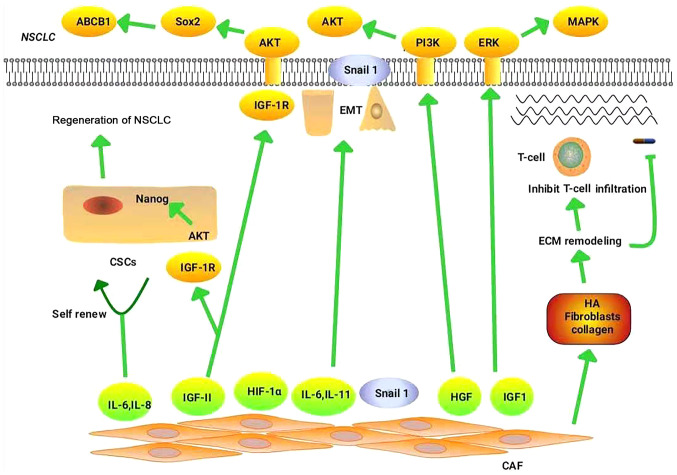
Figure 1.
Mechanism of CAFs in NSCLC drug resistance. CD10+/GPR77+CAFs can maintain the stemness of CSCs by secreting IL-6 and IL-8, thereby promoting drug resistance in patients with NSCLC. CAFs promote NSCLC resistance mainly through the following pathways: HGF/PI3K/AKT, IGF-II/IGF1R/Nanog, IGF-II/IGF-1R/AKT/Sox2/ABCB1 and IGF1/IGF1R/ERK/MAPK. CAFs increase TGF-β1-induced EMT in NSCLC by secreting IL-6. CAFs promote NSCLC drug resistance by regulating the hypoxic microenvironment through high expression of HIF-1α. CAFs deliver Snail to lung cancer cells through exosomes, which induce EMT in these cells and promote drug resistance. CAFs increase the stiffness of the matrix by enhancing ECM components (such as HA, fibroblasts and collagen), thereby preventing the binding of immune checkpoint inhibitors to their receptors, and prevent the infiltration and migration of immune cells, thereby promoting immune escape. In addition, ECM stiffness functions as a barrier to tumor cell drug absorption. CAF, cancer-associated fibroblast; NSCLC, non-small cell lung cancer; CSCs, cancer stem cells; IL, interleukin; HGF, hepatocyte growth factor; PI3K, phosphatidylinositol 3 kinase; AKT, protein kinase B; IGF-II, insulin-like growth factor-II; IGF1R, insulin-like growth factor 1 receptor; ABCB1, ATP-binding cassette sub-family B member 1; ERK, extracellular signal-regulated kinases; MAPK, mitogen-activated protein kinase; TGF-β1, transforming growth factor-β1; HIF-1α, hypoxia-inducible factor-1α; EMT, epithelial-mesenchymal transition; ECM, extracellular matrix; HA, hyaluronic acid.