Abstract
This study examined the effects of the Protecting Strong African American Families (ProSAAF) prevention program on adults’ self-reported health outcomes 25 months after enrollment. ProSAAF is a couple-focused prevention program specifically designed to meet the needs of African American families residing in the rural South. African American couples (N = 346) with an early adolescent child participated in a randomized controlled trial of the program. Dyadic data analyses indicated significant direct effects on changes in couple functioning post-intervention as well as significant indirect effects of ProSAAF on changes in health through post-intervention improvements in couple functioning. These benefits were documented for men’s and women’s general health, depressive symptoms, and problematic sleep. There were no significant direct effects of ProSAAF participation on changes in health. Findings provide tempered optimism regarding the potential benefits of couple-focused programming for adults’ physical, mental, and behavioral health.
Keywords: African Americans, couples, health, prevention, relationship satisfaction
Couple and relationship education (CRE) programs have been widely implemented to help couples maintain and strengthen their relationships. To date, most evaluations of these programs have focused primarily, if not exclusively, on outcomes such as couples’ relationship satisfaction and communication skills (see Fawcett, Hawkins, Blanchard, & Carroll, 2010; Markman & Rhoades, 2012). Yet couples’ relationship functioning also has important, albeit complex, implications for other aspects of individuals’ lives, including their health and well-being (e.g., Kiecolt-Glaser & Wilson, 2017; Proulx, Helms, & Buehler, 2007; Robles, Slatcher, Trombello, & McGinn, 2014). Indeed, one of the primary justifications for the growing dissemination of CRE programs has been their potential effects on the general health and well-being of couples and their children (e.g., Myrick, Ooms, & Patterson, 2009). Nonetheless, there has been little attention to whether these programs do in fact benefit couples’ health more generally. Moreover, the extant research on CRE programming and health rarely includes samples with high percentages of minority populations, despite the prominent and persistent health disparities that these populations experience (National Center for Health Statistics, 2016). The current study was designed to address these gaps by examining the effects of participation in the Protecting Strong African American Families (ProSAAF) program on a range of health outcomes among a sample of middle-aged African American couples living in the rural South.
Couples’ Interventions and Adult Health Outcomes
Although the effects of CRE programs on couples’ relationship outcomes are well-documented (for meta-analyses, see Cowan & Cowan, 2014; Hawkins, Blanchard, Baldwin, & Fawcett, 2008), studies investigating program effects on adults’ health and well-being remain scarce. This lack of research is in stark contrast to robust findings from descriptive, correlational studies indicating that supportive, stable couple relationships forecast improved health across a range of outcomes, including overall general health, depressive symptoms, substance use, and sleep quality (see Robles et al., 2014 for review). Unfortunately, non-experimental designs with purely correlational findings are limited in their ability to rule out the effect of potential confounding third variables, highlighting the unique value of examining these effects in the context of a randomized control trial (RCT) design.
The few studies that have examined CRE program effects on health reveal inconsistent results. In a study of distressed couples participating in the web-based OurRelationship program, participants in the intervention group relative to the control group reported decreased depressive and anxious symptoms as well as improved perceived health and quality of life shortly after program completion (Doss et al., 2016; also see Roddy, Rhoades, & Doss, 2020). Follow-up analyses also indicated that improvements in these domains of individual well-being were maintained over an approximately 12-month time period (Doss, Roddy, Nowlan, Rothman, & Christensen, 2019). A second study involving a community sample of Swiss couples who completed the Couples Coping Enhancement Training (CCET) program found that psychological health improved for women in the CCET condition relative to women in the control condition; no group differences were found with respect to men’s psychological health or physical health for either sex (Pihet, Bodenmann, Cina, Widmer, & Shantinath, 2007). In a third study, German couples who participated in the Ehevorbereitung – Ein Partnerschalftliches Lern-programm (Premarital Preparation – A Couples’ Learning Program; Hahlweg, Markman, Thurmaier, Engl, & Eckert, 1998) demonstrated reduced cortisol responses during laboratory-based couple conflict discussions at post-intervention, suggesting that couple conflicts were less physiologically arousing (Ditzen, Hahlweg, Fehm-Wolfsdorf, & Baucom, 2011). Results also indicated that this decrease in cortisol was partially mediated by increases in individuals’ reports of relationship quality linked to EPL. There is also evidence for null effects on adults’ health following CRE programming: as one example, Loew (2016) found no changes in health in a sample of older couples who participated in the Preparation and Relationship Enhancement Program (PREP; Markman, Renick, Floyd, Stanley, & Clements, 1993) relative to couples in the control condition (also see Halford et al., 2017).
Evaluations of psychoeducational programs for expectant and new parents also provide support of the potential health benefits of CRE participation, particularly with respect to mental health. Meta-analytic findings of these programs suggest significant effects on participants’ psychological and depressive symptoms (Pinquart & Teubert, 2010), though null findings also appear in this literature as well (e.g., Feinberg, Jones, Kan, & Goslin, 2010). Taken together, the existing literature contains mixed support for the idea that couple-focused preventive interventions are associated with positive outcomes for participants’ individual health, with stronger support for effects on participants’ mental health as compared to physical health.
As a final consideration, previous studies examining direct effects on adults’ health outcomes, though informative, may provide an incomplete test of how couple-focused prevention promotes health. As suggested by the basic research literature on marital functioning and health (Robles et al., 2014), any improvements in health following CRE participation would likely occur as a result of improvements in couple functioning. Thus, program effects on health, particularly in a community (i.e., non-distressed) sample, would be most appropriately modeled as indirect effects. In this formulation, CRE participation is expected to lead to improvements in couple functioning, which lead to improvements in health. Such mechanistic tests are rare, but are advantageous in providing clearer conceptual tests of program effects and greater statistical power to examine theoretically meaningful relationships (MacKinnon & Fairchild, 2009).
The Current Study
The current study aims to further our understanding of changes in adults’ health outcomes following participation in couple-focused prevention programming. Study hypotheses are tested using data from a community sample of rural African American adults participating in an RCT of the ProSAAF program. As described in earlier work (e.g., Barton, Beach, Wells, et al., 2018), ProSAAF is a family-centered prevention program for two-parent African American families with a preadolescent child living in the rural South designed to improve couples’ functioning in the short-to-moderate term, which in turn was expected to affect family members’ health and well-being. The program was successful in achieving its primary aims, leading to significant improvements in multiple dimensions of couples’ functioning over a 17-month period (Barton, Beach, Bryant, Lavner, & Brody, 2018; Barton et al., 2017; Barton, Beach, Wells, et al., 2018). These improvements in couple functioning provide a foundation for addressing whether there are direct or indirect benefits that extend to adults’ health as well.
The current study uses four waves of data spanning 25 months to examine ProSAAF’s direct and indirect effects on adults’ long-term health outcomes. Indirect effects are tested in line with prior research by examining the role of couple functioning in transmitting the effect of program participation on changes in secondary outcomes (e.g., Lavner, Barton, & Beach, 2019, 2020). To provide a robust assessment of ProSAAF’s effects on couples’ health and well-being, we investigate effects across mental, behavioral, and physical health domains, including general health, depressive symptoms, sleep problems, and problematic substance use.
Method
Participants and Procedures
Couples with an African American child between 9 and 14 years of age took part in the study.1 The study received approval from the Institutional Review Board (IRB) at The University of Georgia (title: “Protecting Strong African American Families”; IRB approval number: 20121041112) and was not pre-registered. Subject enrollment began in 2013 and continued into 2014 until reaching the target number of participants (sample size information in Supplemental Material). All participants lived in small towns in the southern US, where poverty rates are among the highest in the nation (DeNavas-Walt & Proctor, 2014). To be eligible, couples had to be in a relationship for 2 years or more, living together, and coparenting an African American child in the targeted age range for at least 1 year ((full study overview is provided in Barton, Beach, Wells, et al., 2018). Participant recruitment, randomization, and progress through the study are illustrated in the CONSORT flowchart (see Supplemental Figure S1; for CONSORT checklist, see Supplemental Table S1). A total of 1897 families were screened for eligibility. Of these families, 1145 were ineligible (e.g., single parent household, child was not African American). Of the 752 eligible families, 347 did not respond to the solicitation and 59 were unable to schedule an assessment. The remaining 346 families were randomized to the intervention (n = 172) or control (n = 174) condition.
Of the couples in the randomized sample, 63% were married, with a mean length of marriage of 9.8 years (SD = 7.48; range < 1 year to 56 years). Unmarried couples had been living together for an average of 6.7 years (SD = 5.42; range < 1 year to 24 years). Mean ages were 39.9 years (SD = 9.6; range 21 to 83 years) for men and 36.6 years (SD = 7.45; range 23 to 73 years) for women. The majority of families in the study could be classified as working poor: 51% had incomes below 100% of the federal poverty level and an additional 17% had incomes between 100% and 150% of that level. The majority of both men (74% [65% full-time]) and women (61% [45% full-time]) were employed. Median monthly income was $1,375 (SD = $1,375; range $1 to $7,500) for men and $1,220 (SD = $1,440; range $1 to $10,000) for women. Median education levels were high school or GED (ranging from less than grade 9 to a doctorate or professional degree) for men and some college or trade school (ranging from less than grade 9 to a master’s degree) for women. The total number of children residing in the home ranged from 1 to 8, with a median of 3 and a mode of 2 (M = 2.97; SD = 1.48). Nearly all couples were heterosexual (n = 344 [99.4%]); two families were headed by a same-sex female couple.2
Project staff visited couples’ homes, explained the study in greater detail, and obtained informed consent. Participants completed the W1 assessment using audio computer-assisted self-interview software installed on laptop computers. Participants completed surveys on separate laptops and, if possible, in separate rooms. Couples were visited for Wave 2 (W2), Wave 3 (W3), and Wave 4 (W4) assessments a mean of 9.4 months, 17.0 months, and 24.5 months respectively after W1. Each adult was compensated with a $50 check for each assessment. Randomization took place after couples completed pretest measures using computer-generated tables. Block randomization by marital status was performed within each county to facilitate group equivalence (additional randomization details are located in Supplemental Material).
For women and men in the intervention condition, respective retention was 84% and 81% at W2, 83% and 76% at W3, and was 80% and 72% at W4. For men and women in the control condition, respective retention was 89% and 82% at W2, 93% and 85% at W3, and was 95% and 82% at W4. Retention did not vary by primary study variables or sociodemographic variables (i.e., marital status, children in the home, income, education, and child age). At W3 and W4, control families were more likely to be retained than ProSAAF families (p < .05).
The Protecting Strong African American Families (ProSAAF) Program
Program overview.
ProSAAF was specifically designed to meet the needs of two-parent African American families residing in the rural South. Each session focused on a specific stressor that rural African American couples experience (e.g., work, racism, finances, extended family), and couples were instructed in cognitive and behavioral techniques for handling the stressor together. Sessions were organized around DVD presentations that taught program content and depicted scenarios of program-targeted interactions and behaviors. The primary focus of the intervention was the adult romantic-partner dyad, with additional content in each session on coparenting/parenting, youth development, and parent-child/family relationship quality. Sample couple-focused content included recognizing positive aspects of the partnership, identifying “beneath the surface” issues, strengthening couple identity and unity, and enhancing quality time together. Additional details about the program can be found in Barton and colleagues (2018). No harms or unintended effects were evident in either condition.
ProSAAF implementation.
Intervention facilitators were African American community members who received several days of curriculum training and ongoing supervision. The facilitator visited the couple in their home for six consecutive weeks. The first 60 minutes of each session focused on the couple’s relationship. The next 30 minutes of each session focused on parenting/coparenting topics. The facilitator then met with the target child for 15 minutes to discuss a youth-focused topic while the couple took a break in a different room. After the 15-minute youth activity, the entire family came back together for a 15-minute family activity.
Two booster sessions were scheduled to reinforce program material. If a couple separated or divorced, an alternative booster session was offered that focused on the coparenting relationship and protecting children from the stress of separation and divorce. Booster Session 1 was scheduled approximately 3 months after program completion (approximately 2 months before W2) and Booster Session 2 was scheduled approximately 9 months after program completion (approximately 4 months before W3). Following each intervention session, each adult was compensated for their time (Sessions 1 and 2 = $25, Sessions 3 and 4 = $30, Sessions 5 and 6 = $35, Booster Sessions 1 and 2 = $35). A total of 28 facilitators implemented the program; the total number of families with whom each facilitator worked ranged from 1 to 15.
Attendance.
Total sessions attended by families were as follows: 6 session, 81% (n = 139); 5 sessions, 0.6% (n = 1); 3 sessions, 2.9% (n = 5); 2 sessions, 2.3% (n = 4); 1 session, 4.1% (n = 7); and no sessions, 9.3% (n = 16). For booster sessions, attendance was: Booster Session 1, 73% (n = 126) and Booster Session 2, 59% (n = 101). All of the families to whom the alternative booster session was offered attended: 4% (n = 7).
Fidelity.
All sessions were audiotaped. A sample of sessions (n = 220, corresponding to 25% of all sessions) was coded using an 87- to 143-point checklist (depending on the session) for fidelity to intervention guidelines. All facilitators were assessed at least once. Of the audiotapes reviewed, 10% (n = 22) were coded by more than one rater (ICC = .94). The mean fidelity score across facilitators on a scale of 0–100% was 91% (SD = 9.0%).
Control group.
Couples in the control group were assessed on the same schedule as those in the ProSAAF group, thereby controlling for effects of repeated measurements, external social changes, maturation, and individual differences. After the pretest, couples were mailed the book 12 Hours to a Great Marriage (Markman, Stanley, Blumberg, Jenkins, & Whaley, 2004) and an accompanying workbook. Use of this material was not assessed.
Measures
Couple functioning.
To provide a global assessment of couple functioning at Waves 1, 2, and 3, we used a composite variable from our previous work that included partners’ ratings of effective communication, relationship confidence, relationship satisfaction, and perceived partner support (Lavner et al., 2019). All four variables were significantly correlated at each assessment (rs = .43 to .85, all ps < .001) and showed significant improvement following the intervention (Barton, Beach, Wells, et al., 2018). All scales were standardized within wave for men and for women, then averaged, and were scored such that higher scores indicated more positive couple functioning.
Effective communication was assessed using a seven-item version of the Communication Skills Test (Jenkins & Saiz, 1995). This measure has been used in prior studies with evidence for its internal consistency and validity (e.g., Stanley et al., 2001), including studies specifically with African American samples (Barton et al., 2016). Items, rated on a scale ranging from 1 (almost never) to 7 (almost always), were summed and used to assess the frequency of effective communication patterns between partners (sample item: “When discussing an issue, my mate and I both take responsibility to keep us on track”; men: α ≥ .84; women: α ≥ .86).
Relationship confidence was rated using the sum of four items from the Relationship Confidence Scale (RCS; Stanley, Hoyer, & Trathen, 1994). The RCS assesses partners’ confidence in the future of their relationship (sample item: “I am very confident when I think of my future with [partner name]”). Similar versions of the current scale have demonstrated good reliability and predictive validity (e.g., Whitton, Rhoades, & Whisman, 2014), including studies with predominantly African American samples (e.g., Owen, Quirk, Bergen, Inch, & France, 2012). In the current study, items were rated on a Likert scale ranging from 1 (strongly disagree) to 5 (strongly agree) (men: α ≥ .87; women: α ≥ .90).
Relationship satisfaction was assessed using the Quality of Marriage Index (QMI; Norton, 1983), one of the most widely-used measures of relationship satisfaction, including studies with African Americans couples (e.g., Fincham, Ajayi, & Beach, 2011). This six-item scale measures global perceptions of relationship satisfaction (sample question: “[Partner name] and I have a good relationship”) using a Likert scale ranging from 1 (strongly disagree [questions 1–5] and very unhappy [question 6]) to 5 (strongly agree [questions 1–5] and perfectly happy [question 6]) (men: α ≥ .92; women: α ≥ .93).
Perceived partner support was assessed using items from the Spouse Specific Social Support Scale (Culp & Beach, 1998). This scale is a reliable and valid measure of perceived spousal support among couples (including African American samples, e.g., Barton et al., 2016) and shows associations with relationship and individual well-being (Culp & Beach, 1998). Five items were summed to assess partners’ perceptions of their ability to confide in and receive support from one another (sample item: “[Partner’s name] is someone I can confide in”); the response set ranged from 1 (almost never) to 5 (almost always) (men: α ≥ .81; women: α ≥ .87).
Health outcomes.
Adults’ health at Wave 4 was measured across four different outcomes: self-reported health, depressive symptoms, sleep problems, and problematic substance use. Baseline levels for each health outcome were also included from the earliest available data collection point (W1 for depressive symptoms and problematic substance use; W2 for self-reported health and sleep problems).
Self-reported health.
Individuals reported their health problems at W2 and W4 using items from the General Health Perceptions subscale of the RAND 36-Item Short-Form Health Survey (Hays, Sherbourne, & Mazel, 1993). The 4-item subscale assessed perceptions of current health status, and response options ranged from 1 (strongly disagree) to 4 (strongly agree). Sample items include “I am as healthy as anybody I know” and “I seem to get sick a little easier than other people” (reverse scored). Responses were summed such that higher scores indicated better health (men: α > .65; women: α > .73).
Depressive symptoms.
Depressive symptoms were measured at W1 and W4 using 20 items from the Center for Epidemiological Studies - Depression (CES-D) scale, a commonly used measure for assessing mental health in community samples (Radloff, 1977). Sample items include “In the past week, how often did you feel depressed?” and “In the past week, how often did you think your life was a failure?” Response options, which ranged from 0 (Rarely or none of the time [0–1 day]) to 3 (Most or all of the time [6–7 days]), were summed such that higher scores indicated more depressive symptoms (men: α > .75; women: α > .85).
Sleep problems.
Participants reported their sleep problems at W2 and W4 using the Sleep Problems II subscale of the Medical Outcomes Scale (Spritzer & Hays, 2003). This six-item scale assesses the frequency of sleep disturbance, adequacy, somnolence, and awakening short of breath during the past four weeks. Sample items include how often did you “awaken from your sleep and have trouble falling asleep again” and “have trouble staying awake during the day.” Response options, which ranged from 1 (None of the time) to 5 (All of the time), were summed such that higher scores indicated more sleep problems (men: α > .71; women: α > .72).
Problematic substance use.
Substance use problems were assessed with 7 indicators of problematic substance use from prior research (Harrison, Fulkerson, & Beebe, 1998). As sample items, individuals endorsed (1 = Yes; 0 = No) in the past 6 months whether or not they had “used more alcohol or other drugs than you intended to” and “neglected your responsibilities because of alcohol or other drug use”. Responses were summed to create a count variable of the number of problematic substance use items endorsed.
Analytic Plan
Analyses were conducted using path analysis in Mplus version 8.1 (L. K. Muthén & Muthén, 2017). We ran two models for each of the four health outcomes. In the first model, we examined the direct effects of ProSAAF participation on changes in adult health at Wave 4 (i.e., ProSAAF assignment → W4 Health Outcome [controlling for W1 or W2 depending on outcome]). In the second model, we added men’s and women’s reports of couple functioning to examine if ProSAAF predicted changes in couple functioning, and if post-intervention couple functioning predicted later health outcomes (i.e., ProSAAF assignment → W2&W3 Couple Functioning [controlling for W1] → W4 Health Outcome [controlling for W1 or W2]). For this model, we also tested indirect effects from intervention to long-term health outcomes. Indirect effects were examined using 2,000 bias-corrected bootstrapped samples with 95% confidence intervals (CIs) involving unstandardized parameter estimates given the non-normal distribution of the product term comprising the indirect effect (Hayes, 2009). For count variables, indirect effects were calculated based on counterfactuals (causally-defined effects) as outlined by Muthén and Asparouhov (2015). As there were no sex-specific hypotheses, we constrained corresponding pathways to be equivalent for men and women (i.e., ProSAAF assignment → W2&W3 Couple Functioning as well as W2&W3 Couple Functioning → W4 Health Outcome).3 Given our interest in understanding whether short-term effects of the intervention predicted long-term changes in health, we conceptualized Waves 2 and 3 as representing short-term post-intervention effects (because families participated in booster sessions approximately 2 months before W2 and 4 months before W3, including both waves of data was necessary to capture the full post-intervention period) and thus averaged scores across W2 and W3 to create a single post-intervention variable to use in the mediation analyses as a predictor of health at W4.
All analyses were conducted according to an intent-to-treat (ITT) approach in which all couples assigned to the ProSAAF condition (regardless of program attendance) were compared to all couples assigned to the control condition. The ITT approach is recommended because it preserves randomization, provides a conservative estimate of program effects, and reflects practical community scenarios of noncompliance (Gupta, 2011). Missing data (11% of all valid cases) were handled using full information maximum likelihood estimation as applicable within Mplus. Overall model fit followed criteria by Marsh, Hau, and Wen (2004).
Results
Preliminary Analyses
Equivalence analyses indicated no differences between ProSAAF and control conditions at initial assessment for family characteristics, couple functioning, or health measures (see Table 1). Correlations among study variables are depicted in Supplemental Table S2. As most females (> 92%) reported no substance use problems at Wave 1, analyses of ProSAAF participation effects on problematic substance use were limited to men’s responses. For men, given the overdispersion of zeros (77% of sample at Wave 1), analyses of substance use problems utilized a zero-inflated Poisson distribution and results are presented in log count metrics.
Table 1.
Descriptive Statistics and Baseline Equivalence for Treatment and Control Groups (N = 344 couples)
| Gender | Treatment (n = 170) | Control (n = 174) | Test Statisticg | |||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| Demographic characteristics – baseline | ||||||
| Marrieda | 0.65 | n/a | 0.61 | n/a | 0.58 | |
| Children in home | 3.12 | 1.54 | 2.86 | 1.43 | 0.13 | |
| Incomeb | Men | 1.71 | 1.30 | 1.79 | 1.47 | 0.71 |
| Women | 1.72 | 1.45 | 1.50 | 1.18 | 0.28 | |
| Educationc | Men | 5.01 | 1.66 | 5.13 | 1.65 | 0.54 |
| Women | 5.94 | 1.90 | 5.76 | 1.70 | 0.40 | |
| Age | Men | 39.84 | 9.51 | 39.63 | 9.85 | 0.84 |
| Women | 36.30 | 7.00 | 36.76 | 7.87 | 0.57 | |
| Study variables – baseline | ||||||
| Couple functioning | Men | −0.19 | 3.66 | 0.19 | 2.96 | 1.10 |
| Women | −0.23 | 3.43 | 0.22 | 3.29 | 1.24 | |
| Self-reported healthd | Men | 12.11 | 2.27 | 12.56 | 2.29 | 1.64 |
| Women | 12.25 | 2.47 | 12.06 | 2.22 | 0.67 | |
| Depressive symptoms | Men | 11.09 | 6.41 | 10.86 | 7.24 | 0.32 |
| Women | 12.32 | 8.83 | 11.71 | 8.18 | 0.67 | |
| Sleep problemsd | Men | 14.27 | 3.88 | 13.40 | 4.26 | 1.78 |
| Women | 14.80 | 4.03 | 14.4 | 3.97 | 0.85 | |
| Problematic substance use | Men | 0.42 | 0.85 | 0.32 | 0.74 | 1.18 |
| Women | 0.10 | 0.48 | 0.14 | 0.50 | 0.72 | |
| Study variables – follow-up | ||||||
| Couple functioninge | Men | 0.85 | 5.50 | −0.76 | 6.36 | n/a |
| Women | 0.61 | 5.87 | −0.55 | 6.37 | n/a | |
| Self-reported healthf | Men | 12.00 | 2.18 | 12.22 | 2.26 | n/a |
| Women | 11.98 | 2.34 | 11.93 | 2.28 | n/a | |
| Depressive symptomsf | Men | 11.00 | 7.44 | 10.87 | 8.40 | n/a |
| Women | 13.28 | 10.03 | 12.30 | 9.82 | n/a | |
| Sleep problems (W4)f | Men | 13.34 | 4.00 | 12.94 | 4.36 | n/a |
| Women | 14.13 | 4.54 | 13.43 | 4.76 | n/a | |
| Problematic substance Usef | Men | 0.25 | 0.69 | 0.20 | 0.70 | n/a |
| Women | 0.11 | 0.43 | 0.08 | 0.44 | n/a | |
Note. Variables assessed at Wave 1 unless noted.
1 = Married (0 = Cohabiting).
Gross family monthly income divided by 1,000.
Range: 1 = Below grade 9; 11 = Doctorate or professional degree.
Assessed at W2.
Assessed at average of W2 and W3.
Assessed at W4.
T-test for continuous and ordinal variables; chi-square cross-tab statistic for binary variable.
Direct and Indirect Effects of ProSAAF on Health Outcomes
Our first set of models examined whether there was any direct effect of ProSAAF participation on changes in adult health outcomes. No significant direct effects of program participation were found for any of the health outcomes (see Supplemental Table S3).
Our second set of models introduced changes in couple functioning as a potential mechanism linking ProSAAF participation to health outcomes. Results from these models are summarized in Figure 1, panels A-D. As documented in prior studies (e.g., Lavner et al., 2019), ProSAAF participation had a significant effect on changes in couple functioning, with ProSAAF couples reporting greater improvements in couple functioning compared to control participants. Post-program relationship functioning, in turn, predicted change in each of the four health outcomes at Wave 4. In each instance, higher levels of relationship functioning predicted improved health at Wave 4: increased general health (B [β men, β women] = 0.03 [.08, .08], p = .02), decreased depressive symptoms (B [β men, β women] = −0.29 [−.22; −.18], p < .01), decreased sleep problems (B [β men, β women] = −0.10 [−.15; −.14], p < .01), and decreased problematic substance use (log count B = −0.09, p < .01). For each continuous outcome, indirect effect (IE) analyses indicated post-program levels of couple functioning significantly transmitted the effect of ProSAAF participation to health outcomes. Specifically, significant indirect effects were documented for higher levels of general health (IE = .056, 95% CI [.005, .139]), lower levels of depressive symptoms (IE = −0.539, 95% CI [−1.012, −0.240]), and lower levels of sleep problems (IE = −.201, 95% CI [−.375,−.092]). The total natural indirect effect for problematic substance use was not significant (IE = −.021, 95% CI [−.072, .002]).
Figure 1.
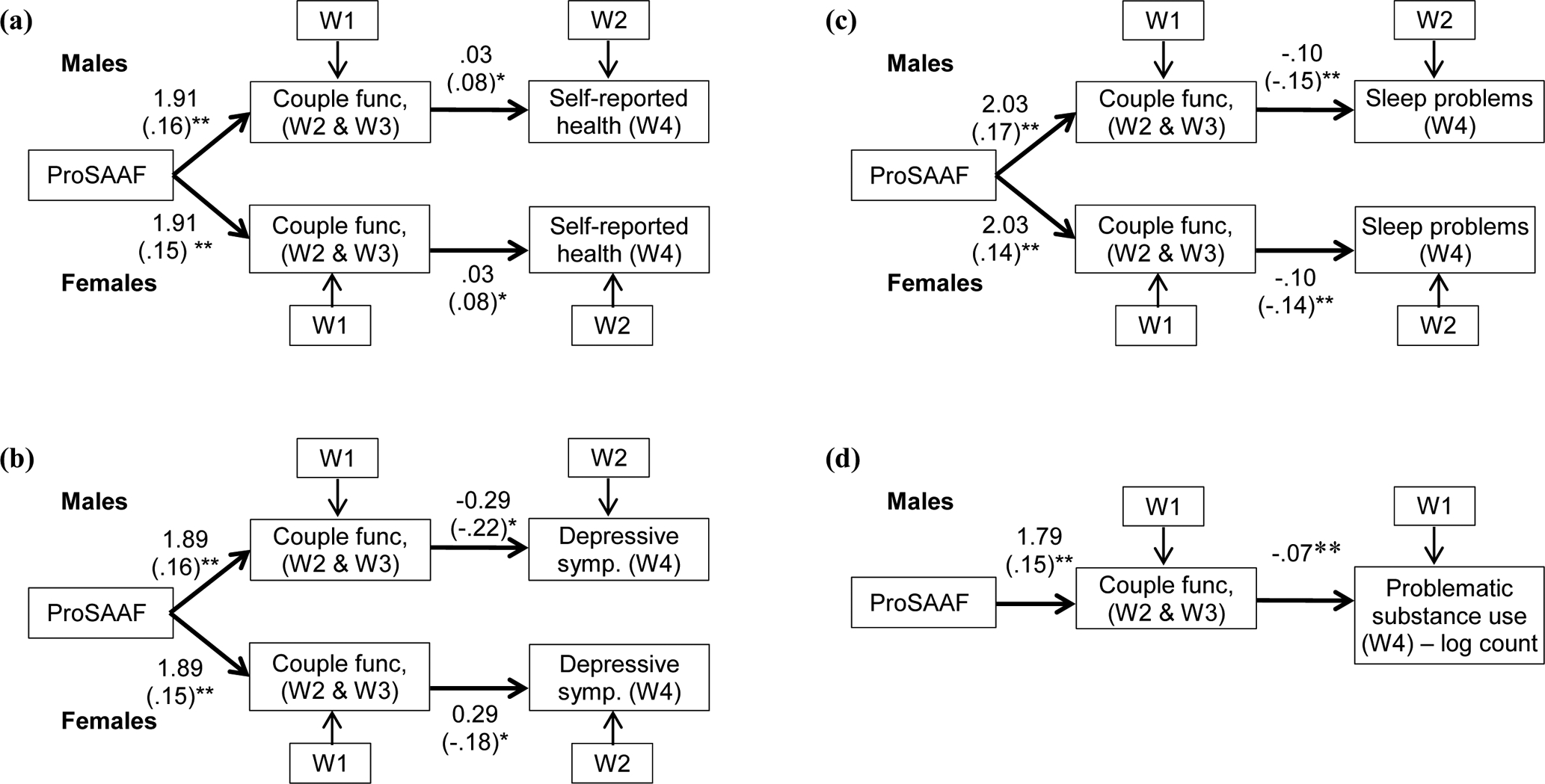
Path models depicting ProSAAF’s indirect effects on changes in (a) self-reported health (N=344), (b) depressive symptoms (n=344), (c) sleep problems (n=297), and (d) problematic substance use (n=304) through changes in couple functioning (CF). Unstandardized and standardized coefficients reported, with standardized coefficients in parentheses.
* p < .05.
** p < .01
Posthoc analyses.
We also conducted exploratory posthoc analyses to examine partner effects from couple functioning to health outcomes (i.e., ProSAAF assignment → W2&W3 Couple Functioning [controlling for W1] → partner’s W4 Health Outcome [controlling for W1/W2]) through Actor-Partner Interdependence Modeling. These analyses allowed us to examine the degree to which individuals’ post-program levels of couple functioning might be consequential for the health outcomes of their partner, controlling for the individual’s own report of couple functioning. For these analyses, partner effects were freely estimated (i.e., not constrained) from men to women and women to men. Results from these models (available from first author) indicated no significant partner effects for men or for women, with only one partner effect even approaching significance (i.e., women’s reports of higher post-intervention couple functioning were associated with decreases in men’s depressive symptoms at W4 ([p = .055]).
Discussion
Can interventions that strengthen couples’ relationships confer additional benefits for individuals’ health? Few studies of CRE programming to date have empirically examined this question, despite the widespread dissemination of CRE programming (at times justified as a means to promote adults’ health and well-being) as well as robust empirical literature documenting associations between couple functioning and health (Myrick et al., 2009; Robles et al., 2014). The current study helped to address this gap by examining the degree to which a preventive intervention for rural African American couples might directly or indirectly benefit individuals’ health as well. Findings indicated that participation in ProSAAF resulted in positive indirect effects on several health outcomes through improvements in couple functioning, lending some support to the hypothesis that couple-focused interventions can improve the health of participants in several ways. We also note, however, that there were no direct effects of ProSAAF on health, resulting in a pattern of indirect effects only.
Collectively, we view these findings as providing cause for tempered optimism regarding the potential benefits of couple-focused programming on health outcomes. Significant indirect effects were observed for changes in men and women’s general health, depressive symptoms, and sleep problems. Aligning with findings by Ditzen (2011), post-program relationship functioning served as an intervening variable linking CRE participation to changes in health. That effects were documented across a range of modestly correlated health outcomes is notable and further underscores the potential value of supportive relationship functioning for positively influencing multiple aspects of rural African American adults’ health and well-being. No partner effects from relationship functioning to health outcomes were evident; this is consistent with prior research that reports few to no partner effects between couple relationship functioning and health outcomes (Choi, Yorgason, & Johnson, 2015; Whisman, Robustelli, & Labrecque, 2018).
The lack of significant direct effects of ProSAAF on health also introduces a cautionary note and adds to a pattern of mixed results in this emerging area of research. The current null findings regarding direct effects on all health outcomes are consistent with some prior work showing no direct effects of CRE programming on health (e.g., Loew, 2016), but are in contrast with other studies (e.g., Doss et al., 2016). Although there are likely multiple factors that account for these mixed findings, we highlight two here. One possible contributing factor is differences in the degree of initial relationship distress, or help-seeking status, within each study’s sample. More relationally distressed couples, including those specifically seeking help for their relationship, presumably have the most to benefit – as a couple and as individuals – from a program that seeks to improve their romantic relationship. Consistent with this position, the strongest findings in support of CRE effects on health appeared in a study involving help-seeking couples with one or both partners reporting relationship distress (Doss et al., 2016). In contrast, in community samples, there are likely to be a greater percentage of couples who were relatively well-functioning, suggesting that there may be ceiling effects as to the possible benefits of the intervention for their individual (and relational) well-being.
Another possible factor explaining differences across studies involves length of follow-up. The current study examined effects over a 25-month period, which included more than 18 months on average following completion of the six-session program. Previous studies documenting program effects have examined health outcomes at a much shorter interval post-intervention (e.g., Ditzen et al., 2011; Doss et al., 2016), raising the possibility that effects on health are more apparent at shorter time intervals following program completion. These results and others highlight how understanding whether, how, and when romantic relationships influence health is multifaceted and complex, involving bidirectional, multi-level pathways that span immediate and long-term temporal associations (see Kiecolt-Glaser & Wilson, 2017; Robles et al., 2014 for reviews and additional discussion). Accordingly, careful attention is needed when interpreting findings and making generalizations with studies in this area.
With respect to the lack of direct effects on health, it is also worth noting that the ProSAAF program was designed primarily to improve the couple relationship functioning and not physical, mental, or behavioral health. As such, the core constructs targeted by the program most directly related to the strength and stability of the couple relationship. To the degree that improving adults’ physical and mental health are a more explicit goal of a CRE program, programs may need to be adapted to target those dimensions of relationship functioning that most strongly link to health outcomes. Speculatively, constructs such as concerns of marital instability and rumination may be particularly relevant for CRE programs that aim to have more direct effects on health (Sansone & Sansone, 2012; Thoits, 2011). Given that our findings were limited to indirect effects with small effect sizes, we caution against viewing these types of CRE programs as secondary or tertiary prevention in populations where general health, depression, sleep, and substance use are primary concerns. Obtaining clinically-meaningful change with community samples, many of whom are not relationally distressed or meeting clinical thresholds for poor health, may be beyond the scope of CRE programming. Emerging findings do suggest, however, that this type of programming with more distressed and help-seeking couples may produce more clinically-meaningful changes in individuals’ health (Roddy et al., 2020).
In the current study, our composite variable of four indices of relationship functioning was found to link program participation to individual health outcomes. Although identifying the precise mechanism(s) accounting for this effect is beyond the scope of current study, we speculate that changes in participants’ cognitions about, and behaviors in, their relationship decreased levels of negative affect and personal distress as well as increased levels of relationship optimism and closeness, which collectively conferred benefits to various areas of individual health. Identifying relationship processes that have the strongest direct effect on individuals’ health, as well as new preventive interventions that target these constructs, remains a promising area for future research. We caution, however, against an overly reductionist perspective that seeks to identify a singular, or very small set, of mechanistic variable(s), as change across a collection of cognitive, affective, behavioral, and biological variables may be responsible for the influence of romantic relationships on health (see Robles et al., 2014).
Several limitations of the current investigation should be noted. First, all measures were based on self-reports. Future research with home-based observations of change in couple interactions and more extensive assessments of individuals’ physical health, including biomarkers of health-related processes and direct physical examination, would be valuable. Second, initial assessments of general health and sleep problems did not occur until W2, precluding our ability to compare groups at baseline as well as our ability to control for pre-intervention levels. Third, the sample was generally healthy, and stronger effects may be evident in a sample with more health problems. Fourth, the current study required dyadic participation by couples, potentially resulting in a sample with higher levels of relationship functioning than the general population (Barton, Lavner, Stanley, Johnson, & Rhoades, 2020). Fifth, although the exclusive African American sample is a strength of the study in certain respects, it also represents a potential limitation for the generalizability of findings to couples with different demographics or confronting different patterns of chronic or community stress. Finally, as with all evaluations of CRE programming, results of the study may be specific to the ProSAAF program, and may or may not be generalizable to other CRE programs.
Notwithstanding these limitations, results from this study indicate that the ProSAAF intervention yielded positive effects on changes in health through improvements in couples’ functioning. The findings advance our understanding of the possible health effects of participating in a couple-focused preventive intervention. In doing so, these findings underscore the value of examining outcomes beyond relationship functioning in order to provide a more complete picture of the potential benefits of these interventions. Further research investigating novel programs and delivery methods that can strengthen couples’ relationship quality as well as individual health, particularly among populations at risk for increased relationship instability and chronic health problems, is needed.
Supplementary Material
Funding.
This research was supported by Award Numbers R01 HD069439 from the National Institute of Child Health and Human Development and R01 AG059260 from the National Institute on Aging to Steven R. H. Beach as well as P50 DA051361 from the National Institute on Drug Abuse to Gene H. Brody. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of a an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
Data is available for review upon request to the first author.
Disclosure of potential conflicts of interest. The authors report no conflicts of interest.
Research involving human participants. All procedures were approved by the Institutional Review Board of the university at which the research was conducted and complied with the 1964 Helsinki declaration and its later amendments.
Informed consent. Informed consent was obtained from all couples prior to data collection and program participation.
To be eligible, the target child to be African American, but not both parents. Ethnicity was not assessed in surveys completed by participants. Notes from research staff indicated that two caregivers (from different families) were not African American. All participants were comfortable being identified as part of an African American family.
These two couples were excluded from analyses because data analytic techniques required dyads to be distinguishable by sex, and this subsample size precluded group comparisons.
Analyses comparing constrained models to the unconstrained model indicted no significant deterioration in model fit by imposing these equality constraints.
References
- Barton AW, Beach SRH, Bryant CM, Lavner JA, & Brody GH (2018). Stress spillover, African Americans’ couple and health outcomes, and the stress-buffering effect of family-centered prevention. Journal of Family Psychology, 32(2), 186–196. 10.1037/fam0000376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barton AW, Beach SRH, Hurt TR, Fincham FD, Stanley SM, Kogan SM, & Brody GH (2016). Determinants and long-term effects of attendance levels in a marital enrichment program for African American couples. Journal of Marital and Family Therapy, 42(2), 272–287. 10.1111/jmft.12126 [DOI] [PubMed] [Google Scholar]
- Barton AW, Beach SRH, Lavner JA, Bryant CM, Kogan SM, & Brody GH (2017). Is communication a mechanism of relationship education effects among rural African Americans? Journal of Marriage and Family, 79(5), 1450–1461. 10.1111/jomf.12416 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barton AW, Beach SRH, Wells AC, Ingels JB, Corso PS, Sperr MC, … Brody GH (2018). The Protecting Strong African American Families program: A randomized controlled trial with rural African American couples. Prevention Science, 19(7), 904–913. 10.1007/s11121-018-0895-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barton AW, Lavner JA, Stanley SM, Johnson MD, & Rhoades GK (2020). “Will you complete this survey too?” Differences between individual versus dyadic samples in relationship research. Journal of Family Psychology, 34(2), 196–203. 10.1037/fam0000583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi H, Yorgason JB, & Johnson DR (2015). Marital quality and health in middle and later adulthood: Dyadic associations. The Journals of Gerontology: Series B, 71(1), 154–164. 10.1093/geronb/gbu222 [DOI] [PubMed] [Google Scholar]
- Cowan PA, & Cowan CP (2014). Controversies in couple relationship education (CRE): Overlooked evidence and implications for research and policy. Psychology, Public Policy, and Law, 20(4), 361–383. 10.1037/law0000025 [DOI] [Google Scholar]
- Culp LN, & Beach SRH (1998). Marriage and depressive symptoms. Psychology of Women Quarterly, 22(4), 647–663. 10.1111/j.1471-6402.1998.tb00183.x [DOI] [Google Scholar]
- DeNavas-Walt C, & Proctor BD (2014). Income and poverty in the United States: 2013 (Current Population Reports P60–249). Washington, DC: U.S. Census Bureau. [Google Scholar]
- Ditzen B, Hahlweg K, Fehm-Wolfsdorf G, & Baucom D (2011). Assisting couples to develop healthy relationships: Effects of couples relationship education on cortisol. Psychoneuroendocrinology, 36(5), 597–607. 10.1016/j.psyneuen.2010.07.019 [DOI] [PubMed] [Google Scholar]
- Doss BD, Cicila LN, Georgia EJ, Roddy MK, Nowlan KM, Benson LA, & Christensen A (2016). A randomized controlled trial of the web-based OurRelationship program: Effects on relationship and individual functioning. Journal of Consulting and Clinical Psychology, 84(4), 285–296. 10.1037/ccp0000063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doss BD, Roddy MK, Nowlan KM, Rothman K, & Christensen A (2019). Maintenance of gains in relationship and individual functioning following the online OurRelationship program. Behavior Therapy, 50(1), 73–86. 10.1016/j.beth.2018.03.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fawcett EB, Hawkins AJ, Blanchard VL, & Carroll JS (2010). Do premarital education programs really work? A meta-analytic study. Family Relations, 59(3), 232–239. 10.1111/j.1741-3729.2010.00598.x [DOI] [Google Scholar]
- Feinberg ME, Jones DE, Kan ML, & Goslin MC (2010). Effects of family foundations on parents and children: 3.5 years after baseline. Journal of Family Psychology, 24(5), 532–542. 10.1037/a0020837 [DOI] [PubMed] [Google Scholar]
- Fincham FD, Ajayi C, & Beach SRH (2011). Spirituality and marital satisfaction in African American couples. Psychology of Religion and Spirituality, 3(4), 259–268. 10.1037/a0023909 [DOI] [Google Scholar]
- Gupta SK (2011). Intention-to-treat concept: A review. Perspectives in Clinical Research, 2(3), 109–112. 10.4103/2229-3485.83221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahlweg K, Markman HJ, Thurmaier F, Engl J, & Eckert V (1998). Prevention of marital distress: Results of a German prospective longitudinal study. Journal of Family Psychology, 12(4), 543–556. 10.1037/0893-3200.12.4.543 [DOI] [Google Scholar]
- Halford WK, Rahimullah RH, Wilson KL, Occhipinti S, Busby DM, & Larson J (2017). Four year effects of couple relationship education on low and high satisfaction couples: A randomized clinical trial. Journal of Consulting and Clinical Psychology, 85(5), 495–507. 10.1037/ccp0000181 [DOI] [PubMed] [Google Scholar]
- Harrison PA, Fulkerson JA, & Beebe TJ (1998). DSM-IV substance use disorder criteria for adolescents: A critical examination based on a statewide school survey. American Journal of Psychiatry, 155(4), 486–492. 10.1176/ajp.155.4.486 [DOI] [PubMed] [Google Scholar]
- Hawkins AJ, Blanchard VL, Baldwin SA, & Fawcett EB (2008). Does marriage and relationship education work? A meta-analytic study. Journal of Consulting and Clinical Psychology, Vol. 76, pp. 723–734. 10.1037/a0012584 [DOI] [PubMed] [Google Scholar]
- Hayes AF (2009). Beyond Baron and Kenny: Statistical mediation analysis in the new millennium. Communication Monographs, 76(4), 408–420. 10.1080/03637750903310360 [DOI] [Google Scholar]
- Hays RD, Sherbourne CD, & Mazel RM (1993). The RAND 36-item health survey 1.0. Health Economics, 2, 217–227. 10.1002/hec.4730020305 [DOI] [PubMed] [Google Scholar]
- Jenkins NH, & Saiz CC (1995). The Communication Skills Test. Denver, CO: Unpublished manuscript, University of Denver. [Google Scholar]
- Kiecolt-Glaser JK, & Wilson SJ (2017). Lovesick: How couples’ relationships influence health. Annual Review of Clinical Psychology, 13(1), 421–443. 10.1146/annurev-clinpsy-032816-045111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavner JA, Barton AW, & Beach SRH (2019). Improving couples’ relationship functioning leads to improved coparenting: A randomized controlled trial with rural African American couples. Behavior Therapy, 50(6), 1016–1029. 10.1016/j.beth.2018.12.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavner JA, Barton AW, & Beach SRH (2020). Direct and indirect effects of a couple-focused preventive intervention on children’s outcomes: A randomized controlled trial with African American families. Journal of Consulting and Clinical Psychology, 88(8), 696–707. 10.1037/ccp0000589 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Loew BA (2016). Internet Delivery of PREP-based Relationship Education for Older Couples. Denver University. [Google Scholar]
- MacKinnon DP, & Fairchild AJ (2009). Current directions in mediation analysis. Current Directions in Psychological Science, 18(1), 16–20. 10.1111/j.1467-8721.2009.01598.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markman HJ, Renick MJ, Floyd FJ, Stanley SM, & Clements M (1993). Preventing marital distress through communication and conflict management training: A 4- and 5-year follow-up. Journal of Consulting and Clinical Psychology, 61(1), 70–77. 10.1037/0022-006X.61.1.70 [DOI] [PubMed] [Google Scholar]
- Markman HJ, & Rhoades GK (2012). Relationship education research: Current status and future directions. Journal of Marital and Family Therapy, 38(1), 169–200. 10.1111/j.1752-0606.2011.00247.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markman HJ, Stanley SM, Blumberg S, Jenkins NH, & Whaley C (2004). Twelve Hours to a Great Marriage. San Francisco: Jossey-Bass. [Google Scholar]
- Marsh HW, Hau K-T, & Wen Z (2004). In search of golden rules: Comment on hypothesis-testing approaches to setting cutoff values for fit indexes and dangers in overgeneralizing Hu and Bentler’s (1999) findings. Structural Equation Modeling: A Multidisciplinary Journal, 11(3), 320–341. 10.1207/s15328007sem1103_2 [DOI] [Google Scholar]
- Muthén B, & Asparouhov T (2015). Causal effects in mediation modeling: An introduction with applications to latent variables. Structural Equation Modeling: A Multidisciplinary Journal, 22(1), 12–23. 10.1080/10705511.2014.935843 [DOI] [Google Scholar]
- Muthén LK, & Muthén BO (2017). Mplus User’s Guide. (8th ed.). Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Myrick M, Ooms T, & Patterson P (2009). Healthy Marriage and Relationship Programs: A Promising Strategy for Strengthening Families. Retrieved from https://www.healthymarriageinfo.org/wp-content/uploads/2017/12/Healthy-Marriage-and-Relationship.pdf
- National Center for Health Statistics. (2016). Health, United States, 2015: With Special Feature on Racial and Ethnic Health Disparities. Hyattsville, MD. [PubMed] [Google Scholar]
- Norton R (1983). Measuring marital quality: A critical look at the dependent variable. Journal of Marriage and Family, 45(1), 141–151. Retrieved from http://www.jstor.org/stable/351302 [Google Scholar]
- Owen J, Quirk K, Bergen C, Inch LJ, & France T (2012). The effectiveness of PREP with lower-income racial/ethnic minority couples. Journal of Marital and Family Therapy, 38, 296–307. 10.1111/j.1752-0606.2012.00294.x [DOI] [PubMed] [Google Scholar]
- Pihet S, Bodenmann G, Cina A, Widmer K, & Shantinath S (2007). Can prevention of marital distress improve well-being? A 1 year longitudinal study. Clinical Psychology & Psychotherapy, 14(2), 79–88. 10.1002/cpp.522 [DOI] [Google Scholar]
- Pinquart M, & Teubert D (2010). Effects of parenting education with expectant and new parents: A meta-analysis. Journal of Family Psychology, Vol. 24, pp. 316–327. 10.1037/a0019691 [DOI] [PubMed] [Google Scholar]
- Proulx CM, Helms HM, & Buehler C (2007). Marital quality and personal well-being: A meta-analysis. Journal of Marriage and Family, 69(3), 576–593. 10.1111/j.1741-3737.2007.00393.x [DOI] [Google Scholar]
- Radloff LS (1977). The CES–D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement, 1(3), 385–401. 10.1177/014662167700100306 [DOI] [Google Scholar]
- Robles TF, Slatcher RB, Trombello JM, & McGinn MM (2014). Marital quality and health: A meta-analytic review. Psychological Bulletin, 140(1), 140–187. 10.1037/a0031859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roddy MK, Rhoades GK, & Doss BD (2020). Effects of ePREP and OurRelationship on Low-Income Couples’ Mental Health and Health Behaviors: a Randomized Controlled Trial. Prevention Science, 21, 861–871. 10.1007/s11121-020-01100-y [DOI] [PubMed] [Google Scholar]
- Sansone RA, & Sansone LA (2012). Rumination: relationships with physical health. Innovations in Clinical Neuroscience, 9(2), 29–34. Retrieved from https://www.ncbi.nlm.nih.gov/pubmed/22468242 [PMC free article] [PubMed] [Google Scholar]
- Spritzer KL, & Hays RD (2003). MOS sleep scale: A manual for use and scoring, version 1.0 Los Angeles, CA. [Google Scholar]
- Stanley SM, Hoyer L, & Trathen DW (1994). The Confidence Scale. In Unpublished manuscript. Denver, CO: University of Denver. [Google Scholar]
- Stanley SM, Markman HJ, Prado LM, Olmos-Gallo PA, Tonelli L, St. Peters M, … Whitton SW (2001). Community-based premarital prevention: Clergy and lay leaders on the front lines*. Family Relations, 50(1), 67–76. 10.1111/j.1741-3729.2001.00067.x [DOI] [Google Scholar]
- Thoits PA (2011). Mechanisms linking social ties and support to physical and mental health. Journal of Health and Social Behavior, 52(2), 145–161. 10.1177/0022146510395592 [DOI] [PubMed] [Google Scholar]
- Whisman MA, Robustelli BL, & Labrecque LT (2018). Specificity of the association between marital discord and longitudinal changes in symptoms of depression and generalized anxiety disorder in the Irish longitudinal study on ageing. Family Process, 57(3), 649–661. 10.1111/famp.12351 [DOI] [PubMed] [Google Scholar]
- Whitton SW, Rhoades GK, & Whisman MA (2014). Fluctuation in relationship quality over time and individual well-being: Main, mediated, and moderated effects. Personality and Social Psychology Bulletin, 40(7), 858–871. 10.1177/0146167214528988 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


