacities. Two patients had a normal CT chest.
Management
Of the 19 inpatients, six required supplemental oxygen through nasal cannula or Hudson mask (Table 3). Two patients required immediate supplemental oxygen on presentation, therefore oxygen saturation on room air was not documented. Three patients required intensive care admission, with one patient requiring intubation. Empirical antibiotics were given to six patients and one patient with influenza A coinfection was given oseltamivir. Oral corticosteroid was given to three patients with a concurrent exacerbation of asthma/chronic obstructive pulmonary disease and one patient with Addison disease. Due to the absence of proven therapies for SARS‐CoV‐2, the majority of patients did not receive targeted treatment. One critical patient received off‐label hydroxychloroquine and azithromycin 16 due to emerging evidence at that time of its effectiveness in reducing SARS‐CoV‐2 viral load. 17
Table 3.
Inpatient management
| Treatment | Total (n = 19) | Mild (n = 11) | Severe (n = 6) | Critical (n = 2) |
|---|---|---|---|---|
| Oxygen supplementation, n (%) | 6 (32) | 0 | 4 (67) | 2 (100) |
| Empirical antibiotics, n (%) | 6 (32) | 1 (9) | 4 (67) | 1 (50) |
| Oral corticosteroids, n (%) | 4 (21) | 2 (18) | 2 (33) | 0 |
| Hydroxychloroquine/azithromycin, n (%) | 1 (5) | 0 | 0 | 1 (50) |
| Intubation, n (%) | 1 (5) | 0 | 0 | 1 (50) |
| Intensive care admission, n (%) | 3 (16) | 0 | 2 (33) | 1 (50) |
Respiratory failure/supplemental oxygen course
Six patients required supplemental oxygen during the course of admission. The medium time from symptom onset to supplemental oxygen was 9.5 days. No patients received HFNP or NIV as per the COVID‐19 Respiratory Failure Protocol.
Case 2 was intubated on Day 3 of admission and was extubated successfully after 27 days. The decision to intubate was based on early expert recommendations that supported early intubation following the onset of increased oxygen requirements. 9 , 12 On admission to hospital, Case 2 had an oxygen requirement of 2 L through nasal cannula to maintain oxygen saturation above 95%. Deterioration occurred rapidly over the course of several hours on Day 3 of admission, requiring 6 L oxygen through Hudson mask to maintain oxygen saturation above 90%; however, work of breathing and respiratory symptoms remained relatively stable. This demonstrates the ‘silent hypoxaemia’ that has been commonly seen in COVID‐19 patients. 18 This was similarly seen in Case 6, who presented following a fall at home and had minimal respiratory symptoms and no oxygen requirement on admission. Deterioration occurred on Day 5 of hospital admission (6 days after symptom onset), rapidly requiring 6 L oxygen through Hudson mask to maintain oxygen saturation above 95%. There was no significant respiratory distress or symptoms despite the hypoxaemia. Ongoing deterioration continued and the decision for comfort measures was decided. Case 6 died 14 days after admission.
Clinical outcomes
The median length of stay was 5 days (Table 4). Three patients required readmission after being identified by the CTAC team: one patient for tachycardia, another for increasing dyspnoea and one for severe hypertension. Complications during hospital admission were identified in eight patients and included new onset atrial fibrillation, liver function derangement and acute renal failure.
Table 4.
Inpatient clinical outcomes
| Total (n = 19) | Mild (n = 11) | Severe (n = 6) | Critical (n = 2) | |
|---|---|---|---|---|
| Length of stay, median (IQR) (days) | 5 (3–8) | 3 (2–5) | 8 (6–8) | 28 (21–34)† |
| Complications, n (%) | 8 (42) | 1 (9) | 5 (83) | 2 (100) |
| Readmission, n (%) | 3 (16) | 2 (18) | 1 (17) | 0 |
| Mortality, n (%) | 1 (5) | 0 | 0 | 1 (50) |
†Median (range).
COVID‐19 source
COVID‐19 source (Table 5) was identified for 15 (79%) inpatients, with 10 inpatients having had recent overseas travel either through air travel or cruise and 5 inpatients had close contact with confirmed COVID‐19 cases. Four inpatients had unknown source and were the last few patients admitted into hospital from this cohort. Similarly, the majority of source in the community was from overseas travel (71%), with 17% from a known COVID‐19 contact, 6% from an occupation with high risk of exposure (e.g. bus/Uber driver or airport worker) and 6% with unknown source.
Table 5.
COVID‐19 source
| Source | n (%) |
|---|---|
| Inpatients | |
| Close contact | 5 (26) |
| Travel | 10 (53) |
| Unknown | 4 (21) |
| Community | |
| Close contact | 14 (17) |
| Travel | 58 (71) |
| Occupation | 5 (6) |
| Unknown | 5 (6) |
Discussion
This retrospective case series describes the experience of a major metropolitan hospital in Sydney, including the clinical characteristics, outcomes and community management of COVID‐19 patients. Our comprehensive community‐hospital integrated care model captured deteriorating patients' early review and management.
Determining the source of COVID‐19 cases is important for effective strategies to be undertaken to prevent the rapid growth seen in countries like Italy, which went from 155 cases to 59 000 cases in 4 weeks. 19 Our case series was conducted during the ‘first wave’ and showed that many of the COVID‐19 cases were from overseas travel. Currently, this major source of infection is being managed by the Australian government with all travellers being isolated in mandatory quarantine accommodation for 14 days from arrival 20 and widespread testing. Patients with unknown COVID‐19 source appeared later in our series and likely reflected community transmission. Reducing and containing community transmissions are vitally important particularly as our nation relaxes restrictions and emerges from hibernation. Community COVID‐19 programmes like the Sutherland CTAC team help with the management and safe release of community COVID‐19 patients from quarantine, which assist in reducing community transmission. All of our unknown transmission cases plus an index case in a high‐density accommodation facility were quickly managed to ensure no dissemination took place.
COVID‐19 has caused significant mortality worldwide and has overwhelmed the healthcare system in many countries. The literature is limited regarding how other countries have managed community COVID‐19 patients. China's model of management involved admission of all confirmed COVID‐19 patients regardless of severity. 21 This approach allowed the close monitoring and quarantine of all COVID‐19 patients, but placed great demands on hospital resources. A similar community management model to ours was used in the United States, which included telephonic primary care, telephone triage system, community management group and a respiratory clinic. 22 This system allowed most patients to be managed without hospitalisation, reducing the number of hospital visits and as a consequence was also estimated to reduce the number of personal protective equipment used and exposure to healthcare workers.
In view of the significant healthcare resources required to manage patients with COVID‐19, strategies to reduce unnecessary hospital admissions are important. However, these should be balanced by strategies that can also identify those patients at risk of deterioration, facilitating early review if required. Our CTAC team aimed to achieve this through daily review through telehealth, managing those with mild disease as outpatients, while monitoring for early deterioration and facilitating hospital admission if necessary. This monitoring is particularly important as COVID‐19 patients are known to potentially clinically decline about 1 week after symptom onset. 3 , 14 We chose this pro‐active approach in order to capture deteriorating patients early and to reduce the mortality rate seen worldwide. Given the possibility of ‘silent hypoxaemia’ and potential for respiratory failure in COVID‐19 patients, our CTAC programme also now includes remote monitoring of vital signs (i.e. oxygen saturation and heart rate) for these patients followed in the community. This remote monitoring programme is part of a wider trial currently running within our local health district. This model of care will hopefully be able to identify those patients at risk of deteriorating and also reduce the burden of hospital‐based clinical care.
Our case series has several limitations. The small numbers available for review limits the generalisability of the results to a larger population. These results are also specific to the Sutherland Shire and may not accurately reflect the experience of other local health districts. A comparison of the outcomes and management models of other health districts would be helpful in identifying areas for improvement in our model. In addition, the outcome of patients who were diagnosed by private laboratory and not referred to the CTAC team is unknown. Future directions include the long‐term follow up of the COVID‐19 positive patients and review of how COVID‐19 impacts their lung functions, radiological resolution and return to normal function.
Conclusion
Having a comprehensive inpatient and community model in place to manage COVID‐19 patients is vital in helping reduce the high mortality rate seen worldwide while reducing unnecessary hospital visits. Our case series not only provides the clinical characteristics of COVID‐19 patients in the Sutherland Shire, but also demonstrates how a well prepared management model that incorporates multiple departments, the Public Health Unit and the CTAC team can help successfully defeat this pandemic.
Supporting information
Figure S1 ED pathway for early management of respiratory failure by rapid respiratory team.
Table S1 Inpatient vital signs and investigations.
Funding: None.
Conflict of interest: None.
References
- 1. World Health Organization (WHO) . WHO Timeline – COVID‐19. Geneva, Switzerland: WHO; 2020 [cited 2020 Apr 27]. Available from URL: https://www.who.int/news-room/detail/27-04-2020-who-timeline---covid-19
- 2. Zhou F, Yu T, Du R, Fan G, Liu Y, Zian J et al. Clinical course and risk factors for mortality of adult inpatients with COVID‐19 in Wuhan, China: a retrospective cohort study. Lancet 2020; 395: 1054–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med 2020; 180: 934–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Australian Bureau of Statistics (ABS) . 2016 Census QuickStats Australia. Canberra: ABS; 2019. [cited 2020 May 10]. Available from URL: https://quickstats.censusdata.abs.gov.au/census_services/getproduct/census/2016/quickstat/128?opendocument
- 5. New South Wales Government. HealthStats NSW: coronary heart disease hospitalisation by age . Sydney: NSW Government; 2020. [cited 2020 May 10]. Available from URL: http://www.healthstats.nsw.gov.au/Indicator/cvd_chdhos/cvd_chdhos_lga_trend
- 6. Australian Government Department of Health . Coronavirus (COVID‐19) current situation and case numbers. Sydney: Commonwealth of Australia Department of Health; 2020. [cited 2020 Apr 27]. Available from URL: https://www.health.gov.au/news/health-alerts/novel-coronavirus-2019-ncov-health-alert
- 7. World Health Organization (WHO) . Coronavirus Disease (COVID‐19). Situation Report 105. Geneva, Switzerland; WHO; 2020. [ cited 2020 May 5]. Available from URL: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200504-covid-19-sitrep-105.pdf?sfvrsn=4cdda8af_2
- 8. International Severe Acute Respiratory and emerging Infection Consortium (ISARIC) . COVID‐19 clinical data collection. Oxford, UK: ISARIC; 2020. [cited 2020 May 5]. Available from URL: https://isaric.tghn.org/COVID-19-CRF/ [Google Scholar]
- 9. World Health Organization (WHO) . Clinical management of severe acute respiratory infection (SARI) when COVID‐19 disease is suspected. Geneva, Switzerland: WHO; 2020. [cited 2020 May 27]. Available from URL: https://www.who.int/publications-detail/clinical-management-of-severe-acute-respiratory-infection-when-novel-coronavirus-(ncov)-infection-is-suspected [Google Scholar]
- 10. Wu Z, McGoogan J. Characteristics of and important lessons from the coronavirus disease 2019 (COVID‐19). JAMA 2020; 323: 1239–42. [DOI] [PubMed] [Google Scholar]
- 11. van Doremalen N, Bushmaker T, Morris D, Holbrook M, Gamble A, WIlliamson B et al. Aerosol and surface stability of SARS‐CoV‐2 as compared with SARS‐CoV‐1. N Engl J Med 2020; 382: 1564–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Zuo M, Huang Y, Ma W, Xue Z, Zhang J, Gong Y et al. Expert recommendation for tracheal intubation in critically ill patients with noval coronavirus disease 2019. Chin Med Sci J 2020; 35: 105–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. NSW Government . COVID‐19 cases by notification date and postcode. Sydney: NSW Government; 2020. [cited 2020 May 7]. Available from URL: https://data.nsw.gov.au/data/dataset/covid-19-cases-by-location/resource/21304414-1ff1-4243-a5d2-f52778048b29
- 14. Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2010; 395: 495–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Richardson S, Hirsch J, Narasimhan M, Crawford J, McGinn T, Davidson K. Presenting charactersitics, comorbidities, and outcomes among 5700 patients hospitalised with COVID‐19 in the New York City area. JAMA 2020; 323: 2052–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Sanders J, Monogue M, Jodlowski T, Cutrell J. Pharmacologic treatments for coronavirus disease 2019 (COVID‐19), a review. JAMA 2020; 323: 1824–36. [DOI] [PubMed] [Google Scholar]
- 17. Gautret P, Lagier J, Parola P, Hoang V, Meddeb L, Mailhe M et al. Hydroxychloroquine and azithromycin as a treatment of COVID‐19: results of an open‐label non‐randomised clinical trial. Int J Antimicrob Agents 2020; 56: 106081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Xie J, Tong Z, Guan X, Du B, Qiu H, Slutsky A. Critical care crisis and some recommendation during the COVID‐19 epidemic in China. Intensive Care Med 2020; 46: 837–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Sibble G. Covid‐10 Growth Comparison. COVID.bio; 2020. [cited 2020 Jul 4]. Available from URL: https://covid.bio/growth
- 20. Australian Government Department of Health . Coronavirus (COVID‐19) advice for travellers, Sydney: Commonwealth of Australia Department of Health; 2020. [cited 2020 Jul 10]. Available from URL: https://www.health.gov.au/news/health-alerts/novel-coronavirus-2019-ncov-health-alert/coronavirus-covid-19-advice-for-travellers#travel-to-australia
- 21. First Affliated Hospital Zhejiang University School of Medicine (FAHZU) . Handbook of COVID‐19 Prevention and Treatment. Hangzhou, China: FAHZU; 2020. [cited 2020 May 30]. Available from URL: https://cm-us-standard.s3.amazonaws.com/documents/Zhejiang-University-Handbook-of-COVID-19-Prevention-and-Treatment.pdf [Google Scholar]
- 22. John J, Zallman L, Blau J. Our hospital's community management strategy for COVID‐19 works. Yours can, too. Boston, MA: STAT News; 2020. [cited 2020 May 30]. Available from URL: https://www.statnews.com/2020/04/23/community-management-strategy-for-covid-19-works/ [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1 ED pathway for early management of respiratory failure by rapid respiratory team.
Table S1 Inpatient vital signs and investigations.


