Abstract
Background
Simple anal fistula is one of the most common causes of proctological surgery and fistulotomy is considered the gold standard. This procedure, however, may cause complications. The aim of this systematic review was to assess the surgical treatment of simple anal fistula with traditional and sphincter-sparing techniques.
Methods
A literature research was performed using PubMed, Cochrane, and Google Scholar to identify studies on the surgical treatment of simple anal fistulas. Observational studies and randomized clinical trials were included. We assessed the risk of bias of included studies using the Jadad scale for randomized controlled trials, and the MINORS Scale for the remaining studies.
Results
The search returned 456 records, and 66 studies were found to be eligible. The quality of the studies was generally low. A total of 4883 patients with a simple anal fistula underwent a sphincter-cutting procedure, mainly fistulotomy, with a weighted average healing rate of 93.7%, while any postoperative continence impairment was reported in 12.7% of patients. Sphincter-sparing techniques were adopted to treat 602 patients affected by simple anal fistula, reaching a weighted average success rate of 77.7%, with no study reporting a significant postoperative incontinence rate. The postoperative onset of fecal incontinence and the recurrence of the disease reduced patients’ quality of life and satisfaction.
Conclusions
Surgical treatment of simple anal fistulas with sphincter-cutting procedures provides excellent cure rates, even if postoperative fecal incontinence is not a negligible risk. A sphincter-sparing procedure could be useful in selected patients.
Keywords: Simple anal fistula, Fistula-in-ano, Fistulotomy, Incontinence
Introduction
Anal fistula (AF), one of the most common causes of proctological surgery [1], is a condition that can have impact on patients’ anorectal function and quality of life (QoL) [2].
The classification of AFs into “simple” or “complex” has the greatest practical and surgical significance. Usually, the majority of simple AFs are considered to have “low” tracts. However, the definition of low fistula has changed over time, with a trend towards lowering the percentage of the external anal sphincter (EAS) crossed by the fistula tract [3]. According to several guidelines [4–6], an AF is defined “simple” when the tract is intersphincteric, or low transsphincteric (crossing < 30% of the EAS). Instead, AFs are defined as complex in cases of––high transphincteric tract (crossing > 30% of the EAS); in patients considered at risk for postoperative fecal incontinence (anterior fistula in women, recurrent fistula, or pre-existent fecal incontinence) even though with low transphincteric tract; suprasphincteric or extrasphincteric tracts; and in AFs with multiple tracts in a horseshoe fashion or those associated with inflammatory bowel disease (IBD), radiation, malignancy, tuberculosis, or chronic diarrhea [4–6].
Surgical treatment of AFs is therefore usually based on the amount of the sphincters involved, and, based on this concept, anal fistulotomy is considered the gold standard to treat simple AFs. This procedure, however, may have side effects such as deformities and esthetic alterations [7], together with detrimental effects on continence and on patient satisfaction [2, 4–8].
For these reasons, several minimally invasive techniques have been developed, even if their adoption (mainly in simple AFs) is limited by a higher failure rate. They also tend to be more expensive and are rarely used in real practice scenarios [9]. Reflecting this, guidelines do not offer specific indications regarding the clinical application of these techniques in simple AFs [4–6].
The aim of this systematic review was to assess the surgical treatment of simple AFs by sphincter-cutting and sphincter-sparing techniques, and specifically—(1) peri-operative features and morbidity, (2) clinical results in terms of efficacy, (3) the risk of postoperative continence impairment and impact of surgery on patients’ QoL.
Materials and methods
Literature review and eligibility criteria
This review was carried out according to the Preferred Reporting Items for Systematic reviews and Meta-Analyses Statement (PRISMA) guidelines [10]. A literature research was performed using PubMed, Cochrane, and Google Scholar. “Simple anal fistula”, “low anal fistula”, “intersphincteric fistula”, “low transphincteric fistula”, “fistulotomy” were the search terms used. Studies were included if they provided any number of cases analyzing any surgical treatment for simple AFs as defined by commonly adopted guidelines [4–6]. Prospective, retrospective, observational studies, and randomized clinical trials were included, while reviews, meta-analyses, trial proposals, thesis articles, technical notes, commentaries, letters, and meeting abstracts were excluded. The time range covered was 1990–April 2020, and only articles written in English were selected. Additional articles responding to the inclusion criteria were extrapolated from the bibliography of relevant material via backward citation tracking.
All articles concerning complex, recto-vaginal or ano-vaginal, tuberculosis- and IBD-related AFs were excluded, as well as any study where data on simple AFs could not be extrapolated.
Database research was performed by three authors individually (FL, AP, LF) and the results were then discussed and merged by a working group. Article inclusion, when in doubt, was decided on a per-case basis after discussion.
Data extraction
Data from eligible literature was thus extracted and inserted in tables using SPSS® version 21.0 for Windows® software (SPSS, Chicago, IL, USA), including publication data (author, year of publication, study type), type of intervention, characteristics of participants (number of patients, mean age, male-to-female ratio), perioperative details, and other outcomes (operating time, hospital stay, mean healing time, complications, recurrence, and/or success rates, continence impairment, pre- and postoperative anorectal manometry, QoL scores).
Data extraction was performed by two reviewers (AP, LF) and independently assessed by another (FL) for completeness and accuracy. Surgical procedures were summarized as sphincter-cutting procedures (fistulotomy, fistulectomy, and cutting setons) or sphincter-sparing techniques [glues/pastes, laser, flap, ligation of intersphinctericv fistula tract (LIFT), etc.].
Risk of bias assessment
A risk of bias and quality assessment was performed for each article. For randomized studies, the Jadad scale was used (1–5 points, 1 = poor and 5 = excellent) [11], while for non-randomized studies, the Methodological Index for Non-Randomized Studies (MINORS) Scale for comparative (0–24 points, 0 = poor and 24 = excellent) or non-comparative (0–16 points, 0 = poor and 16 = excellent) studies was applied [12].
Data reporting and statistical analysis
Descriptive statistics have been reported as absolute frequencies and percentages for qualitative data; quantitative variables have been described as mean value (standard deviation) or median (range), based on availability. For means, the weighted averages were calculated as follows: (single study average × study cohort size) 1, 2, …, n/pooled cohort size. This was done to minimize the effect of the different cohort sizes of the studies on the calculated averages and to provide an overall value for the outcome measures evaluated.
Results
Study selection and risk of bias
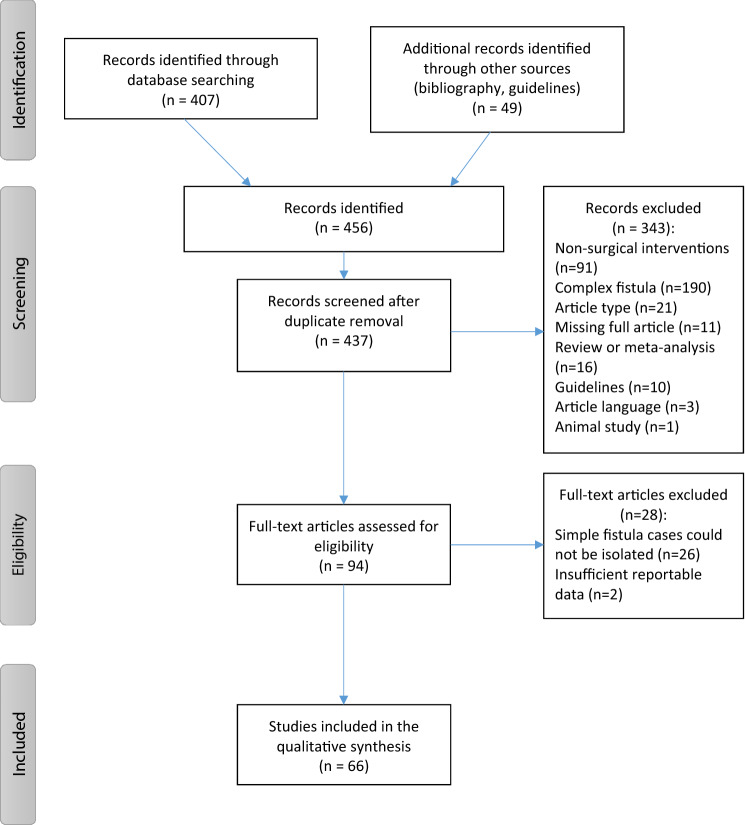
The search returned 456 records of interest. After removal of duplicated records, 437 were screened; after title and abstract evaluation, 343 were excluded according to the inclusion criteria. Finally, 94 full text articles were assessed for eligibility; however, 28 of them were excluded, mainly because of the impossibility of isolating data on patients affected by simple AFs from mixed case reports. Therefore, a total of 66 articles [2, 8, 13–76] were found to be eligible (Fig. 1). The publication dates of the articles range from 1994 to 2020. Among the included studies, 28 were prospective studies [21–25, 29, 38–40, 42, 44, 48, 51, 53, 56, 58–62, 64, 65, 68, 70, 71, 74–76], 19 were retrospective series [2, 8, 13–15, 18, 26–28, 33, 43, 45, 57, 63, 66, 67, 69, 72, 73], and 19 were randomized clinical trials (RCT) [16, 17, 19, 20, 30–32, 34–37, 41, 46, 47, 49, 50, 52, 54, 55] (Tables 1–2). The quality of the studies was generally low with a consistent risk of bias; the median score of the Jadad Scale for RCT was 3 (1–5), and only 2 studies had the highest possible score [52, 55]; the median MINORS score for non-comparative studies was 12 (3–16), with only one study that could be regarded as excellent [44], while the median MINORS score for comparative studies was 17 (8–21) (Tables 1, 2). Risk of bias of the selected studies could be attributed mainly to a retrospective design, difficulty or impossibility of patients’ and operators’ blinding, small sample size, short follow-up, heterogeneity of the analyzed variables, absence of uniform definition of the main outcomes (success rate, continence impairment).
Fig. 1.
PRISMA flow diagram of the included studies
Table 1.
Patient and study characteristics—sphincter-cutting procedures
| Authors | Year | Study type | Intervention | Patients | Age (years) | Sex (M:F) |
Quality of the studya |
|---|---|---|---|---|---|---|---|
| Sangwan et al. [13] | 1994 | R | Fistulotomy | 461 | 42 | 310:151 | 8/16 |
| Lentner and Wienert [14] | 1996 | R | Long-term indwelling seton | 108 | NR | NR | 6/16 |
| Hongo et al. [15] | 1997 | R | Coring out | 319 | NR | NR | 4/16 |
| Ho et al. [16] | 1998 | RCT | Fistulotomy | 52 | 41.1 | 49:3 | 3/5 |
| Fistulotomy with marsupialization | 51 | 41.2 | 41:10 | ||||
| Ho et al. [17] | 2001 | RCT | Chemical ayurvedic seton | 46 | 42 | 21:2 | 3/5 |
| Fistulotomy | 54 | 37 | 5:1 | ||||
| Isbister and Al Sanea [18] | 2001 | R | Cutting Seton | 31 | 42 | 14.5:1 | 12/16 |
| Shahbaz et al. [19] | 2002 | RCT | Fistulectomy | 25 | 32.1 | 24:1 | 1/5 |
| Fistulectomy with primary closure | 25 | ||||||
| Lindsey et al. [20] | 2002 | RCT | Fistulotomy | 7 | NA | NA | 3/5 |
| Chang and Lin [21] | 2003 | P | Fistulotomy | 45 | 54.2 | 29:16 | 14/16 |
| Gupta [22] | 2004 | P | Radiofrequency fistulotomy | 232 | NR | NR | 11/16 |
| Hammond et al. [23] | 2006 | P | Snug seton | 18 | 42* | 26:3 | 13/16 |
| Van Der Hagen et al. [24] | 2006 | P | Fistulotomy | 62 | 40* | 22:9 | 11/16 |
| Mahajan et al. [25] | 2007 | P | Fistulectomy and skin graft | 25 | NR | 24:1 | 3/16 |
| Van Koperen et al. [26] | 2008 | R | Fistulotomy | 109 | 39 | 71:38 | 14/16 |
| Jordàn et al. [27] | 2009 | R | Fistulotomy, fistulectomy | 76 | NA | NA | 12/16 |
| Bokhari and Lindsey [28] | 2010 | R | Fistulotomy | 57 | NA | NA | 17/24 |
| Bhatti et al. [29] | 2011 | P | Fistulotomy | 25 | NR | 46:4 | 15/24 |
| Fistulectomy | 25 | NR | |||||
| Sahakitrungruang et al. [30] | 2011 | RCT | Fistulotomy | 25 | 43.2 | 23:2 | 3/5 |
| Fistulotomy with marsupialization | 25 | 40.6 | 4:1 | ||||
| Nazeer et al. [31] | 2012 | RCT | Fistulectomy | 75 | NR | NR | 3/5 |
| Fistulotomy | 75 | NR | NR | ||||
| Jain et al. [32] | 2012 | RCT | Fistulectomy | 20 | 34.5 | 4:1 | 3/5 |
| Fistulotomy with marsupialization | 20 | 34.3 | 9:1 | ||||
| Salem [33] | 2012 | R | Fistulectomy | 146 | NR | 190:82 | 14/24 |
| Fistulotomy | 126 | NR | |||||
| Kamal [34] | 2012 | RCT | Fistulotomy | 32 | NR | 15:4 | 1/5 |
| Fistulectomy | 44 | NR | |||||
| Wang et al. [35] | 2012 | RCT | SDPC suture dragging and pad compression | 6 | NA | NA | 3/5 |
| Fistulotomy | 5 | NA | NA | ||||
| Chalya and Mabula [36] | 2013 | RCT | Fistulectomy | 82 | 37.8 | 76:6 | 3/5 |
| Fistulotomy with marsupialization | 80 | 38.6 | 74:6 | ||||
| Gottgens et al. [8] | 2015 | R | Fistulotomy | 537 | 45.5 | 379:158 | 12/16 |
| Sheikh et al. [37] | 2015 | RCT | Fistulotomy | 131 | 32.5 | All M | 1/5 |
| Fistulectomy | 131 | 33.5 | All M | ||||
| Visscher et al. [2] | 2015 | R | Fistulotomy | 68 | NA | NA | 13/16 |
| Abramowitz et al. [38] | 2016 | P | Fistulotomy | 133 | 48 | 107:133 | 14/16 |
| Elsebai et al. [39] | 2016 | P | Fistulectomy | 15 | 35.3 | 23:7 | 21/24 |
| Fistulotomy | 15 | 37.4 | |||||
| Limongelli et al. [40] | 2016 | P | Fistulotomy | 29 | 41 | 40:13 | 20/24 |
| Fistulotomy with marsupialization | 44 | ||||||
| Saber [41] | 2016 | RCT | Fistulotomy | 100 | NR | All M | 3/5 |
| Fistulectomy | 100 | NR | All M | ||||
| Vyas et al. [42] | 2016 | P | Fistulotomy | 38 | 45.2 | 7.3:1 | 17/24 |
| Fistulectomy | 37 | ||||||
| Wang and Rosen [43] | 2016 | R | Fistulotomy | 26 | 46.4 | 23:3 | 13/16 |
| Jayarajah et al. [44] | 2017 | P | Multiple techniques | 34 | 42.5 | 30:14 | 16/16 |
| Murtaza et al. [45] | 2017 | R | Fistulotomy | 96 | 40.5 | 81:15 | 21/24 |
| Fistulectomy | 96 | 41.4 | 92:4 | ||||
| Ganesan et al. [46] | 2017 | RCT | Fistulotomy | 30 | NR | NR | 3/5 |
| Fistulectomy | 30 | NR | NR | ||||
| Shahid et al. [47] | 2017 | RCT | Fistulectomy | 30 | 35.8 | 4:1 | 3/5 |
| Fistulectomy and suture | 30 | 38.4 | 13:1 | ||||
| Vyas et al. [48] | 2017 | P | Fistulotomy | 92 | 38.5 | 85:7 | 8/16 |
| Mittal et al. [49] | 2018 | RCT | Fistulotomy | 38 | 41.5 | 31:6 | 3/5 |
| Fistulectomy | 37 | 45.2 | 35:3 | ||||
| Gupta et al. [50] | 2018 | RCT | Fistulectomy | 30 | 35.5 | 28:2 | 1/5 |
| Mallik et al [51] | 2018 | P | Fistulotomy | 25 | 39.6 | 23:2 | 13/24 |
| Fistulectomy | 25 | 24:1 | |||||
| Anan et al. [52] | 2019 | RCT | Fistulotomy | 30 | 38.3 | 4:1 | 5/5 |
| Fistulotomy with marsupialization | 30 | 43.5 | 13:2 | ||||
| Bhatia [53] | 2019 | P | Fistulectomy | 50 | NR | > 2:1 | 12/16 |
| Sahai et al. [54] | 2019 | RCT | Fistulotomy | 28 | 41 | 5:1 | 1/5 |
| Sanad et al. [55] | 2019 | RCT | Fistulotomy + phenytoin 2% and sitz baths | 30 | 41.4 | 5:1 | 5/5 |
| Fistulotomy + sitz baths | 30 | ||||||
| Basa and Prakash [56] | 2020 | P | Open Fistulectomy | 25 | NR | 2:1 | 21/24 |
| Fistulectomy with primary closure | 25 | NR | |||||
| De Hous et al. [57] | 2020 | R | Fistulectomy and suture | 24 | 52.8 | 2:1 | 14/16 |
| Total | 4883 |
P prospective study, R retrospective study, RCT randomized clinical trial, NR not reported, NA not available
*Values are median
aRandomized studies assessed according to JADAD scale [11] (maximum score: 5); non-randomized studies assessed according to MINOR Scale [12] (maximum score 16 for non-comparative studies. 24 for comparative studies)
Table 2.
Patient and study characteristics—sphincter-sparing techniques
| Authors | Year | Study type | Intervention | Patients (no.) | Age (years) | Sex (M:F) | Quality of the studya |
|---|---|---|---|---|---|---|---|
| Cintron et al [58] | 2000 | P | Fibrin glue | 11 | NA | NA | 19/24 |
| Lindsey et al [20] | 2002 | RCT | Fibrin glue | 6 | NA | NA | 3/5 |
| Mohammed [59] | 2004 | P | Laser | 6 | 32 | All M | 11/16 |
| Gisbertz et al [60] | 2005 | P | Fibrin glue | 27 | 43 | 23:4 | 13/16 |
| Barillari et al [61] | 2006 | P | Cyanoacrylate glue | 7 | NA | NA | 13/16 |
| Rojanasakul et al [62] | 2007 | P | LIFT | 13 | NA | NA | 12/16 |
| Chew and Adams [63] | 2007 | R | Advancement flap | 6 | 46 | 2:1 | 11/16 |
| Jain et al [64] | 2008 | P | Cyanoacrylate glue | 20 | 26 | 3:1 | 12/16 |
| Bokhari and Lindsey [28] | 2010 | R | Flap and glue | 9 | NA | NA | 17/24 |
| Mishra et al [65] | 2013 | P | Fibrin glue | 16 | NA | NA | 11/16 |
| Van Onkelen et al [66] | 2013 | R | LIFT | 22 | 45.5 | 13:9 | 14/16 |
| Oztürk and Gülcü [67] | 2014 | R | Laser | 44 | NR | NR | 13/16 |
| Cestaro et al [68] | 2014 | P | Fibrin glue | 6 | NR | NR | 12/16 |
| Malakorn et al [69] | 2017 | R | LIFT | 167 | NR | NR | 13/16 |
| Wilhelm et al [70] | 2017 | P | Laser | 8 | NA | NA | 13/16 |
| Gupta et al [50] | 2018 | RCT | SLOFT | 30 | 33.5 | 23:7 | 1/5 |
| Giordano et al [71] | 2018 | P | Permacol paste | 27 | NA | NA | 12/16 |
| Terzi et al [72] | 2018 | R | Laser | 61 | NA | NA | 15/16 |
| Marinello et al [73] | 2018 | R | OTSC clip | 3 | 58.3 | All F | 9/16 |
| Bayrak et al [74] | 2018 | P | Permacol paste | 11 | NA | NA | 11/16 |
| Sahai et al [54] | 2019 | RCT | LIFT | 22 | 41 | 5:1 | 1/5 |
| Iqbal et al [75] | 2019 | P | 1% silver nitrate | 76 | 32 | 31:7 | 11/16 |
| Vander Mijnsbrugge et al [76] | 2019 | P | LIFT | 4 | NA | NA | 15/16 |
| Total | 602 |
P prospective study, R retrospective study, RCT randomized clinical trial, NR not reported, NA not available, LIFT ligation of the intersphincteric fistula tract, SLOFT submucosal llgation of fistula tract
*Values are median
aRandomized studies assessed according to JADAD scale [11]; non-randomized studies assessed according to MINOR scale [12] (maximum score 16 for non-comparative studies. 24 for comparative studies)
Patient characteristics and surgical procedures
A total of 4883 patients (weighted average age: 41.3 years; M:F ratio 6:1) underwent a sphincter-cutting procedure, which was usually fistulotomy or fistulectomy (Table 1). Main technical variations reported were marsupialization [16, 30, 32, 36, 40, 52] or primary sphincteroplasty [19, 35, 47, 56, 57].
Sphincter-sparing techniques were adopted to treat 602 patients (weighted average age: 36.2 years; M:F ratio 4:1) with a simple AF (Table 2). Among those, glues/pastes (fibrin glue, Permacol® collagen paste, and cyanoacrylate glue) were the most frequently analyzed procedures with ten records [20, 28, 58, 60, 61, 64, 65, 68, 71, 74]. LIFT and the laser closure of fistula tracts were reported in five [54, 62, 66, 69, 76] and four studies [59, 67, 70, 72], respectively. Other procedures adopted are detailed in Table 2.
Perioperative details
When reported, the weighted average duration of the sphincter-cutting procedures was 21.9 (8.0–43.0) minutes, and the weighted average duration of hospital stay was 3.1 (0–13.0) days. The weighted average healing time was 41.0 (8.0–183.0) days (Table 3). The most frequent complication reported was wound infection (123 cases, 6%), followed by bleeding (53 cases, 2.9%) and urinary retention (40 cases, 2.6%) (Table 3).
Table 3.
Perioperative details—sphincter-cutting procedures
| Authors | Technique | Operation time (minutes) | Hospital stay (days) | Healing time (days) | Morbidity (no. %) | |||
|---|---|---|---|---|---|---|---|---|
| Bleeding | Urinary retention | Infection | Other | |||||
| Lentner and Wienert | Long term indwelling seton | NR | 0.3 | NR | NR | NR | NR | NR |
| Ho et al | Fistulotomy | 8.0 | 2.0 | 42.0 | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Ho et al | Fistulotomy with marsupialization | 10.0 | 1.0 | 70.0 | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Ho et al | Chemical ayurvedic seton | NR | 1* | 54* | 0 (0) | 0 (0) | 1 (2.2) | 0 (0) |
| Ho et al | Fistulotomy | NR | 1* | 45* | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Isbister and Al Sanea | Cutting Seton | NR | NR | 183.0 | NR | NR | NR | 0 (0) |
| Shahbaz et al | Fistulectomy | NR | NR | 31.8 | NR | NR | NR | 0 (0) |
| Shahbaz et al | Fistulectomy with primary closure | NR | NR | 8.0 | NR | NR | NR | 0 (0) |
| Lindsey et al | Fistulotomy | NA | NA | NA | NA | NA | NA | 0 (0) |
| Gupta | Radiofrequency fistulotomy | 13.0 | 0 | 67.0 | 0 (0) | 0 (0) | 0 (0) | 1 (0.4) |
| Hammond et al | Snug seton | NA | NA | NA | NR | NR | 1 (5.6) | 2 (11.1) |
| Mahajan et al | Fistulectomy and skin graft | 41.2 | 9.2 | 13.8 | NR | NR | NR | NR |
| Van Koperen et al | Fistulotomy | NR | NR | NR | 1 (0.9) | 0 (0) | 1 (0.9) | 0 (0) |
| Bhatti et al | Fistulotomy | NR | 1.5 | 24* | 1 (4) | 0 (0) | 0 (0) | 0 (0) |
| Bhatti et al | Fistulectomy | NR | 2.5 | 35* | 3 (12) | 0 (0) | 0 (0) | 0 (0) |
| Sahakitrungruang et al | Fistulotomy | NR | NR | NR | 2 (8) | 2 (8) | 1 (4) | 0 (0) |
| Sahakitrungruang et al | Fistulotomy with marsupialization | NR | NR | NR | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Nazeer et al | Fistulectomy | NR | 3.5 | 40.0 | 5 (6.7) | 0 (0) | 0 (0) | 0 (0) |
| Nazeer et al | Fistulotomy | NR | 2.0 | 28.0 | 1 (1.3) | 0 (0) | 0 (0) | 0 (0) |
| Jain et al | Fistulectomy | 28.0 | NR | 47.3 | NR | NR | NR | NR |
| Jain et al | Fistulotomy with marsupialization | 28.2 | NR | 34.0 | NR | NR | NR | NR |
| Salem | Fistulectomy | NR | 2.0 | 21.0 | NR | NR | NR | NR |
| Salem | Fistulotomy | NR | 3.0 | 28.0 | NR | NR | NR | NR |
| Kamal | Fistulotomy | 17.3 | NR | 26.4 | 0 (0) | 0 (0) | 1 (3.1) | 0 (0) |
| Kamal | Fistulectomy | 33.0 | NR | 38.6 | 1 (2.3) | 0 (0) | 1 (2.3) | 0 (0) |
| Chalya e Mabula | Fistulectomy | 28.4 | 3.9 | 36.4 | 0 (0) | 0 (0) | 27 (32.9) | 0 (0) |
| Chalya e Mabula | Fistulotomy with marsupialization | 29.2 | 4.2 | 28.6 | 0 (0) | 0 (0) | 28 (35) | 0 (0) |
| Gottgens et al | Fistulotomy | NR | NR | 37* | NR | NR | NR | NR |
| Sheikh et al | Fistulotomy | 14.3 | 3.7 | 28.8 | 1 (0.8) | NR | 3 (2.3) | NR |
| Skeikh et al | Fistulectomy | 25.9 | 4.9 | 32.0 | 4 (3.1) | NR | 5 (3.8) | NR |
| Abramowitz et al | Fistulotomy | NR | NR | 56* | 1 (0.8) | 0 (0) | 0 (0) | 0 (0) |
| Elsebai et al | Fistulectomy | 40.7 | NR | 45.3 | 0 (0) | 2 (13.3) | 1 (6.7) | NR |
| Elsebai et al | Fistulotomy | 19.4 | NR | 28.5 | 0 (0) | 1 (6.7) | 2 (13.3) | NR |
| Limongelli et al | Fistulotomy | NR | NR | NR | 14 (48.3) | NR | NR | NR |
| Limongelli et al | Fistulotomy with marsupialization | NR | NR | NR | 7 (15.9) | NR | NR | NR |
| Saber | Fistulotomy | 27.0 | 1.0 | 30.0 | NR | NR | NR | NR |
| Saber | Fistulectomy | 37.0 | 1.0 | 41.7 | NR | NR | NR | NR |
| Vyas et al | Fistulotomy | NR | 2.9 | 28.6 | NR | NR | 4 (10.5) | NR |
| Vyas et al | Fistulectomy | NR | 4.3 | 48.5 | NR | NR | 15 (40.5) | NR |
| Murtaza et al | Fistulotomy | 17* | NR | 15* | NR | NR | NR | NR |
| Murtaza et al | Fistulectomy | 25* | NR | 30* | NR | NR | NR | NR |
| Ganesan et al | Fistulotomy | 12.1 | 1.8 | 24.2 | 0 (0) | 3 (10.0) | 1 (3.3) | NR |
| Ganesan et al | Fistulectomy | 22.2 | 2.6 | 31.5 | 2 (6.7) | 5 (16.7) | 3 (10) | NR |
| Vyas et al | Fistulotomy | NR | NR | 28.0 | NR | NR | 7 (7.7) | NR |
| Mittal et al | Fistulotomy | NR | 2.9 | 28.6 | NR | NR | 4 (10.5) | NR |
| Mittal et al | Fistulectomy | NR | 4.3 | 48.5 | NR | NR | 15 (40.5) | NR |
| Gupta et al | Fistulectomy | 43.0 | NR | 32.0 | NR | NR | 2 (6.7) | NR |
| Mallik et al | Fistulotomy | 9.7 | 3.9 | 16.8 | NR | 0 (0) | NR | NR |
| Mallik et al | Fistulectomy | 15.2 | 4.2 | 24.4 | NR | 0 (0) | NR | NR |
| Anan et al | Fistulotomy | 16.8 | NR | 46.9 | 2 (6.7) | 1 (3.3) | 0 (0) | 0 (0) |
| Anan et al | Fistulotomy with marsupialization | 18.4 | NR | 35.7 | 0 (0) | 2 (6.7) | 0 (0) | 0 (0) |
| Bhatia | Fistulectomy | 26.4 | 2.0 | 39.0 | 3 (6) | 6 (12) | 0 (0) | 6 (12) |
| Sanad et al | Fistulotomy + phenytoin 2% and sitz baths | 13.0 | 0 | 41.2 | 3 (10) | 1 (3.3) | 0 (0) | 0 (0) |
| Sanad et al | Fistulotomy + sitz baths | 14.0 | 0 | 42.0 | 2 (6.7) | 1 (3.3) | 0 (0) | 0 (0) |
| Basa and Prakash | Fistulectomy | NR | 1.0 | 31.0 | 0 (0) | 10 (40) | 0 (0) | 0 (0) |
| Basa and Prakash | Fistulectomy with primary closure | NR | 7.0 | 8.0 | 0 (0) | 6 (24) | 0 (0) | 0 (0) |
| De Hous et al | Fistulectomy and suture | 20* | 0 | NR | 0 (0) | NR | 0 (0) | 6 (25) |
| Total | 53 (2.9) | 40 (2.6) | 123 (6) | 15 (4) | ||||
| Weighted average | 21.9 | 3.1 | 41.0 | |||||
NR not reported, NA not available
*Values are median
The overall weighted average operation time of sphincter-sparing procedures was 34.5 (19.0–52.5) minutes, with a weighted average postoperative hospital stay of 0.8 (0–1.5) days. Only 3 studies reported healing time [50, 59, 62]; the weighted average was 15.1 (7.7–28.0) days (Table 4). The morbidity rate was very low, with a total of 6 complications registered (Table 4).
Table 4.
Perioperative details—sphincter-sparing techniques
| Authors | Technique | Operation time (minutes) | Hospital stay (days) | Healing time (days) | Morbidity (no. %) | |||
|---|---|---|---|---|---|---|---|---|
| Bleeding | Urinary retention | Infection | Other | |||||
| Lindsey et al | Fibrin glue | NA | NA | NA | NA | NA | NA | 1 (16.7) |
| Mohammed | Laser | 19.0 | 0 | 7.7 | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Gisbertz et al | Fibrin glue | 20.0 | NR | NA | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Barillari et al | Cyanoacrylate glue | NR | NR | NR | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Rojanasakul et al | LIFT | 40 | 1.3 | 28.0 | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Chew e Adams | Advancement flap | 52.5 | 1.0 | NR | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Jain et al | Cyanoacrylate glue | NR | 0.0 | NR | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Mishra et al | Fibrin glue | NA | NA | NA | 0 (0) | 0 (0) | 0 (0) | 1 (6.3) |
| Oztürk and Gulcü | Laser | NR | 1.5 | NR | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Cestaro et al | Fibrin glue | NR | 1.0 | NR | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Gupta et al | SLOFT | 46.0 | NR | 11.0 | 0 (0) | 0 (0) | 1 (3.3) | 0 (0) |
| Marinello et al | OTSC clip | 21.7 | NR | NR | 0 (0) | 0 (0) | 0 (0) | 3 (100) |
| Iqbal et al | 1% silver nitrate | NR | NR | NR | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Vander Mijnsbrugge et al | LIFT | NA | NA | NA | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| Total | 0 (0) | 0 (0) | 1 (0.004) | 5 (0.02) | ||||
| Weighted average | 34.5 | 0.8 | 15.1 | |||||
NR not reported, NA not available, LIFT ligation of the intersphincteric fistula tract, SLOFT submucosal ligation of fistula tract
* Values are median
Success rate and continence status
After a weighted average follow-up of 14.7 (1–77) months, the weighted mean success rate after a sphincter-cutting procedure was 93.7% (61.0–100%), while any postoperative continence impairment was reported in 12.7% of patients (0–45.7%) (Table 5).
Table 5.
Results—sphincter-cutting procedures
| Author | Technique | Follow-up (months) | Success (%) | Preoperative continence impairment (%) | Postoperative continence impairment (%) | |||
|---|---|---|---|---|---|---|---|---|
| Any impairment | Incontinence to liquid | Incontincence to gas | Major incontinence | |||||
| Sangwan et al | Fistulotomy | 34.0 | 93.5 | NR | NA | 2.8 | NR | 0.0 |
| Lentner and Wienert | Long term Indwelling seton | 15.6 | 88.0 | 0 | 1 | 0 | 1 | 0.0 |
| Hongo et al | Coring out | NR | 98.7 | NR | 6.4 | NR | NR | NR |
| Ho et al | Fistulotomy | 9.0 | 96.0 | NR | 12.0 | NR | NR | NR |
| Ho et al | Fistulotomy with marsupialization | 10.2 | 98.0 | NR | 2.0 | NR | NR | NR |
| Ho et al | Chemical ayurvedic seton | 2.3* | 97.8 | NR | 10.9 | 6.5 | 4.3 | 0.0 |
| Ho et al | Fistulotomy | 1.9* | 98.2 | NR | 5.6 | 3.7 | 1.9 | 0.0 |
| Isbister and Al Sanea | Cutting seton | 13 | 96.8 | NA | 7.1 | 0 | 7.1 | 0 |
| Shahbaz et al | Fistulectomy | NR | 88.0 | NR | 12.0 | NR | 12.0 | NR |
| Shahbaz et al | Fistulectomy with primary closure | NR | 92.0 | NR | NR | NR | NR | NR |
| Lindsey et al | Fistulotomy | 18 | 100.0 | NA | 0 | 0 | 0 | 0 |
| Chang and Lin | Fistulotomy | 9.5 | 100.0 | NR | 38 | NR | NR | NR |
| Gupta | Radiofrequency fistulotomy | 15.0 | 99.2 | NR | 0 | 0 | 0 | 0 |
| Hammond et al | Snug seton | NA | 100.0 | 0 | 25.0 | 0 | 25.0 | 0 |
| Van Der Hagen et al | Fistulotomy | 75* | 61.0 | 4.8 | 9.7 | 0 | 0 | 0 |
| Van Koperen et al | Fistulotomy | 77* | 93.0 | 2.8 | 41.0 | NR | NR | 4.8 |
| Jordàn et al | Fistulotomy, fistulectomy | 19.2 | 97.4 | NA | 8.1 | NA | NA | NA |
| Bokhari and Lindsey | Fistulotomy | NR | 93.0 | NR | 16.0 | NR | 11.0 | 5.0 |
| Bhatti et al | Fistulotomy | NR | 100.0 | NR | 0 | 0 | 0 | 0 |
| Bhatti et al | Fistulectomy | NR | 100.0 | NR | 0 | 0 | 0 | 0 |
| Sahakitrungruang et al | Fistulotomy | NR | 100.0 | NR | 0 | 0 | 0 | 0 |
| Sahakitrungruang et al | Fistulotomy with marsupialization | NR | 100.0 | NR | 0 | 0 | 0 | 0 |
| Nazeer et al | Fistulectomy | 10.0 | 100.0 | NR | 0 | 0 | 0 | 0 |
| Nazeer et al | Fistulotomy | 10.0 | 100.0 | NR | 0 | 0 | 0 | 0 |
| Jain et al | Fistulectomy | 3.0 | 100.0 | NR | 0 | 0 | 0 | 0 |
| Jain et al | Fistulotomy with marsupialization | 3.0 | 100.0 | NR | 0 | 0 | 0 | 0 |
| Salem | Fistulectomy | 12 | 94.0 | NR | NR | NR | NR | NR |
| Salem | Fistulotomy | 12 | 90.0 | NR | NR | NR | NR | NR |
| Kamal | Fistulotomy | 12.0 | 93.7 | NR | 6.3 | 0 | 6.3 | 0 |
| Kamal | Fistulectomy | 12.0 | 93.2 | NR | 11.4 | 0 | 11.4 | 0 |
| Wang et al | SDPC suture dragging and pad compression | 12 | 96.7 | 0 | 0.0 | NA | NA | NA |
| Wang et al | Fistulotomy | 12 | 100.0 | 0 | 1.0 | NR | NR | NR |
| Chalya and Mabula | Fistulectomy | 3.0 | 100.0 | NR | 0 | 0 | 0 | 0 |
| Chalya and Mabula | Fistulotomy with marsupialization | 3.0 | 100.0 | NR | 0 | 0 | 0 | 0 |
| Gottgens et al | Fistulotomy | 38.9* | 83.6 | 1.3 | 45.7 | NA | NA | 28.0 |
| Sheikh et al | Fistulotomy | 6 | 89.3 | NR | NR | NR | NR | NR |
| Skeikh et al | Fistulectomy | 6 | 84.7 | NR | NR | NR | NR | NR |
| Visscher et al | Fistulotomy | NA | 84.0 | NR | 27.9 | 3.0 | 24.0 | 3.0 |
| Abramowitz et al | Fistulotomy | 12.0 | 99.2 | NR | NA | NA | NA | NA |
| Elsebai et al | Fistulectomy | 8.0 | 100.0 | 0.0 | 6.7 | 0.0 | 6.7 | 0.0 |
| Elsebai et al | Fistulotomy | 8.0 | 100.0 | 0.0 | 13.3 | 0.0 | 13.3 | 0.0 |
| Limongelli et al | Fistulotomy | 39.4 | 96.6 | NR | NR | NR | NR | NR |
| Limongelli et al | Fistulotomy with marsupialization | 39.4 | 95.5 | NR | NR | NR | NR | NR |
| Saber | Fistulotomy | NR | 98.0 | NR | 2.0 | NA | NA | NA |
| Saber | Fistulectomy | NR | 100.0 | NR | 4.0 | NA | NA | NA |
| Vyas et al | Fistulotomy | NR | 94.7 | NR | 0 | NA | NA | NA |
| Vyas et al | Fistulectomy | NR | 81.1 | NR | 0 | NA | NA | NA |
| Wang e Rosen | Fistulotomy | 11.9 | 100.0 | NR | NR | 0 | NA | 0 |
| Jayarajah et al | Multiple techniques | 27.5 | NR | 18.0 | 38.0 | NR | NR | NR |
| Murtaza et al | Fistulotomy | 6.0 | 96.9 | NR | 5.3 | NR | NR | NR |
| Murtaza et al | Fistulectomy | 6.0 | 95.8 | NR | 12.5 | NR | NR | NR |
| Ganesan et al | Fistulotomy | 8.0 | 96.7 | NR | 1.0 | 0.0 | 6.7 | 0.0 |
| Ganesan et al | Fistulectomy | 8.0 | 100.0 | NR | 0.0 | 3.3 | 13.3 | 0.0 |
| Shahid et al | Fistulectomy | 1.5 | 93.3 | NR | NR | NR | NR | NR |
| Shahid et al | Fistulectomy and suture | 1.5 | 100.0 | NR | NR | NR | NR | NR |
| Vyas et al | Fistulotomy | NR | 96.8 | NR | 0.0 | NR | NR | NR |
| Mittal et al | Fistulotomy | NR | 94.7 | NR | 0 | 0 | 0 | 0 |
| Mittal et al | Fistulectomy | NR | 81.1 | NR | 0 | 0 | 0 | 0 |
| Gupta et al | Fistulectomy | NR | 100.0 | NR | 3.3 | NR | NR | NR |
| Mallik et al | Fistulotomy | 18.0 | 96.0 | NR | 0 | 0 | 0 | 0 |
| Mallik et al | Fistulectomy | 18.0 | 100.0 | NR | 0 | 0 | 0 | 0 |
| Anan et al | Fistulotomy | 11.3 | 96.7 | NR | 3.3 | 0 | 3.3 | 0 |
| Anan et al | Fistulotomy with marsupialization | 11.5 | 100.0 | NR | 0 | 0 | 0 | 0 |
| Bhatia | Fistulectomy | NR | 96.0 | NR | 8.0 | 0 | 8.0 | 0 |
| Sahai et al | Fistulotomy | 2–6 | 86.0 | NR | 0 | NA | NA | NA |
| Sanad et al | Fistulotomy + phenytoin 2% and sitz baths | 8.2 | 100.0 | NR | 0 | NA | NA | NA |
| Sanad et al | Fistulotomy + Sitz baths | 7.6 | 100.0 | NR | 0 | NA | NA | NA |
| Basa and Prakash | Open Fistulectomy | 1 | 96.0 | NR | 0 | NA | NA | NA |
| Basa and Prakash | Fistulectomy with primary closure | 1 | 100.0 | NR | 0 | NA | NA | NA |
| De Hous et al | Fistulectomy and suture | 3* | 95.8 | NR | 20.8 | NR | NR | NR |
| Weighted average | 14.7 | 93.7 | 2.1 | 12.7 | 1.1 | 3.7 | 6.0 | |
NR not reported, NA not available
* Values are median
Overall, sphincter-sparing techniques reached a weighted average success rate of 77.7% (25.0–100%) after a weighted average follow-up of 13.2 (2.3–71.0) months. No study reported any postoperative continence deterioration, with the exception of a retrospective study reporting minor incontinence in 1 out of 9 patients (11.1%) with a simple AF and treated with a sphincter-saving technique [28] (Table 6).
Table 6.
Results—sphincter-sparing procedures
| Author | Technique | Follow-up (months) | Success (%) | Preoperative continence impairment (%) | Postoperative continence impairment (%) | |||
|---|---|---|---|---|---|---|---|---|
| Any impairment | Incontinence to liquid | Incontincence to gas | Major incontinence | |||||
| Cintron et al | Fibrin glue | NA | 82.0 | NR | NR | NR | NR | NR |
| Lindsey et al | Fibrin glue | NA | 50.0 | NA | 0 | 0 | 0 | 0 |
| Mohammed | Laser | 2.3 | 100.0 | NR | 0 | 0 | 0 | 0 |
| Gisbertz et al | Fibrin glue | 6.8* | 33.0 | 7.4 | 0 | 0 | 0 | 0 |
| Barillari et al | Cyanoacrylate glue | 18.0 | 71.4 | 0 | 0 | 0 | 0 | 0 |
| Rojanasakul et al | LIFT | NR | 94.4 | NR | 0 | 0 | 0 | 0 |
| Chew e Adams | Advancement flap | 8.1 | 98.0 | 0 | 0 | 0 | 0 | 0 |
| Jain et al | Cyanoacrylate glue | 6.0 | 95.0 | 0 | 0 | 0 | 0 | 0 |
| Bokhari and Lindsey | Flap and glue | NR | 60.0 | NR | 11.1 | 0 | 11.1 | 0 |
| Mishra et al | Fibrin glue | NA | 81.0 | NA | 0 | 0 | 0 | 0 |
| Oztürk e Gülcü | Laser | NA | 86.4 | NR | NR | NR | NR | NR |
| Cestaro et al | Fibrin glue | 12 | 66.7 | NR | 0 | 0 | 0 | 0 |
| Van Onkelen et al | LIFT | 19.9* | 82.0 | 0 | 0 | 0 | 0 | 0 |
| Malakorn et al | LIFT | 71* | 91.0 | NR | 0 | 0 | 0 | 0 |
| Wilhelm et al | Laser | NA | 100.0 | NA | 0 | 0 | 0 | 0 |
| Gupta et al | SLOFT | NR | 100.0 | NR | 0 | 0 | 0 | 0 |
| Giordano et al | Permacol paste | 12 | 70.4 | NA | NA | NA | NA | NA |
| Terzi et al | Laser | 28.3 | 39.0 | NR | 0 | 0 | 0 | 0 |
| Marinello et al | OTSC clip | 22.7 | 100.0 | NR | NR | NR | NR | NR |
| Bayrak et al | Permacol paste | 12 | NA | NA | 0 | 0 | 0 | 0 |
| Sahai et al | LIFT | 2–6 | 68.2 | NR | 0 | 0 | 0 | 0 |
| Iqbal et al | 1% silver nitrate | 2.5 | 76.3 | NR | NR | NR | NR | NR |
| Vander Mijnsbrugge et al | LIFT | 45 | 25.0 | NA | 0 | 0 | 0 | 0 |
| Weighted average | 13.2 | 77.7 | 2.4 | 0.2 | 0 | 0.2 | 0 | |
NR not reported, NA not available, LIFT ligation of the intersphincteric fistula tract, SLOFT submucosal ligation of fistula tract
* Values are median
Only four studies reported anorectal manometry data in patients affected by simple AFs—unfortunately, differences in the instruments and units of measurement adopted (mmHg, cmH2O or kPa) made it impossible to pool the manometric results. In 3 studies, resting and squeeze pressures did not change [17, 20, 35], while a prospective study reported a significant reduction of postoperative resting and squeeze pressures [21].
QoL and patient satisfaction
Seven studies [2, 38, 41, 44, 51, 71, 76] evaluated the effects of surgery on patients’ QoL and satisfaction, even if the data for simple AFs could not be extrapolated for two of them [51, 71]. The postoperative onset of fecal incontinence reduced patients’ QoL in a retrospective series [2], while it had no significant effect in another prospective study [44]; the recurrence of the disease had a negative impact on QoL in a recent prospective study [76]; finally, two reports [38, 41] stated that patient satisfaction after surgery for a simple AF was high or very high in 86.4% and 90.6% of patients, respectively.
Discussion
Surgical treatment of simple AFs is usually considered “simple” by definition. However, over time, the definition of “simple” AFs has led to a reduction in the percentage of the sphincters that is involved, mainly due to the feared risk of postoperative continence impairment [3]. Moreover, it must be considered that the lack of an univocal definition of "simple" fistula can make it difficult to pool the results of the different studies available. However, the selection of studies in this review was performed considering the definition of “simple” fistula provided by the most important international guidelines [4–6]. Only a few of the studies analyzed reported the adoption of imaging techniques (magnetic resonance imaging or endoanal ultrasound) to define the diagnosis, although this probably reflects the infrequent use of these techniques in this kind of anal fistula.
From this systematic review, it emerged that fistulotomy/fistulectomy is by far the most suitable surgical intervention to treat simple AFs. The use of these procedures was constant over the years, and they provide a very high overall success rate (Table 5). However, it should be noted that many of the studies analyzed had a short follow-up, and the healing rate seems to decrease in some studies with a long follow-up. Van der Hagen et al. [24] stated that the recurrence rate after fistulotomy for low AFs gradually increased over time, being 7%, 16%, and 39% after 12, 24, and 72 months of follow-up, respectively. The same study underlined that in more than half of the cases, the recurrence occurred in a different location from the previous fistula tract. Therefore, the authors hypothesized that the recurrence in patients with a simple AF was "more likely a matter of patient disease than a failure of the treatment" [24]. Another large retrospective series on 537 patients showed that the healing rate at the 5-year follow-up was about 83% [8], while a study by van Koperen et al. failed to identify a significant risk factor for fistula recurrence [26].
Concerning the sphincter-sparing procedures, the pooled healing rate calculated in this review was 77.7% (Table 6); however, it should be considered that small sample sizes, short follow-up, and the heterogeneity of the evaluated procedures do not allow us to draw definitive conclusions. LIFT is an attractive recently developed procedure which has proven to be effective (91% success rate) also in a study on simple AFs with a long mean follow-up (71 months) [69]. However, other investigations on this topic are needed to really assess the efficacy of this procedure specifically to treat simple AFs.
Our study confirmed that fistulotomy is a simple and quick procedure (mean operation time: 21 min), with an acceptable mean wound healing time (41 days), although a certain amount of morbidity has been registered (Table 3). In contrast, sphincter-sparing techniques are sometimes more technically demanding and therefore operating time can be longer, even if postoperative complications are almost absent (Table 4). Several new sphincter-sparing techniques have been developed, mainly to reduce the most feared complication of fistulotomy, which is postoperative fecal incontinence. In fact, even this systematic review has confirmed that this complication is almost absent if one of the above-mentioned procedures is used (Table 6). On the other hand, techniques that are not sphincter-sparing could cause continence impairment in approximately 13% of patients with simple AFs (Table 5). Moreover, studies with longer follow-up showed that the incontinence rate after fistulotomy could be higher [2, 8, 21, 44], much more than expected for such a "simple" operation. A study by Visscher et al. [2] reported about 25% of continence impairment (mainly minor) in simple AF patients, with a significant reduction of QoL. Similarly, a high postoperative incontinence rate (about 45%) emerged from a study on 537 patients [8].
There is still debate about how to reduce or contain the risk of fecal incontinence even in simple AFs. Some studies suggest using preoperative anorectal manometry to evaluate baseline anorectal function. Chang and Lin [21] analyzed 45 patients with low intersphincteric fistula with anorectal manometry performed at baseline and at least 6 months after surgery. They found that maximum anal resting pressure significantly decreased, and a lower preoperative anal resting pressure was the only independent predictive factor of postoperative continence disturbances. Similarly, Toyonaga et al. [77] recommend avoiding a fistulotomy in patients with intersphincteric fistulas and with a preoperative low anal squeeze pressure at the anorectal manometry. Therefore, a sphincter-sparing procedure in this kind of patient could be advisable. A technical variation of lay-open fistulotomy to reduce postoperative fecal incontinence seems to be immediate sphincter reconstruction, both for simple and complex fistulas [78].
Some issues regarding the length of hospital stay (3.1 days in the fistulotomy group and 0.8 in the "sphincter-sparing" group) must be considered—the "sphincter-cutting" group includes a relevant number of studies that were carried out decades ago (1990–2000), when protocols on shorter hospital stay were not yet fully implemented. Furthermore, the series with a longer hospital stay were often conducted in specific geographic areas (mainly Asia). We could therefore hypothesize that in both cases, the length of stay was due to hospital requirements. However, we believe that today, in most centers, it is possible to perform both "sphincter-cutting" and "sphincter-sparing" procedures in a day-hospital setting.
Strengths and limitations
This systematic review pooled a large number of patients undergoing surgery for simple AF and analyzed clinically relevant outcomes of different kinds of procedures. As far as we could gather from the literature, an analysis of this size regarding the treatment of simple AFs has never been carried out. The interrogation of multiple search databases allowed us to collect articles from countries with different ranges of income and cultural impact of the disease providing an extensive coverage of both population and procedure types.
The implementation of quality assessment allowed more accurate quantification of selection bias and partially moderated the inhomogeneity of reports.
Nonetheless, a number of limitations of the articles included in this systematic review have surfaced. A large number of studies are low quality and many report a small sample size and/or short follow-up. Additionally, a substantial heterogeneity of the examined procedures, concerning mainly sphincter-sparing techniques was observed. Finally, it must be emphasized that in many of the studies analyzed the continence impairment assessment was performed without the adoption of validated incontinence scores.
Conclusions
Surgical treatment of simple AFs by sphincter-cutting procedures provides excellent cure rates, even if a certain morbidity should be expected. Postoperative continence impairment is not a negligible risk, which could have a detrimental effect on both patients’ QoL and satisfaction. The adoption of sphincter-sparing procedures could be useful in selected patients, and this should be better evaluated in future prospective studies with adequately long follow-up.
Acknowledgements
We thank Dr. Franziska Michaela Lohmeyer for English language editing of this manuscript.
Funding
Open access funding provided by Università Cattolica del Sacro Cuore within the CRUI-CARE Agreement.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest, and no funding from any organization for the submitted work.
Ethical approval
This article does not contain any study with human participants performed by any of the authors.
Informed consent
For this type of study, formal consent is not required.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Francesco Litta, Angelo Parello and Lorenzo Ferri contributed equally to this article.
References
- 1.García-Olmo D, Van Assche G, Tagarro I, et al. Prevalence of anal fistulas in Europe: systematic literature reviews and population-based database analysis. Adv Ther. 2019;36:3503–3518. doi: 10.1007/s12325-019-01117-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Visscher AP, Schuur D, Roos R, Van der Mijnsbrugge GJ, et al. Long-term follow-up after surgery for simple and complex cryptoglandular fistulas: fecal incontinence and impact on quality of life. Dis Colon Rectum. 2015;58:533–539. doi: 10.1097/DCR.0000000000000352. [DOI] [PubMed] [Google Scholar]
- 3.Phillips J, Lees N, Arnall F. Current management of fistula-in-ano. Br J Hosp Med (Lond) 2015;76(142):144–147. doi: 10.12968/hmed.2015.76.3.142. [DOI] [PubMed] [Google Scholar]
- 4.Vogel JD, Johnson EK, Morris AM, et al. Clinical practice guideline for the management of anorectal abscess, fistula-in-ano, and rectovaginal fistula. Dis Colon Rectum. 2016;59:1117–1133. doi: 10.1097/DCR.0000000000000733. [DOI] [PubMed] [Google Scholar]
- 5.Amato A, Bottini C, De Nardi P, et al. Evaluation and management of perianal abscess and anal fistula: SICCR position statement. Tech Coloproctol. 2020;24:127–143. doi: 10.1007/s10151-019-02144-1. [DOI] [PubMed] [Google Scholar]
- 6.Williams G, Williams A, Tozer P, et al. The treatment of anal fistula: second ACPGBI Position Statement—2018. Colorectal Dis. 2018;20:5–31. doi: 10.1111/codi.14054. [DOI] [PubMed] [Google Scholar]
- 7.Mazier WP. Keyhole deformity. Fact and fiction. Dis Colon Rectum. 1985;28:8–10. doi: 10.1007/BF02553897. [DOI] [PubMed] [Google Scholar]
- 8.Göttgens KW, Janssen PT, Heemskerk J, et al. Long-term outcome of low perianal fistulas treated by fistulotomy: a multicenter study. Int J Colorectal Dis. 2015;30:213–219. doi: 10.1007/s00384-014-2072-y. [DOI] [PubMed] [Google Scholar]
- 9.Ratto C, Grossi U, Litta F, et al. Contemporary surgical practice in the management of anal fistula: results from an international survey. Tech Coloproctol. 2019;23:729–741. doi: 10.1007/s10151-019-02051-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Version 2. BMJ 339:b2535. 10.1136/bmj.b2535. [PMC free article] [PubMed]
- 11.Jadad AR, Moore RA, Carroll D, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 12.Slim K, Nini E, Forestier D, et al. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73:712–716. doi: 10.1046/j.1445-2197.2003.02748.x. [DOI] [PubMed] [Google Scholar]
- 13.Sangwan YP, Rosen L, Riether RD, et al. Is simple fistula-in-ano simple? Dis Colon Rectum. 1994;37:885–889. doi: 10.1007/BF02052593. [DOI] [PubMed] [Google Scholar]
- 14.Lentner A, Wienert V. Long-term, indwelling setons for low transsphincteric and intersphincteric anal fistulas. Experience with 108 cases. Dis Colon Rectum. 1996;39:1097–1101. doi: 10.1007/BF02081407. [DOI] [PubMed] [Google Scholar]
- 15.Hongo Y, Kurokawa A, Nishi Y. Open coring-out (function-preserving) technique for low fistulas. Dis Colon Rectum. 1997;40(10 Suppl):S104–106. doi: 10.1007/BF02062031. [DOI] [PubMed] [Google Scholar]
- 16.Ho YH, Tan M, Leong AF, et al. Marsupialization of fistulotomy wounds improves healing: a randomized controlled trial. Br J Surg. 1998;85:105–107. doi: 10.1046/j.1365-2168.1998.00529.x. [DOI] [PubMed] [Google Scholar]
- 17.Ho KS, Tsang C, Seow-Choen F, et al. Prospective randomised trial comparing ayurvedic cutting seton and fistulotomy for low fistula-in-ano. Tech Coloproctol. 2001;5:137–141. doi: 10.1007/s101510100015. [DOI] [PubMed] [Google Scholar]
- 18.Isbister WH, Al SN. The cutting seton: an experience at King Faisal Specialist Hospital. Dis Colon Rectum. 2001;44:722–727. doi: 10.1007/BF02234574. [DOI] [PubMed] [Google Scholar]
- 19.Shahbaz CM, Ghazanfar A, Goraya AR. Comparative study of fistulectomy and fistulectomy with primary repair for low fistula-in-ano. Ann King Edward Med Univ. 2002;8:87–89. [Google Scholar]
- 20.Lindsey I, Smilgin-Humphreys MM, Cunningham C, et al. A randomized, controlled trial of fibrin glue vs. conventional treatment for anal fistula. Dis Colon Rectum. 2002;45:1608–1615. doi: 10.1007/s10350-004-7247-0. [DOI] [PubMed] [Google Scholar]
- 21.Chang SC, Lin JK. Change in anal continence after surgery for intersphincteral anal fistula: a functional and manometric study. Int J Colorectal Dis. 2003;18:111–115. doi: 10.1007/s00384-002-0430-7. [DOI] [PubMed] [Google Scholar]
- 22.Gupta PJ. Radiofrequency fistulotomy: a better alternative for treating low anal fistula. Sao Paulo Med J. 2004;122:172–174. doi: 10.1590/s1516-31802004000400008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hammond TM, Knowles CH, Porrett T, et al. The Snug Seton: short and medium term results of slow fistulotomy for idiopathic anal fistulae. Colorectal Dis. 2006;8:328–337. doi: 10.1111/j.1463-1318.2005.00926.x. [DOI] [PubMed] [Google Scholar]
- 24.van der Hagen SJ, Baeten CG, Soeters PB, et al. Long-term outcome following mucosal advancement flap for high perianal fistulas and fistulotomy for low perianal fistulas: recurrent perianal fistulas: failure of treatment or recurrent patient disease? Int J Colorectal Dis. 2006;21:784–790. doi: 10.1007/s00384-005-0072-7. [DOI] [PubMed] [Google Scholar]
- 25.Mahajan MK, Gupta V, Anand SR. Evalution of fustulectomy and primary skin grafting in low fistula in ano. JK Sci. 2007;9:68–71. [Google Scholar]
- 26.van Koperen PJ, Wind J, Bemelman WA, et al. Long-term functional outcome and risk factors for recurrence after surgical treatment for low and high perianal fistulas of cryptoglandular origin. Dis Colon Rectum. 2008;51:1475–1481. doi: 10.1007/s10350-008-9354-9. [DOI] [PubMed] [Google Scholar]
- 27.Jordán J, Roig JV, García-Armengol J, et al. Risk factors for recurrence and incontinence after anal fistula surgery. Colorectal Dis. 2010;12:254–260. doi: 10.1111/j.1463-1318.2009.01806.x. [DOI] [PubMed] [Google Scholar]
- 28.Bokhari S, Lindsey I (2020) Incontinence following sphincter division for treatment of anal fistula. Colorectal Dis. 12:e135–139. 10.1111/j.1463-1318.2009.01872.x [DOI] [PubMed]
- 29.Bhatti Y, Fatima S, Shaikh GS, et al. Fistulotomy versus fistulectomy in the treatment of low fistula in ano. Rawal Med J. 2011;36:284–286. [Google Scholar]
- 30.Sahakitrungruang C, Pattana-Arun J, Khomvilai S, et al. Marsupialization for simple fistula in ano: a randomized controlled trial. J Med Assoc Thai. 2011;94:699–703. [PubMed] [Google Scholar]
- 31.Nazzer MA, Saleem R, Ali M. Better option for the patients of low fistula in ano: fistulectomy or fistulotomy. PJMHS. 2012;6:888–890. [Google Scholar]
- 32.Jain BK, Vaibhaw K, Garg PK, et al. Comparison of a fistulectomy and a fistulotomy with marsupialization in the management of a simple anal fistula: a randomized, controlled pilot trial. J Korean Soc Coloproctol. 2012;28:78–82. doi: 10.3393/jksc.2012.28.2.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Salem OTA. Fistulectomy and fistulotomy for low anal fistula. Rawal Med J. 2012;37:409–411. [Google Scholar]
- 34.Kamal ZB. Fistulotomy versus fistulectomy as a primary treatment of low fistula in ano. Iraqi Acad Sci J. 2012;11:510–515. [Google Scholar]
- 35.Wang C, Lu JG, Cao YQ, et al. Traditional Chinese surgical treatment for anal fistulae with secondary tracks and abscess. World J Gastroenterol. 2012;18:5702–5708. doi: 10.3748/wjg.v18.i40.5702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chalya PL, Mabula JB. Fistulectomy versus fistulotomy with marsupialisation in the treatment of low fistula-in-ano: a prospective randomized controlled trial. Tanzan J Health Res. 2013;15:193–198. doi: 10.4314/thrb.v15i3.7. [DOI] [PubMed] [Google Scholar]
- 37.Sheikh IA, Shukr I, Hanif MS, et al. Fistulotomy vs fistulectomy in the treatment of simple low anal fistula of male patients. Pak Armed Forces Med J. 2015;65:798–802. [Google Scholar]
- 38.Abramowitz L, Soudan D, Souffran M, et al. The outcome of fistulotomy for anal fistula at 1 year: a prospective multicentre French study. Colorectal Dis. 2016;18:279–285. doi: 10.1111/codi.13121. [DOI] [PubMed] [Google Scholar]
- 39.Elsebai O, Elsesy A, Ammar M, et al. Fistulectomy versus fistulotomy in the management of simple perianal fistula. Menoufia Med J. 2016;29:564–569. doi: 10.4103/1110-2098.198710. [DOI] [Google Scholar]
- 40.Limongelli P, Brusciano L, Del Genio G, et al. Marsupialization compared to open wound improves dressing change and wound care management after fistulectomy for low transsphincteric anal fistula. Int J Colorectal Dis. 2016;31:1081–1082. doi: 10.1007/s00384-015-2430-4. [DOI] [PubMed] [Google Scholar]
- 41.Saber A. Patients satisfaction and outcome of fistulotomy versus fistulectomy for low anal fistula. J Surg Spec Issue Gastrointest Surg Recent Trends. 2016;4:15–19. doi: 10.11648/j.js.s.2016040201.14. [DOI] [Google Scholar]
- 42.Vyas AK, Katlana A, Rathi A et al (2016) Comparison and evaluation of the outcome of fistulotomy vs fistulectomy technique in treatment of low fistula in ano. J Med Sci Clin Res 4:14999–15006. 10.18535/jmscr/v4i12.114.
- 43.Wang C, Rosen L. Management of low transsphincteric anal fistula with serial setons and interval muscle-cutting fistulotomy. J Integr Med. 2016;14:154–158. doi: 10.1016/S2095-4964(16)60229-7. [DOI] [PubMed] [Google Scholar]
- 44.Jayarajah U, Wickramasinghe DP, Samarasekera DN. Anal incontinence and quality of life following operative treatment of simple cryptoglandular fistula-in-ano: a prospective study. BMC Res Notes. 2017;10:572. doi: 10.1186/s13104-017-2895-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Murtaza G, Shaikh FA, Chawla T, et al. Fistulotomy versus fistulectomy for simple fistula in ano: a retrospective cohort study. J Pak Med Assoc. 2017;67:339–342. [PubMed] [Google Scholar]
- 46.Ganesan R, Karunakaran K, Anandan H (2017) A comparative study between fistulotomy and fistulectomy in management of low anal fistulae. Int Surg J. 4:3665–3669. 10.18203/2349-2902.isj20174882
- 47.Shahid M, Ahmed Z, Malik S. Management of low anal fistula: fistulectomy alone versus fistulectomy with primary closure. Pak Armed Forces Med J. 2017;67:203–206. [Google Scholar]
- 48.Vyas AK, Katlana A, Singh A et al (2017) Incidence of low fistula in ano and results of fistulotomy in rural tertiary centre. Ann Int Med Den Res 3:28–30. 10.21276/aimdr.2017.3.3.SG9
- 49.Mittal A, Sreeramulu PN, Shashirekha CA et al (2018) Comparative study of surgical management of low fistula-in-ano between fistulotomy & fistulectomy and its outcome. JMSCR 6:32657–32664. 10.18535/jmscr/v6i1.41
- 50.Gupta S, Goel A, Pathak V et al (2018) Comparative study between conventional fistulectomy and SLOFT in cases of low fistula in ano. Santosh Univ J Health Sci 4:91–94. 10.18231/2455-1732.2018.0021
- 51.Mallik NR, Nandi S, Saha AK et al (2018) Study of fistulotomy and fistulectomy in the management of low anal fistula and evaluation of short term outcomes. IOSR-JDMS 17:42–45. 10.9790/0853-1704124245
- 52.Anan M, Emile SH, Elgendy H et al (2019) Fistulotomy with or without marsupialisation of wound edges in treatment of simple anal fistula: a randomised controlled trial. Ann R Coll Surg Engl 101:472–478. 10.1308/rcsann.2019.0057 [DOI] [PMC free article] [PubMed]
- 53.Bhatia H. (2019) Excision of low fistula in ano under local anaesthesia. JMSCR 7:585–591. 10.18535/jmscr/v7i3.106
- 54.Sahai RN (2019) Fistulotomy or LIFT: which has better outcome in management of intersphincteric and low transphincteric fistula-in-ano—a randomized prospective study. IJARIIT 5(1). https://www.ijariit.com/
- 55.Sanad A, Emile S, Thabet W, et al. A randomized controlled trial on the effect of topical phenytoin 2% on wound healing after anal fistulotomy. Colorectal Dis. 2019;21:697–704. doi: 10.1111/codi.14580. [DOI] [PubMed] [Google Scholar]
- 56.Basa M, Prakash K (2020) A study on outcome of primary closure versus open fistulectomy in low level fistula in ano. Int Surg J 7:1015–1020. 10.18203/2349-2902.isj20201166
- 57.De Hous N, Van den Broeck T, de Gheldere C. Fistulectomy and primary sphincteroplasty (FIPS) to prevent keyhole deformity in simple anal fistula: a single-center retrospective cohort study. Acta Chir Belg. 2020 doi: 10.1080/00015458.2020.1753151. [DOI] [PubMed] [Google Scholar]
- 58.Cintron JR, Park JJ, Orsay CP et al (2000) Repair of fistulas-in-ano using fibrin adhesive: long-term follow-up. Dis Colon Rectum 43(7):944–949 (discussion 949–950). 10.1007/BF02237355 [DOI] [PubMed]
- 59.Mohammed MK (2004) Interstitial photocoagulation of low anal fistula using 810 nm diode laser: prospective study. Iraqi J Laser 3:43–50. https://www.iasj.net/iasj?func=fulltext&aId=45323
- 60.Gisbertz SS, Sosef MN, Festen S, et al. Treatment of fistulas in ano with fibrin glue. Dig Surg. 2005;22:91–94. doi: 10.1159/000085299. [DOI] [PubMed] [Google Scholar]
- 61.Barillari P, Basso L, Larcinese A, et al. Cyanoacrylate glue in the treatment of ano-rectal fistulas. Int J Colorectal Dis. 2006;21:791–794. doi: 10.1007/s00384-006-0090-0. [DOI] [PubMed] [Google Scholar]
- 62.Rojanasakul A, Pattanaarun J, Sahakitrungruang C, et al. Total anal sphincter saving technique for fistula-in-ano; the ligation of intersphincteric fistula tract. J Med Assoc Thai. 2007;90:581–586. [PubMed] [Google Scholar]
- 63.Chew SS, Adams WJ. Anal sphincter advancement flap for low transsphincteric anal fistula. Dis Colon Rectum. 2007;50:1090–1093. doi: 10.1007/s10350-006-0866-x. [DOI] [PubMed] [Google Scholar]
- 64.Jain SK, Kaza RC, Pahwa M, et al. Role of cyanoacrylate in the management of low fistula in ano: a prospective study. Int J Colorectal Dis. 2008;23:355–358. doi: 10.1007/s00384-007-0417-5. [DOI] [PubMed] [Google Scholar]
- 65.Mishra A, Shah S, Nar AS, et al. The role of fibrin glue in the treatment of high and low fistulas in ano. J Clin Diagn Res. 2013;7:876–879. doi: 10.7860/JCDR/2013/5387.2964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Van Onkelen RS, Gosselink MP, Schouten WR. Ligation of the intersphincteric fistula tract in low transsphincteric fistulae: a new technique to avoid fistulotomy. Colorectal Dis. 2013;15:587–591. doi: 10.1111/codi.12030. [DOI] [PubMed] [Google Scholar]
- 67.Oztürk E, Gülcü B. Laser ablation of fistula tract: a sphincter-preserving method for treating fistula-in-ano. Dis Colon Rectum. 2014;57:360–364. doi: 10.1097/DCR.0000000000000067. [DOI] [PubMed] [Google Scholar]
- 68.Cestaro G, De Rosa M, Gentile M. Treatment of fistula in ano with fibrin glue: preliminary results from a prospective study. Miner Chir. 2014;69:225–228. [PubMed] [Google Scholar]
- 69.Malakorn S, Sammour T, Khomvilai S, et al. Ligation of intersphincteric fistula tract for fistula in ano: lessons learned from a decade of experience. Dis Colon Rectum. 2017;60:1065–1070. doi: 10.1097/DCR.0000000000000880. [DOI] [PubMed] [Google Scholar]
- 70.Wilhelm A, Fiebig A, Krawczak M. Five years of experience with the FiLaCTM laser for fistula-in-ano management: long-term follow-up from a single institution. Tech Coloproctol. 2017;21:269–276. doi: 10.1007/s10151-017-1599-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Giordano P, Sileri P, Buntzen S, et al. Final results of a European, multicentre, prospective, observational study of PermacolTM collagen paste injection for the treatment of anal fistula. Colorectal Dis. 2018;20:243–251. doi: 10.1111/codi.13715. [DOI] [PubMed] [Google Scholar]
- 72.Terzi MC, Agalar C, Habip S, et al. Closing perianal fistulas using a laser: long-term results in 103 patients. Dis Colon Rectum. 2018;61:599–603. doi: 10.1097/DCR.0000000000001038. [DOI] [PubMed] [Google Scholar]
- 73.Marinello F, Kraft M, Ridaura N, et al. Treatment of fistula-in-ano with OTSC® proctology clip device: short-term results. Cir Esp. 2018;96:369–374. doi: 10.1016/j.ciresp.2018.02.003. [DOI] [PubMed] [Google Scholar]
- 74.Bayrak M, Altıntas Y. Permacol™ collagen paste injection in anal fistula treatment: a retrospective study with one-year follow-up. Adv Ther. 2018;35:1232–1238. doi: 10.1007/s12325-018-0743-8. [DOI] [PubMed] [Google Scholar]
- 75.Iqbal A, Ahmed T, Khan I, et al. Outcome of use of 1% silver nitrate in patients with low lying perianal fistula. J Ayub Med Coll Abbottabad. 2019;31:355–358. [PubMed] [Google Scholar]
- 76.Vander Mijnsbrugge GJH, Felt-Bersma RJF, Ho DKF, et al. Perianal fistulas and the lift procedure: results, predictive factors for success, and long-term results with subsequent treatment. Tech Coloproctol. 2019;23:639–647. doi: 10.1007/s10151-019-02023-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Toyonaga T, Matsushima M, Kiriu T, et al. Factors affecting continence after fistulotomy for intersphincteric fistula-in-ano. Int J Colorectal Dis. 2007;22:1071–1075. doi: 10.1007/s00384-007-0277-z. [DOI] [PubMed] [Google Scholar]
- 78.Litta F, Parello A, De Simone V, et al. Fistulotomy and primary sphincteroplasty for anal fistula: long-term data on continence and patient satisfaction. Tech Coloproctol. 2019;23:993–1001. doi: 10.1007/s10151-019-02093-9. [DOI] [PubMed] [Google Scholar]