Highlights
-
•
Several complications after corona viral infection-19 (COVID-19) have been reported.
-
•
Some of these complications may require surgical intervention.
-
•
Aspergillosis is one of the COVID-19 complications.
-
•
In this study a case with post-COGID-19 pulmonary fungal infection is discussed.
Keywords: COVID-19, Fungal infection, Complications, CAPA
Abstract
Introduction and importance
Several complications after corona viral infection-19 (COVID-19) have been reported. The study aims is to present a case with post-covid-19 pulmonary fungal infection with antifungal resistance characteristics.
Case presentation
A 50-year-old male presented with hemoptysis, dyspnea, cough, fever, and rigor for 4-month duration. Three weeks before this complaint, he had cured of COVID-19. Investigations showed multiple ill-defined cavitary lesions involving the left upper lobe. The patient underwent a left upper lobectomy. The post-operative period was uneventful.
Clinical discussion
All studies of COVID-19 fungal infections reported occurrence during the COVID-19 infection, mostly 14 days after the appearance of COVID-19 symptoms. The case in the current study was a 50-year-old patient, who was previously diagnosed with COVID-19 for a period of 4 months. After a few days from his recovery, the patient developed dyspnea, cough, fever, and rigor again.
Conclusion
Pulmonary aspergillosis is a serious complication of COVID-19 patients that may not respond well to medical therapy. Pulmonary resection is the last and effective strategy to control the disease.
1. Introduction
The coronavirus disease-2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) appeared first in Wuhan, China, in December 2019, which rapidly spread to become a pandemic disease, as such, it is now present in all of the continents, causing quarantine and lockdown in populated areas. Most patients with COVID-19 disease may have no or very mild symptoms such as fever and dry cough, but in severe cases, especially in elderly, hypertensive, and diabetic patients, SARS-CoV-2 can cause severe acute respiratory syndrome (SARS) [1]. SARS-CoV-2 is primarily associated with the infection of the lungs causing pneumonia, but recent studies have revealed that many other organs can be affected, including cardiovascular, immune, nervous, and gastrointestinal systems [2]. According to the published reports, a portion (7.2%) of COVID-19 patients are sometimes co-infected by other microbial pathogens, adding to the severity of these cases and raising difficulty in the diagnosis, prognosis, and treatment [3,4]. Hence, hospitalized COVID-19 patients are prescribed anti-microbial agents due to uncertainty, which poses a risk of the selecting of anti-microbial resistance bacteria and fungi that can cause superinfections [5].
The study aims to present a case with post-covid-19 pulmonary fungal infection with antifungal resistance characteristics. The report has been written in line with SCARE 2020 guidelines [6].
1.1. Patient information
A 50-year-old male presented with hemoptysis, dyspnea, cough, fever, and rigor for a duration of 4 months. Three weeks before this complaint, he had cured of COVID-19 with 30% of chest involvement on computed tomography scan (CT-scan). He was diagnosed as a case of diabetes mellitus before 4 years and controlled by 800 mg metformin twice a day.
1.1.1. Clinical findings
The patient was pale and cachexic with normal vital signs and decrease air entry on the left upper zone.
1.1.2. Diagnostic assessment
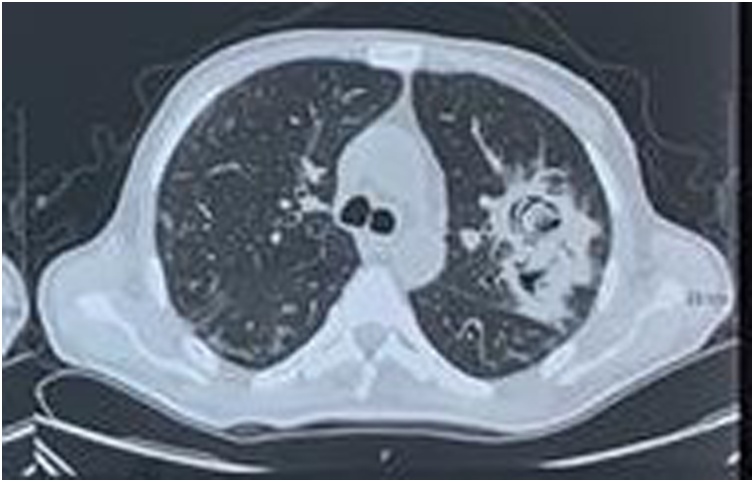
Complete blood count showed anemia (Hemoglobin 9.1 g/dl) and high white blood cells (16 × 106 cells/cm2). Chest X-Ray showed multiple ill-defined lesions involving the left upper zone. CT scan confirmed multiple cavitary lesions (Fig. 1). Flexible bronchoscopy findings were normal. The patient’s laboratory diagnosis indicated elevated WBC. Bronchoalveolar lavage (BAL) revealed pulmonary aspergillosis.
Fig. 1.
Axial CT scan shows multiple cavitary lesions involving the left upper lobe.
1.1.3. Therapeutic intervention
The patient was administered broad spectrum antifungal and antibiotics without clinical response. Due to patient deterioration and decreasing oxygen saturation (SPO2: 89), the patient was prepared for general anesthesia, in the right lateral position, through the posterolateral incision, left upper lobectomy was done. Macroscopic inspection of the specimen showed black greasy necrotic material characteristics of Aspergillus ball (Fig. 2). Direct tissue inoculation onto the blood agar showed heavy cotton colonies with aerial hyphae (Fig. 3).
Fig. 2.
Specimen showing Aspergillus ball.
Fig. 3.
Twenty-two hours after direct tissue inoculation onto the sheep blood agar showing heavy cotton colonies with aerial hyphae on agar surface and mold covering tissue piece on the plate consistent with Aspergillus species.
Macroscopic colonial characteristic was very consistent with Aspergillus spp.
1.1.4. Follow-up and outcomes
The post-operative period was uneventful. The patient stayed in the hospital for two days.
2. Discussion
Even though SARS-CoV-2 is primarily responsible for severe pneumonia and ARDS, COVID-19 is associated with a wide variety of extrapulmonary complications; hence it can be considered as a systemic disease [7]. A small portion of COVID-19 patients have fungal or bacterial co-infections, which are reportedly less than that of previous influenza pandemic [8]. A study by Intra et al. showed that Amongst COVID-19 patients, those who were admitted to the Intense Care Unit (ICU) had a higher probability (57% of ICU cases) of acquiring a fungal or bacterial secondary infection, which was higher than an earlier study (only 14%) [8,9]. The patient in the current presentation was a non-severe covid-19 case who was not hospitalized.
One of the common fungal infections that can cause secondary pulmonary infection in severely immunocompromised patients is aspergillosis, which is caused by Aspergillus fumigatus [10]. While previous studies failed to recognize influenza and COVID-19 viral infections as risk factors for aspergillosis, newly published studies report an occurrence of aspergillosis in 20–30% of the severely ill or ventilated COVID-19 patients, hence addressing an association between COVID-19 and pulmonary fungal infections, which is referred to as COVID-19 Associated Pulmonary aspergillosis (CAPA) [11].
All studies of COVID-19 fungal infections reported occurrence during the COVID-19 infection, mostly 14 days after the appearance of COVID-19 symptoms [12]. The case in the current study was a 50-year-old patient, who was previously diagnosed with COVID-19 for a period of 4 months; after a few days from his recovery, the patient developed dyspnea, cough, fever, and rigor again.
Diagnosis of CAPA is challenging due to harmless inhabitation of the airways by Aspergillus when immunity is impaired they can spread and cause pulmonary parenchymal injuries. Patients with pulmonary aspergillosis show more frequent positive serum Aspergillus Galactomannan Enzyme Immunoassay (GM EIA) results when the fungal infection is invasive beyond the airways into the blood [13,14]. In cases of CAPA, serum GM EIA is usually negative, which limits the reliability of serum-based diagnosis of CAPA [12].
There are variations from early airway inflammation to airway necrosis and cavitary lesions, revealed by imaging [12]. In the current study, the patient had elevated WBC in his laboratory diagnosis and was initially diagnosed with a chest X-Ray that revealed multiple cavitary lesions of the left upper zone, he was then suggested to do a CT scan, which also confirmed the presence of numerous cavitary lesions.
In COVID-19 patients, direct sampling of the infection site though Bronchoalveolar Lavage (BAL) is not usually considered by clinicians due to the risk of increasing COVID-19 transmission, despite having a high specificity [15]. For further examination of the current case, bronchoscopy was performed, and the result was normal; hence BAL examination revealed pulmonary aspergillosis.
According to recent studies, CAPA's risk factors are similar or the same as the risk factors of severe COVID-19 infection, such as; diabetes, use of immunosuppressive drugs [16]. In the study by Bartoletti et al. COVID-19 patients with previous exposure to anti-interleukin-6 treatment and corticosteroids were reported as risk factors of CAPA [17]. While others reported CAPA even without any prior corticosteroid treatment [18]. It has also been reported that CAPA is significantly associated with intubated COVID-19 patients [19,20]. The patient in the current case had a medical history of diabetes mellitus and was on Metformin medication. He was a non-smoker and without any recent history of corticosteroid medication.
The management of CAPA can be quite challenging and controversial, as some studies reported antifungal resistance characteristics, limiting possible treatment options [15]. At the same time, others suggested the early use of antifungal drugs, which may improve clinical outcome [12,21]. In the current case, the patient was administered different antifungal drugs (Azole family) without achieving any clinical response, which indicated multi-drug resistance characteristics of the Aspergillus. As a last resort, lobectomy was performed to remove the infected lobe.
CAPA is usually associated with severe COVID-19 cases admitted to the ICU with very similar symptoms that prevent proper early diagnosis; hence it is generally associated with the poor outcome with mortality rates of above 40% [15]. In a study by Koehler et al. 3 out of 5 of their cases died [19]. In a study by Kieren 3 out of 20 of their cases died even after antifungal treatment [12]. In the current case, the patient left the hospital in good health two days after his lobectomy operation, and no concern has been raised from later follow up.
In conclusion, pulmonary aspergillosis is a serious complication of COVID-19 patients that may not respond well to medical therapy. Pulmonary resection is the last and effective strategy to control the disease.
Declaration of Competing Interest
The authors report no declarations of interest.
Sources of funding
No source to be stated.
Ethical approval
Approval is not necessary for case report in our locality.
Consent
Consent has been taken from the patient and the family of the patient.
Author’s contribution
Fahmi H. Kakamad: Surgeon performing the operation, follow up the patient, writing the manuscript and final approval of the manuscript.
Safeen O. Mahmood: microbiologist examining the specimen and confirming the diagnosis, major contribution to the idea. Revising the manuscript.
Hawbash M. Rahim, Berwn A. Abdulla, Hiwa O. Abdullah: preparing the manuscript and final approval of the manuscript.
Snur Othman, Shvan H. Mohammed, Suhaib H. Kakamad, Shevan M. Mustafa, Abdulwahid M. Salih: major contribution to the idea, revision and final revision of the manuscript.
Registration of research studies
Not applicable.
Guarantor
Fahmi Hussein Kakamad is the Guarantor of submission.
Provenance and peer review
Not commissioned, externally peer-reviewed.
References
- 1.Abdullah H.M., Hama-Ali H.H., Ahmed S.N., Ali K.M., Karadakhy K.A., Mahmood S.O. Severe refractory COVID-19 patients responding to convalescent plasma; a case series. Ann. Med. Surg. 2020;56:125–127. doi: 10.1016/j.amsu.2020.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Baram A., Kakamad F.H., Abdullah H.M., Mohammed-Saeed D.H., Hussein D.A., Mohammed S.H. Large vessel thrombosis in patient with COVID-19, a case series. Ann. Med. Surg. 2020;60:526–530. doi: 10.1016/j.amsu.2020.11.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chen X., Liao B., Cheng L., Peng X., Xu X., Li Y. The microbial co-infection in COVID-19. Appl. Microbiol. Biotechnol. 2020;104(15):1–9. doi: 10.1007/s00253-020-10814-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Garcia-Vidal C., Sanjuan G., Moreno-García E., Puerta-Alcalde P., Garcia-Pouton N., Chumbita M. Incidence of co-infections and superinfections in hospitalized patients with COVID-19: a retrospective cohort study. Clin. Microbiol. Infect. 2021;27(1):83–88. doi: 10.1016/j.cmi.2020.07.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rawson T.M., Wilson R.C., Holmes A. Understanding the role of bacterial and fungal infection in COVID-19. Clin. Microbiol. Infect. 2021;27(1):9–11. doi: 10.1016/j.cmi.2020.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Agha R.A., Franchi T., Sohrabi C., Mathew G., for the SCARE Group The SCARE 2020 guideline: updating consensus Surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;(84):226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 7.Zheng K.I., Feng G., Liu W.Y., Targher G., Byrne C.D., Zheng M.H. Extrapulmonary complications of COVID-19: a multisystem disease? J. Med. Virol. 2021;93(1):323–335. doi: 10.1002/jmv.26294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lansbury L., Lim B., Baskaran V., Lim W.S. Co-infections in people with COVID-19: a systematic review and meta-analysis. J. Infect. 2020;81(2):266–275. doi: 10.1016/j.jinf.2020.05.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Intra J., Sarto C., Beck E., Tiberti N., Leoni V., Brambilla P. Bacterial and fungal colonization of the respiratory tract in COVID-19 patients should not be neglected. Am. J. Infect. Control. 2020;48(9):1130–1131. doi: 10.1016/j.ajic.2020.06.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Silva L.N., de Mello T.P., de Souza Ramos L., Branquinha M.H., Roudbary M., Dos Santos A.L. Fungal infections in COVID-19-positive patients: a lack of optimal treatment options. Curr. Top. Med. Chem. 2020;20(22):1951–1957. doi: 10.2174/156802662022200917110102. [DOI] [PubMed] [Google Scholar]
- 11.Fekkar A., Lampros A., Mayaux J., Poignon C., Demeret S., Constantin J.M. Occurrence of invasive pulmonary fungal infections in severe COVID-19 patients admitted to the ICU. Am. J. Respir. Crit. Care Med. 2020;203(3):307–317. doi: 10.1164/rccm.202009-3400OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Marr K.A., Platt A., Tornheim J.A., Zhang S.X., Datta K., Cardozo C. Aspergillosis complicating severe coronavirus disease. Emerging Infect. Dis. 2021;27(1):18. doi: 10.3201/eid2701.202896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Van de Groep K., Verboom D.M., Van de Veerdonk F.L., Haas P.J., Van der Poll T., Schultz M.J. Detection of invasive aspergillosis in critically ill patients with influenza: the role of plasma galactomannan. Am. J. Respir. Crit. Care Med. 2019;200(5):636–638. doi: 10.1164/rccm.201903-0587LE. [DOI] [PubMed] [Google Scholar]
- 14.Bassetti M., Giacobbe D.R., Grecchi C., Rebuffi C., Zuccaro V., Scudeller L. Performance of existing definitions and tests for the diagnosis of invasive aspergillosis in critically ill, adult patients: a systematic review with qualitative evidence synthesis. J. Infect. 2020;81(1):131–141. doi: 10.1016/j.jinf.2020.03.065. [DOI] [PubMed] [Google Scholar]
- 15.Hoenigl M. Invasive fungal disease complicating COVID-19: when it rains it pours. Clin. Infect. Dis. 2020 doi: 10.1093/cid/ciaa1342. (In Press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nasir N., Farooqi J., Mahmood S.F., Jabeen K. COVID‐19‐associated pulmonary aspergillosis (CAPA) in patients admitted with severe COVID‐19 pneumonia: an observational study from Pakistan. Mycoses. 2020;63(8):766–770. doi: 10.1111/myc.13135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bartoletti M., Pascale R., Cricca M., Rinaldi M., Maccaro A., Bussini L. Epidemiology of invasive pulmonary aspergillosis among COVID-19 intubated patients: a prospective study. Clin. Infect. Dis. 2020;1(1) doi: 10.1093/cid/ciaa1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rutsaert L., Steinfort N., Van Hunsel T., Bomans P., Naesens R., Mertes H. COVID-19-associated invasive pulmonary aspergillosis. Ann. Intensive Care. 2020;10(1):1–4. doi: 10.1186/s13613-020-00686-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Koehler P., Cornely O.A., Böttiger B.W., Dusse F., Eichenauer D.A., Fuchs F. COVID‐19 associated pulmonary aspergillosis. Mycoses. 2020;63(6):528–534. doi: 10.1111/myc.13096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Van Arkel A.L., Rijpstra T.A., Belderbos H.N., Van Wijngaarden P., Verweij P.E., Bentvelsen R.G. COVID-19–associated pulmonary aspergillosis. Am. J. Respir. Crit. Care Med. 2020;202(1):132–135. doi: 10.1164/rccm.202004-1038LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Talento A.F., Hoenigl M. Fungal infections complicating COVID-19: with the rain comes the spores. J. Fungi. 2020;6(4):279. doi: 10.3390/jof6040279. [DOI] [PMC free article] [PubMed] [Google Scholar]