ABSTRACT
Background
Little is known about the lived experiences of individuals with tic disorders when driving vehicles or trying to obtain a driving license.
Objective
To survey the driving‐related experiences of adults with tic disorders.
Methods
A global survey was disseminated via social media, international patient organizations, and experts between April 27, 2020 and July 20, 2020.
Results
Participants were 228 adult individuals self‐reporting a confirmed diagnosis of Tourette syndrome or chronic tic disorder. Of these, 183 (87.7%) had a driver's license. A minority (9%) reported that they had found it hard to pass the driving test. Tics only interfered with driving “a bit” (58.5%) or “not at all” (33%). A majority of participants reported being able to suppress their tics (39.5%) or that their tics are unchanged (28.5%) while driving. Nearly half of the participants (46.5%) had been involved in accidents, but only a negligible percentage (3.2%) considered that these were linked to the tics. Participants without a driver's license (n = 28, 12.3%) reported significantly more severe tics, compared to those with a license. The majority of these (60.7%) identified their tics as the main reason for not having a license and 64.3% said that they would like to receive support to obtain one.
Conclusions
The majority of surveyed participants with chronic tic disorders reported minimal difficulties with driving. However, a non‐negligible minority of more severe cases struggle with driving or refrain from driving altogether and would benefit from additional support. The results have implications for clinicians and vehicle licensing agencies.
Keywords: tic disorders, Tourette syndrome, chronic tic disorder, driving, motor vehicles, licensing agencies
Tourette syndrome (TS) and chronic tic disorder (CTD) are childhood‐onset movement disorders characterized by multiple motor and/or vocal tics persisting for more than 1 year. 1 Whether tics interfere with driving and constitute a safety risk is an important research question that remains poorly explored. In some countries, like Sweden or the United Kingdom, individuals with TS are encouraged or required to report their diagnosis to their licensing authorities, particularly if they feel that their tics interfere with driving. 2 , 3 A large Swedish population‐based study 4 found that individuals with TS/CTD (n = 3450) had a small increased risk of serious transport accidents, compared to individuals from the general population, but the risk was largely explained by the presence of comorbid attention‐deficit/hyperactivity disorder (ADHD). However, the study could not determine if individuals with TS/CTD are less likely to obtain a driving license or simply refrain from driving because of their tics. Data on the driving experiences of persons with TS/CTD and whether they perceive particular challenges when obtaining a driving license are lacking. Here, we partnered with the leading charity Tourettes Action to design a global survey to capture the driving experiences of adults with TS/CTD.
Methods
The Swedish Ethics Review authority determined that the study was exempt from ethical review according to Swedish law because participation in the survey was anonymous and no sensitive personal data was stored. Participants consented to participate in the study. They were asked to confirm that they were 18 years old or over and that they understood that their anonymous data would be used for research purposes.
Survey Design
An online survey was developed, with feedback from Tourettes Action, and hosted at www.surveygizmo.com. The survey took approximately 10 to 15 minutes to complete and consisted of both multiple‐choice and open‐ended questions (see Supporting Information).
The survey included several sections. The first section gathered information on sociodemographic (gender, age group, and country) and clinical characteristics, including comorbidities and current tic severity, measured with the Adult Tic Questionnaire (ATQ). 5 The ATQ is a self‐report questionnaire that provides intensity and severity scores for 27 specific vocal and motor tics. Scores can be summed to produce a total tic severity score (range = 0–216). The ATQ has adequate psychometric properties. 5
The next section asked whether the person had a driver's license. A skip logic algorithm showed 1 of 2 different sets of questions depending on whether the answer was affirmative or negative. Participants with a driver's license were asked about the process of obtaining the license, the interference caused by the tics and/or comorbidities when driving, whether the treatment for tics and/or comorbidities impacted their driving, traffic accidents, road rage and dangerous behaviors when driving, and their perceived need for support with their driving. Participants without a driver's license were asked whether not having a license was related to their tics or other comorbidities, previous attempts or plans to get a license, and the perceived need of support to obtain a license.
Participants and Procedure
Recruitment was done by distributing a link to the online survey via social media (eg, Reddit, Twitter, and Facebook) and by emailing it to patient organizations and international TS experts that could share the link among colleagues and patients.
The survey was open to participants from any country who could read in English. A minimum reported age of 18 years, consent to participate in the study, and a self‐reported confirmed diagnosis of TS or CTD were required for participation. The survey was open from April 27, 2020 to July 20, 2020.
Statistical Analyses
The completed surveys were downloaded into a Microsoft Excel spreadsheet and data managed and analyzed in Stata, version 13.1 (StataCorp LLC, College Station, TX). Frequencies and percentages for each question were calculated for the whole sample and separately for the participants with and without a driver's license. Further, because previous literature has reported a small increased risk of traffic accidents in TS/CTD mainly driven by ADHD comorbidity, 4 analyses were repeated stratifying by the presence or absence of ADHD in those with a driver's license.
χ2 and Student's t tests were used as appropriate to compare groups. All tests used 2‐tailed significance set at P < 0.05. Common themes were extracted from the open‐ended questions and summarized.
Results
Survey Participants
Figure 1 shows the flow of participants. The final sample consisted of 228 individuals. Their demographic and clinical characteristics are shown in Table 1. A substantial majority of participants (75%) reported comorbid psychiatric disorders. Insomnia was reported by 14.9% of the sample. The ATQ score was 51.9 (SD = 31.2), with a reasonable representation of tic severities (range 0–184).
FIG. 1.
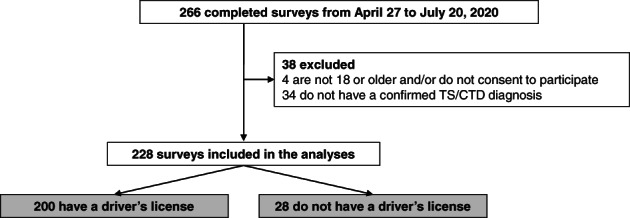
Flow of survey participants. CTD, chronic tic disorder; TS, Tourette syndrome.
TABLE 1.
Demographic and clinical characteristics of the survey participants (N = 228), by driving license status
| All participants N = 228 | Participants with a driver's license n = 200 (87.7%) | Participants without a driver's license n = 28 (12.3%) | |
|---|---|---|---|
| Demographic variables | |||
| Gender* | |||
| Woman | 130 (57.0) | 114 (57.0) | 16 (57.1) |
| Man | 93 (40.8) | 85 (42.5) | 8 (28.6) |
| Other/prefer not to say | 5 (2.2) | 1 (0.5) | 4 (14.3) |
| Age group* | |||
| 18–25 yr | 98 (43.0) | 77 (38.5) | 21 (75.0) |
| 26–35 yr | 59 (25.9) | 56 (28.0) | 3 (10.7) |
| 36–45 yr | 36 (15.8) | 34 (17.0) | 2 (7.1) |
| 46–55 yr | 23 (10.1) | 21 (10.5) | 2 (7.1) |
| 56 yr or older | 12 (5.3) | 12 (6.0) | 0 (0) |
| Country ** | |||
| United States | 66 (28.9) | 62 (31.0) | 4 (14.3) |
| Norway | 42 (18.4) | 40 (20.0) | 2 (7.1) |
| United Kingdom | 40 (17.5) | 32 (16.0) | 8 (28.6) |
| Canada | 13 (5.7) | 8 (4.0) | 5 (17.9) |
| Sweden | 12 (5.3) | 11 (5.5) | 1 (3.6) |
| The Netherlands | 11 (4.8) | 11 (5.5) | 0 (0) |
| Germany | 11 (4.8) | 9 (4.5) | 2 (7.1) |
| Other countries | 33 (14.5) | 27 (13.5) | 6 (21.4) |
| Clinical variables | |||
| Any psychiatric comorbidity | 171 (75.0) | 146 (73.0) | 25 (89.3) |
| Attention‐deficit/hyperactivity disorder | 79 (34.6) | 66 (33.0) | 13 (46.4) |
| Obsessive–compulsive disorder | 87 (38.2) | 73 (36.5) | 14 (50.0) |
| Anxiety disorder | 98 (43.0) | 82 (41.0) | 16 (57.1) |
| Depression | 81 (35.5) | 70 (35.0) | 11 (39.3) |
| Autism spectrum disorder* | 23 (10.1) | 16 (8.0) | 7 (25.0) |
| Other | 13 (5.7) | 11 (5.5) | 2 (7.1) |
| Insomnia | 34 (14.9) | 32 (16.0) | 2 (7.1) |
| ATQ total score, mean (SD)* | 51.9 (31.2) | 49.6 (29.4) | 68.6 (38.1) |
| ATQ motor tics scale, mean (SD)* | 33.6 (17.7) | 32.5 (17.1) | 41.3 (20.8) |
| ATQ vocal tics scale, mean (SD)* | 18.3 (16.5) | 17.1 (15.7) | 27.3 (19.4) |
Figures correspond to frequencies (percentages), unless otherwise specified.
Indicates statistically significant differences between participants with and without driver's license in χ2 tests (all categorical variables) and Student's t tests (ATQ variables) at P < 0.05.
Only the countries endorsed by more than 10 participants (when all 228 participants are taken into account) are listed. The rest of countries are grouped under “Other.”
ATQ, Adult Tic Questionnaire; SD, standard deviation.
Of the 228 participants, 200 (87.7%) reported having a driver's license. There were significant differences between those with and without a driver's license in gender (χ2 = 22.453, P < 0.001) and age group (χ2 = 13.915, P = 0.008). Specifically, those without a driver's license defined themselves more often as “other gender” or “preferred not to say” and tended to be younger (Table 1). For the clinical variables, there was a significantly higher proportion of individuals with autism spectrum disorder in the group without, compared to the group with, a driver's license (χ2 = 7.826, P = 0.005). Additionally, participants without a driver's license reported more severe tics than those with a license (ATQ score: t test = 3.081, P = 0.002; Table 1).
Participants with a Driver's License
About the Process of Obtaining a Driver's License
Of the 200 participants with a driver's license, only 18 (9%) responded that it was hard for them to pass the test (Table 2). A minority (n = 29; 14.5%) said that they had been obligated to disclose their diagnosis to the driving licensing agency. These individuals were spread across a number of countries including 9 in the United Kingdom (31.0%), 7 in Norway (24.1%), 4 in Sweden (13.8%), 3 in the United States (10.3%), 2 in the Netherlands (6.9%), and 1 each (3.4%) in Australia, Canada, Finland, and Ireland. For 26 individuals (13%), a doctor had to write a report supporting their application. In 10 cases (5%), the doctor or the licensing agency had told them that they could not drive because of the tics, and in 5 cases (2.5%) the license was revoked because of the tics.
TABLE 2.
Survey answers of those participants with Tourette syndrome or chronic tic disorder who have a driver's license (n = 200)
| n (%) | |
|---|---|
| About obtaining a driver's license | |
| Age when the license was obtained | |
| Younger than 18 yr | 67 (34.0) |
| 18–25 yr | 111 (56.3) |
| 26–35 yr | 14 (7.1) |
| 36–45 yr | 5 (2.5) |
| Found it hard to pass the test due to the tics | 18 (9.0) |
| Was obligated to disclose the TS diagnosis to the licensing agency | 29 (14.5) |
| Doctor had to write a report supporting the application | 26 (13.0) |
| Doctor or diving agency told them that could not drive due to the tics | 10 (5.0) |
| Driver's license has been revoked at some point due to the tics | 5 (2.5) |
| About the driving experience and the impact of comorbidities | |
| Drive regularly | 177 (88.5) |
| What happens to the tics when they drive | |
| Can suppress tics when they drive | 79 (39.5) |
| Tics are unchanged when they drive | 57 (28.5) |
| Tics get worse when they drive | 28 (14.0) |
| Other | 36 (18.0) |
| How much do the tics interfere with driving | |
| Not at all (they drive normally) | 66 (33.0) |
| A bit (tics sometimes interfere with driving) | 117 (58.5) |
| Quite a bit (can drive but with difficulty due to the tics) | 11 (5.5) |
| Extremely (tics make the driving unsafe) | 6 (3.0) |
| What problem interferes the most with the driving | |
| The tics | 49 (24.5) |
| Attention‐deficit/hyperactivity disorder | 75 (37.5) |
| Obsessive–compulsive disorder | 16 (8.0) |
| Autism spectrum disorder | 20 (10.0) |
| Anxiety disorder | 1 (0.5) |
| Depression | 19 (9.5) |
| Insomnia | 3 (1.5) |
| Other problem | 2 (1.0) |
| The driving is not at all impaired | 15 (7.5) |
| About traffic accidents and road rage | |
| Has been involved in a traffic accident while driving | 93 (46.5) |
| The tics had something to do with this/these accident(s) | 3 (3.2) |
| Get angry or frustrated when driving | |
| Never | 3 (1.5) |
| Rarely | 20 (10.0) |
| Often | 105 (52.5) |
| All the time | 56 (28.0) |
| They do not drive | 16 (8.0) |
| Experience road rage when they drive | |
| Never | 3 (1.5) |
| Rarely | 92 (46.0) |
| Often | 71 (35.5) |
| All the time | 27 (13.5) |
| They do not drive | 7 (3.5) |
| Feel that they do things that are a bit dangerous when driving | |
| Never | 3 (1.5) |
| Rarely | 79 (39.5) |
| Often | 97 (48.5) |
| All the time | 18 (9.0) |
| They do not drive | 3 (1.5) |
| About support | |
| Feel that they need support for their driving | 13 (6.5) |
TS, Tourette syndrome.
The open‐ended question revealed a few common themes. Many participants reported not having developed symptoms or that the tics were not affecting them substantially at the time they got their license. Some participants did not disclose their diagnosis and/or purposely tried to hide it during the driving lessons or the exam because of the fear that the symptoms would hinder their chances of getting the license or because of the economic costs associated with obtaining a medical report that certified them fit for driving. Other participants reported that other psychiatric and somatic comorbidities (eg, anxiety, ADHD, epilepsy, and vision problems), rather than the tics, played a more relevant role when they applied for the license.
About the Driving Experience and the Impact of Comorbidities
As reported in Table 2, the vast majority of respondents reported driving regularly (n = 177, 88.5%). These, compared to those that did not drive regularly, had a similar proportion of psychiatric comorbidities (n = 128, 72.3% vs. n = 18, 78.3%, respectively; χ2 = 0.365, P = 0.546), but scored lower in tic severity (mean [SD] ATQ score: 47.8 [2.0] vs. 62.9 [9.6], respectively; t test = −2.327, P = 0.021).
More than two‐thirds of the drivers reported that, when they drive, their tics either can be suppressed (n = 79, 39.5%) or are unchanged (n = 57, 28.5%). However, 14% (n = 28) of the participants reported that their tics get worse when driving. The rest of respondents (“other” category: n = 36, 18%) reported that their tics decrease, but are not completely suppressed, or a mixture of responses, with tics manifesting differently when they drive, mostly depending on levels of stress or anxiety. Others expressed that they can “adapt” the tics to the driving so that they will not interfere (eg, twitching right arm instead of right leg that would affect the gas pedal).
The majority of the sample reported that, overall, their tics either do not interfere with driving (n = 66, 33%) or they do so only a bit (n = 117, 58.5%). Some participants highlighted their ability to “self‐regulate” in a way that when tics are worse or more intense, they refrain from driving for a period or are able to pull over, if the symptoms arise while they are driving. Some individuals mentioned that, because of the interference of the tics, they try to drive only when necessary or for short distances or ask a relative or a friend to drive them to places. Specific tics, like those related to the eyes or the head, were mentioned as being the most interfering.
When asked about the problem that interfered the most with their driving, one‐fourth mentioned the tics (n = 49, 24.5%), but a larger proportion mentioned ADHD symptoms as the main problem (n = 75, 37.5%). Other comorbidities seemed to be less problematic (Table 2).
About Traffic Accidents and Road Rage
Less than half of the sample (n = 93, 46.5%) reported to have previously been involved in a traffic accident while being in the driving seat. Of these, only 3 (3.2%) mentioned that their tics had something to do with the accident (Table 2).
A large majority of participants reported that they get angry and frustrated when driving (all the time: n = 56, 28%; often: n = 105, 52.5%). A lower but still significant proportion reported that they experience road rage (eg, performing rude and offensive gestures, uttering insults, and using dangerous driving moves) when they drive (all the time: n = 27, 13.5%; often: n = 71, 35.5%) and that they feel that they do things that are a bit dangerous when driving, like speeding too much or racing other drivers (all the time: n = 18, 9%; often: n = 97, 48.5%; Table 2).
Treatment and Interference with Driving
One‐fourth of the sample (n = 51, 25.5%) were on medication for their tics, whereas almost half (n = 99, 49.5%) were on medication for other reasons. Approximately one‐third (n = 65, 32.5%) reported having received behavioral treatment for their tics (Table 3).
TABLE 3.
Treatment and impact of treatment on driving of those participants with Tourette syndrome or chronic tic disorder who have a driver's license (n = 200)
| n (%) | |
|---|---|
| Type of treatment | |
| On medication for the tics | 51 (25.5) |
| Antipsychotics | 23 (11.5) |
| Guanfacine | 5 (2.5) |
| Other | 27 (13.5) |
| On medication for other reasons | 99 (49.5) |
| For attention‐deficit/hyperactivity disorder | 20 (10.0) |
| For obsessive–compulsive disorder | 17 (8.5) |
| For anxiety and/or depression | 53 (26.5) |
| For insomnia | 17 (8.5) |
| For other problems | 40 (20.0) |
| Previous behavioral treatment for the tics | 65 (32.5) |
| Treatment and driving | |
| Medication for the tics affects the driving | |
| Yes, helps with the driving | 20 (39.2) |
| Yes, impairs the driving | 9 (17.7) |
| No, does not affect the driving | 22 (43.1) |
| Medication for other reasons affects the driving | |
| Yes, helps with the driving | 17 (17.2) |
| Yes, impairs the driving | 9 (9.1) |
| No, does not affect the driving | 73 (73.7) |
| Behavioral treatment for the tics affects the driving | |
| Yes, helps with the driving | 14 (21.5) |
| Yes, impairs the driving | 0 (0) |
| No, does not affect the driving | 51 (78.5) |
For all treatments, including medication for the tics, medication for other reasons, and behavioral treatment for the tics, participants reported that they did not affect their driving (in 43.1%, 73.7%, and 78.5% of the cases, respectively) or that these treatments helped with the driving (in 39.2%, 17.2%, and 21.5% of the cases, respectively). Smaller numbers of participants reported that the medication impaired their driving (17.7% for medication for the tics and 9.1% for medication for other reasons).
Need of Support for their Driving
A small percentage of participants (n = 13, 6.5%) reported that they feel they need support for their driving. For these, the main ways they could be supported included having someone in the car when they are driving who can provide reassurance and reduce anxiety and having someone to rely on to take them to places when the tics are too severe for them to drive. Other topics included improving driving instructors’ knowledge of tics, so they are not negatively judged, and learning themselves to identify when the tics might be too severe to drive.
Participants without a Driver's License
About Obtaining a Driver's License
The majority of the 28 individuals with TS/CTD who reported not to have a driver's license (Table 4) attributed this to their tics (n = 17, 60.7%). Others reported that they did not have a license because of other problems (eg, anxiety disorders, ADHD).
TABLE 4.
Survey answers of those participants with Tourette syndrome or chronic tic disorder who do not have a driver's license (n = 28)
| n (%) | |
|---|---|
| About obtaining a driver's license | |
| Do not have a driver's license because of the tics | 17 (60.7) |
| Do not have a driver's license because of other problems | |
| Because of the attention‐deficit/hyperactivity disorder | 6 (21.4) |
| Because of the obsessive–compulsive disorder | 4 (14.3) |
| Because of the anxiety disorder | 9 (32.1) |
| Because of the depression | 2 (7.1) |
| Because of the insomnia | 0 (0) |
| Because of another psychiatric disorder | 2 (7.1) |
| Does not have to do with any psychiatric disorder | 8 (28.6) |
| Does not have psychiatric comorbidities | 3 (10.7) |
| Application for driver's license was denied because of the tics | 1 (3.6) |
| Think it was a fair decision that the application was denied | 1 (100) |
| Planning on getting a driver's license in the future | 18 (64.3) |
| Worried that tics will make it hard to get a driver's license | 14 (77.8) |
| How difficult it would be to obtain a driver's license | |
| Easier than for other people | 0 (0) |
| About the same than for other people | 6 (33.3) |
| Harder than for other people | 7 (38.9) |
| Much harder than for other people | 5 (27.8) |
| About support | |
| Feel that they need support to obtain a driver's license | 18 (64.3) |
Only 1 person (3.6%) reported that their application for a driver's license was denied because of their tics, but also reported feeling that this decision was fair. A majority (n = 18, 64.3%) reported plans to get a driver's license in the future and, of these, 14 (77.8%) were worried that their tics would make it hard to obtain it. Two‐thirds of these individuals reported that, for them, getting a driver's license would be much harder or harder (n = 12, 67.7%) than for other people (Table 4).
Need of Support to Obtain a Driver's License
Eighteen of the 28 individuals in this sample (64.3%) reported that they feel they need support to obtain a driver's license. Among the most common themes identified in the open‐ended question were the need to increase the awareness and understanding of the condition among driving instructors and examiners, because their lack of knowledge may lead to individuals being more self‐aware of their tics or may add pressure and stress, making the tics more severe or more noticeable. Other aspects mentioned included more social support while studying for the license or when learning to drive and getting additional help for their psychiatric comorbidities.
Are Driving Experiences Different for Those with and without ADHD Comorbidity?
Among the 200 individuals with a driver's license, 66 (33%) reported a comorbid ADHD diagnosis. Those with ADHD, compared to those without, had a significantly higher proportion of “any psychiatric comorbidity” (n = 51, 77.3% vs. n = 80, 59.7%, respectively; χ2 = 6.042, P = 0.014), as well as a higher proportion of obsessive–compulsive disorder (n = 31, 47% vs. n = 42, 31.3%; χ2 = 4.659, P = 0.031). Those with ADHD, compared to those without, reported more severe ATQ scores (mean [SD]: 59.1 [4.3] vs. 44.9 [2.2], respectively; t test = −3.296, P = 0.001).
Those with ADHD obtained their driver's license later than those without ADHD (χ2 = 9.245, P = 0.026), with more individuals with ADHD obtaining it at ages 26 to 35, compared to the younger age group. Additionally, those with ADHD, compared to those without, reported more often that they required a doctor's report to get their license (19.7% vs. 9.7%, respectively; χ2 = 3.906, P = 0.048). All 5 individuals in the sample that reported that their driver's license had been revoked had ADHD (7.6% vs. 0%; χ2 = 10.412, P = 0.001).
Those with ADHD reported driving as regularly as those without ADHD (89.4% vs. 88.1%, respectively; χ2 = 0.077, P = 0.781). Similarly, there were no group differences regarding how the tics varied while driving (ie, if they were suppressed, unchanged or got worse; χ2 = 1.159, P = 0.763) or regarding the interference caused by the tics when driving (χ2 = 2.304, P = 0.512).
There were no significant differences between those with and without ADHD in the number of reported traffic accidents (40.9% vs. 49.2%, respectively; χ2 = 1.238, P = 0.266). Those with ADHD did not report experiencing more anger, road rage, or dangerous driving, compared to those without ADHD (χ2 = 1.043, P = 0.791; χ2 = 4.391, P = 0.222; χ2 = 3.753, P = 0.289, respectively). Those with ADHD, compared to those without, reported more frequently that they need support with driving (12.3% vs. 3.8%; χ2 = 4.915, P = 0.027).
A similar proportion of individuals with and without ADHD were on medication for their tics (18.2% vs. 29.10; χ2 = 2.777, P = 0.096). Both groups reported a similar proportion of use of other medications, however, as expected, all 20 people on ADHD drugs reported to have the diagnosis (54.0% vs. 0%; χ2 = 44.272, P < 0.001). Medication for problems other than tics affected differently those with and without ADHD (χ2 = 10.606, P = 0.005). Those with ADHD were more likely to report that these medications helped with, rather than impaired, their driving (χ2 = 5.539, P = 0.019).
Discussion
This study sheds unique light on the lived experiences of individuals with tic disorders and identifies some areas for future research and specific recommendations for clinicians and vehicle licensing agencies.
A majority of participants in this study reported having a driver's license. Approximately 90% of these reported that passing the test was not hard and that they drive regularly. A majority reported that their tics do not interfere with their driving or that they do so only a bit, with the tics remaining unchanged or being successfully suppressed when they drive. In most cases, tics are highly dependent on mental state, activity, and external environment, classically worse with stress and better when absorbed in a task such as playing music, sports, or video games. These effects are variable from person to person. Clinical observation suggests that driving can be associated with a decrease as well as an increase in tics, as also indicated by our results. Approximately half of the sample reported to have been involved in traffic accidents before, but only 3 individuals attributed these to the tics. When asked about the problem that interfered the most with their driving, approximately a quarter mentioned the tics, although ADHD, if present, was perceived as being more interfering. Based on these results, the majority of participants in our survey were generally able to obtain a driver's license and drive without significant interference from the tics.
Despite this generally positive picture, a smaller proportion of individuals did report difficulties when driving or refrained from driving altogether. Approximately 14% of the participants reported that their tics are worse when driving and ~12% of individuals with a driver's license reported not driving regularly; these individuals had significantly higher tic severity. In fact, this ability to “self‐regulate” was reported by several participants, who indicated that they would not drive or would stop the car if they perceived that their symptoms were too severe or too interfering. A smaller proportion of respondents (~6%) reported needing additional support for their driving.
A small proportion of participants (12.3%) did not have a driver's license, and 61% of these blamed their tics for it. Those without a license had significantly more severe tics. Although a majority of these individuals had plans to get a license in the future, they anticipated that it would be hard to obtain it because of their tics and wished for additional support to get it.
We found relatively few differences between participants with and without comorbid ADHD. Interestingly, although those with ADHD had more severe tics than those without, there were no between‐group differences in the degree of interference of the tics while driving, number of traffic accidents or in expressing more anger, road rage, or violent behaviors when driving. On the other hand, individuals with tics and ADHD reported needing more support with their driving. Of note, all 5 individuals that indicated that their license had been revoked had ADHD. Together with our previous epidemiological findings, 4 the results suggest that individuals with comorbidities that are known to potentially interfere with driving (ie, ADHD) 6 may require additional support.
Although direct comparisons are difficult because of the idiosyncratic nature of our survey, which was specifically designed for individuals with tic disorders, our results echo the findings of previous driving studies in individuals with other neuropsychiatric disorders, such as ADHD, 6 , 7 autism spectrum disorders8, 9 or depression. 10 , 11
Assuming that the results are generalizable to the larger population of adults with tic disorders, our findings have some implications for both clinicians and licensing agencies. Clinicians should be aware that some of their patients might struggle with driving or encounter obstacles when trying to obtain a driver's license. Adequate long‐term management and treatment of the tics and associated comorbidities is a good starting point. A substantial proportion of survey participants reported that the treatments they were receiving for their tics (medication or behavioral treatment) were helpful with their driving. It is not known if treatment can successfully allow driving in some individuals initially not able or licensed to drive because of their tics.
A non‐negligible 15% of those with a driver's license stated that they were obligated to disclose their TS/CTD diagnosis to the licensing agency in their country. For a similar proportion, a doctor was required to write a report to support their application. In light of our results, it may be timely for licensing agencies in some countries to reconsider the need for applicants with TS/CTD to report on their health status given that empirical evidence suggests that, for the vast majority, tics do not necessarily interfere with the safety of their driving. In relation to this, a number of survey participants suggested that it would be helpful for driving instructors and examiners to be more aware of tic disorders. This may help avoiding negative judgment and attitudes that may inadvertently lead sufferers to become more aware of their symptoms, leading in turn to increased stress and tic outbursts that can make driving more difficult, for example, during their driving test. In general, decisions on whether or not to grant a driver's license should not be done based on the diagnosis of TS/CTD itself but on an individual assessment of the individual in question.
The highest threat to the validity of our results is the non‐probabilistic sampling method. Although a lower prevalence risk ratio for sex is expected in adults compared to children with TS, 12 our sample still included a higher than expected proportion of women (57%). Most participants were from Europe and North America and the results may not generalize to other populations. The accuracy of the diagnoses could not be verified and, therefore, our sample may contain individuals with both primary and functional tic disorders. Statistical power was limited for some of the analyses. Finally, the study lacked a control group, which makes it difficult to put some of the findings in context (eg, road rage, accidents).
In sum, and with these caveats in mind, we found that the majority of surveyed participants with TS/CTD reported minimal difficulties with driving. However, a non‐negligible minority of more severe cases struggle with driving or refrain from driving altogether and would benefit from additional support. Clinicians and licensing agencies should be aware of these struggles and assess safety risks related to driving on an individual basis.
Author Roles
(1) Research project: A. Conception, B. Organization, C. Execution; (2) Statistical Analysis: A. Design, B. Execution, C. Review and Critique; (3) Manuscript: A. Writing of the first draft, B. Review and Critique.
D.M‐C.: 1A, 1B, 1C, 2A, 2C, 3A
H.R.: 1A, 1B, 1C, 2C, 3B
S.A.: 1A, 2C, 3B
J.S.S.: 1A, 2C, 3B
L.F.C.: 1A, 1B, 1C, 2A, 2B, 3B
Disclosures
Ethical Compliance Statement
The authors confirm that the approval of the Swedish Ethics Review authority was not required for this work because participation in the survey is anonymous and no personal data was stored. Participants consented to participate in the study. They were asked to confirm that they were 18 or over and that they understood that their anonymous data would be used for research purposes. We confirm that we have read the Journal's position on issues involved in ethical publication and affirm that this work is consistent with those guidelines.
Funding Sources and Conflicts of Interest
No specific funding was available for this project. The authors declare no conflicts of interest.
Financial Disclosures for Previous 12 months
L.F.C. receives royalties for contributing articles to UpToDate, Wolters Kluwer Health, outside the submitted work. D.M‐C. receives royalties for contributing articles to UpToDate, Wolters Kluwer Health and for editorial work from Elsevier, all outside the submitted work.
Supporting information
Supplement 1. Online survey.
References
- 1. American Psychiatric Association . The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM‐5). Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- 2. GOV.UK . Tourette's syndrome and driving. https://www.gov.uk/tourettes-syndrome-and-driving. 2020. Accessed September 9, 2020.
- 3. Vägverkets författningssamling [Swedish Transport Administration] . Vägverkets föreskrifter om medicinska krav för innehav av körkort m.m. [The Swedish Transport Administration's regulations on medical requirements for holding a driving license]. Borlänge: Vägverkets författningssamling; 2008. [Google Scholar]
- 4. Mataix‐Cols D, Brander G, Chang Z, et al. Serious transport accidents in Tourette syndrome or chronic tic disorder. Mov Disord 2021; 36:188–195. 10.1002/mds.28301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Abramovitch A, Reese H, Woods DW, et al. Psychometric properties of a self‐report instrument for the assessment of tic severity in adults with tic disorders. Behav Ther 2015;46(6):786–796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Chang Z, Lichtenstein P, D'Onofrio BM, Sjolander A, Larsson H. Serious transport accidents in adults with attention‐deficit/hyperactivity disorder and the effect of medication: a population‐based study. JAMA Psychiat 2014;71(3):319–325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Barkley RA, Cox D. A review of driving risks and impairments associated with attention‐deficit/hyperactivity disorder and the effects of stimulant medication on driving performance. J Safety Res 2007;38(1):113–128. [DOI] [PubMed] [Google Scholar]
- 8. Daly BP, Nicholls EG, Patrick KE, Brinckman DD, Schultheis MT. Driving behaviors in adults with autism spectrum disorders. J Autism Dev Disord 2014;44(12):3119–3128. [DOI] [PubMed] [Google Scholar]
- 9. Wilson NJ, Lee HC, Vaz S, Vindin P, Cordier R. Scoping review of the driving behaviour of and driver training programs for people on the autism spectrum. Behav Neurol 2018;2018:6842306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. van der Sluiszen NNJJM, Wingen M, Vermeeren A, Vinckenbosch F, Jongen S, Ramaekers JG. Driving performance of depressed patients who are untreated or receive long‐term antidepressant (SSRI/SNRI) treatment. Pharmacopsychiatry 2017;50(5):182–188. [DOI] [PubMed] [Google Scholar]
- 11. Wingen M, Ramaekers JG, Schmitt JAJ. Driving impairment in depressed patients receiving long‐term antidepressant treatment. Psychopharmacology (Berl) 2006;188(1):84–91. [DOI] [PubMed] [Google Scholar]
- 12. Yang J, Hirsch L, Martino D, Jette N, Roberts J, Pringsheim T. The prevalence of diagnosed Tourette syndrome in Canada: a national population‐based study. Mov Disord 2016;31(11):1658–1663. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplement 1. Online survey.


