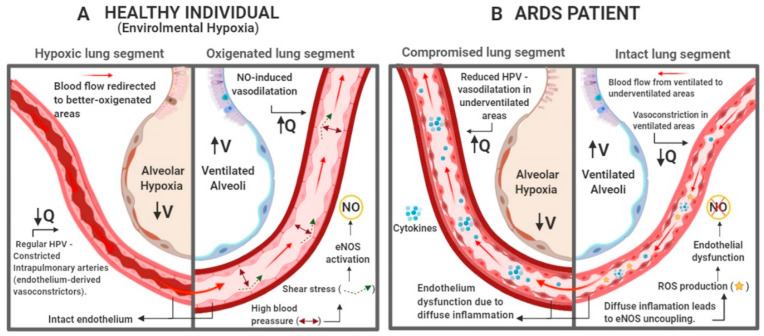
Fig. 1.
Implications of ARDS in hypoxic pulmonary vasoconstriction (HPV). (A) In individuals with intact endothelium, alveolar hypoxia induces vasoconstriction in intrapulmonary arteries, redirecting blood flow to well ventilated areas. The blood pressure in arteries near ventilated alveoli rises, which in turn promotes shear stress, induces eNOS activity and increases the concentration of endothelium-derived vasodilators, like NO, inhibiting HPV and promoting widening of vessel diameter. This regulation causes the blood to flow in direction of well-ventilated areas, improving V/Q [[35], [36], [37]]. (B) In ARDS patients, the diffuse inflammation causes endothelial dysfunction in intrapulmonary arteries, causing reduction of HPV. In this situation, the production of endothelium-derived vasoconstrictors (endothelin and thromboxane) is disrupted, causing relaxation of vessel walls in underventilated areas. Once the blood flow is not redirected to well ventilated areas and the activation of eNOS by shear does not occur, inhibiting the production of endothelium-derived vasodilators. These events may cause redirection of blood flow to areas were gas exchange is compromised, worsening V/Q [34,38]. Created with BioRender.com.