Fig. 1 |. Neuroimmune interfaces and postulated mechanisms by which they can be breached.
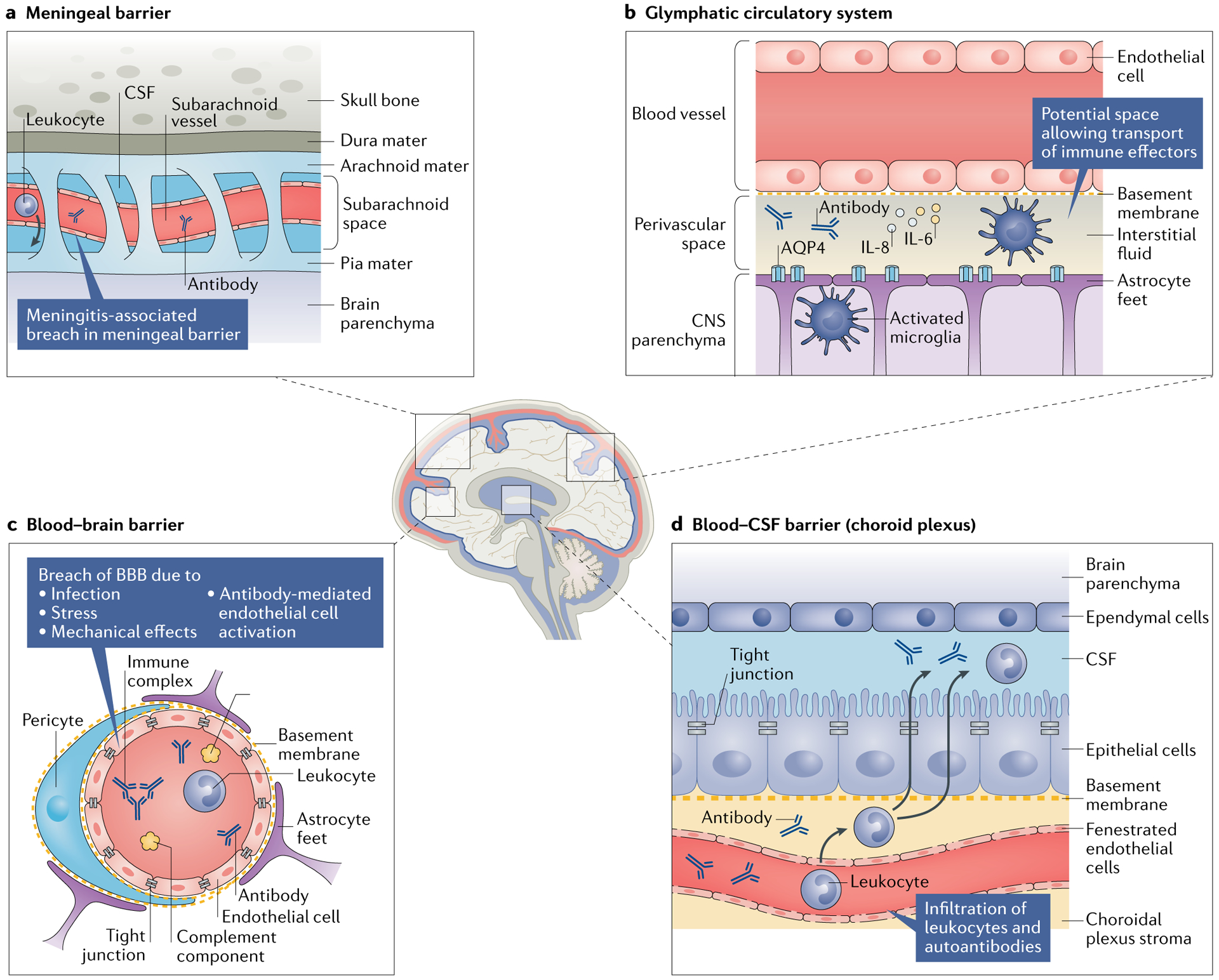
Damage to the blood–brain barrier (BBB) might enable neuropathic antibodies in the serum of patients with systemic lupus erythematosus to enter the central nervous system (CNS); however, several other interfaces could also serve as sites of leukocyte and pathogenic antibody transfer into the CNS. a | The arachnoid epithelium serves as the meningeal barrier between the cerebrospinal fluid (CSF) in the subarachnoid space and the blood in cerebral veins. Meningitis (both aseptic and infectious) can cause inflammation in the subarachnoid space, potentially leading to a breach of this barrier that enables circulating pathogenic antibodies, leukocytes and pro-inflammatory cytokines to enter into the CSF. b | The glymphatic pathway is a perivascular pseudolymphatic system that provides a conduit for interstitial fluid in the brain parenchyma. Brain antigens (such as microtubule-associated protein 2) might be recognized by indwelling antigen-presenting cells in the perivascular space, which can migrate to the cervical lymph nodes and initiate an adaptive response. c | Breach of the BBB has been observed under several circumstances, including infection (simulated by lipopolysaccharide administration), stress (simulated by adrenaline infusion), the mechanical and inflammatory sequelae of vascular occlusion and antibody-mediated endothelial cell activation. d | The fenestrated capillary plexus within the choroid plexus enables ready access of antibodies and leukocytes to the choroidal plexus stroma (a previously characterized site of immunosurveillance) and potentially into the CSF. AQP4, aquaporin 4.
