Figure 1.
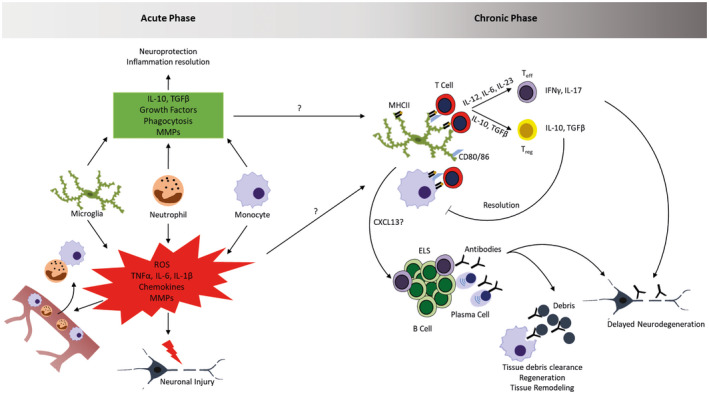
Inflammation in acute and chronic stroke lesions. Upon cerebral ischemia, tissue damage triggers the activation of microglia and the early infiltration of peripheral myeloid cells (neutrophils, monocytes). These cells contribute to tissue damage by the production of inflammatory mediators, reactive oxygen species (ROS) and MMPs, but also dampen this reaction and influence regeneration by releasing anti‐inflammatory mediators, growth factors, remove tissue debris and contribute to tissue remodeling. The mediators and molecular mechanisms influencing the transition from acute to chronic phase are currently unknown and a matter of active research. In this chronic phase where lymphocytes start infiltrating, myeloid cells can influence their function through antigen‐presentation and cytokine production. This leads to the generation of pro‐inflammatory T effector cells and anti‐inflammatory regulatory T cells. Through the release of chemokines, myeloid cells can potentially also influence the generation of B cell‐rich ectopic lymphoid structures (ELS) in which antibodies are produced. The generation of different T cell subsets and antibodies can promote delayed neurodegeneration, but potentially also contributes to tissue debris clearance and regenerative processes.
