Fig. 2 |. Pathogenetic mechanisms and potential treatment targets in diffuse NPSLE.
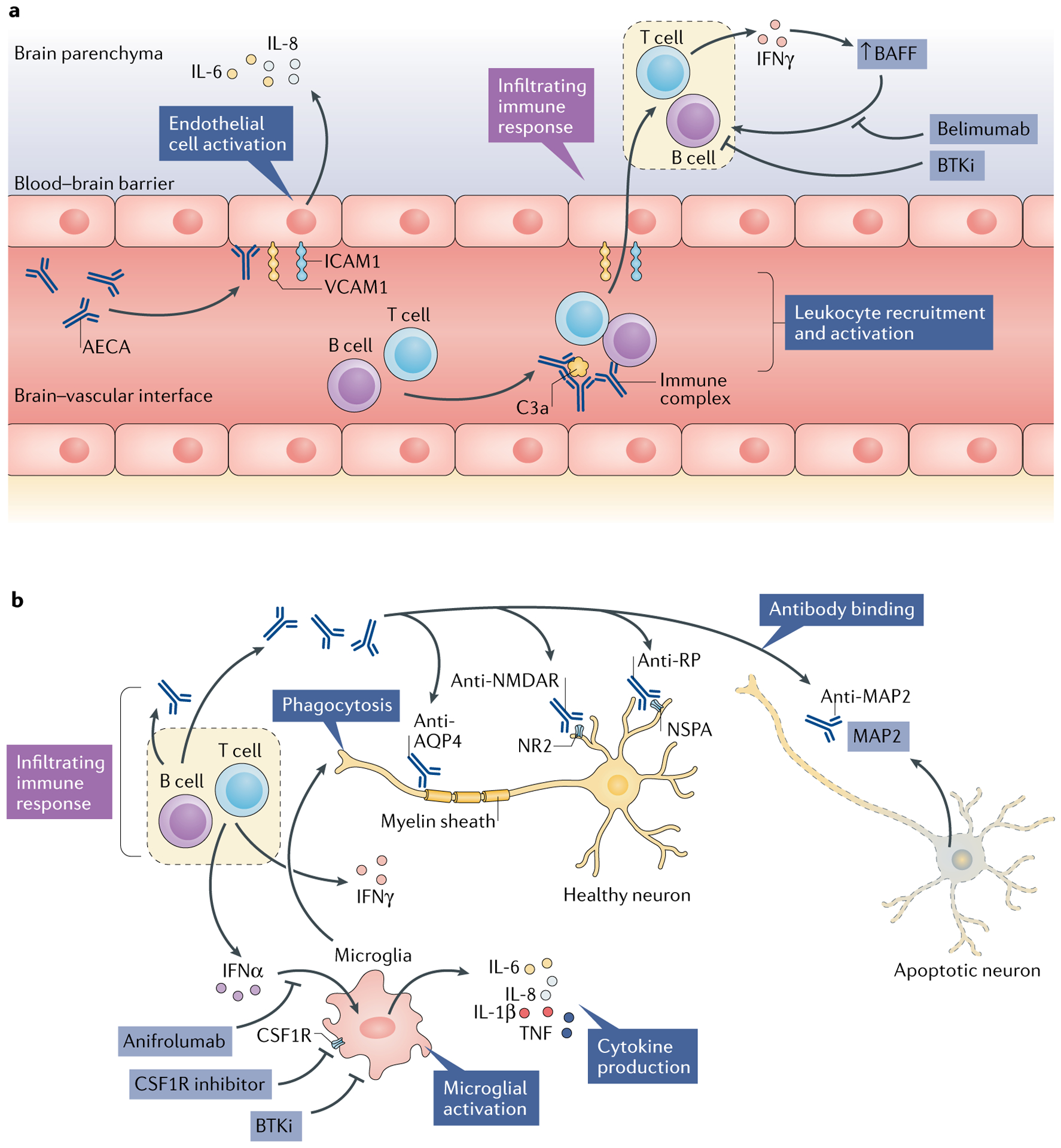
Several different but potentially complementary pathways and effectors in the central nervous system (CNS) microenvironment might be involved in the pathogenesis of neuropsychiatric systemic lupus erythematosus (NPSLE). a | Endothelial cells connected by tight junctions comprise the blood–brain barrier and are subject to activation by autoantibodies such as anti-endothelial cell antibodies (AECAs). Activated endothelial cells show upregulated expression of adhesion molecules (such as intercellular adhesion molecule 1 (ICAM1) and vascular cell adhesion molecule 1 (VCAM1)), which facilitate leukocyte infiltration into the CNS parenchyma. In addition, these activated endothelial cells secrete pro-inflammatory cytokines, including IL-6 and IL-8. Concurrently, immune complexes in the cerebral vasculature activate the complement system, which further promotes chemotaxis. The locally infiltrating leukocytes secrete pro-inflammatory cytokines, such as IFNγ, which in turn promotes B cell survival and activation via increasing local levels of B cell activating factor (BAFF). b | Microglia are consequently activated, most notably by interferons, the elevated intrathecal levels of which are commonly seen in patients with NPSLE. Activated microglia further propagate local cytokine and chemokine signalling cascades, in addition to direct phagocytic activity focused on neuronal surface signalling domains and synaptic termini. Finally, several neuropathic autoantibodies have been implicated in NPSLE, including antibodies to the NR2 subunit of the anti-N-methyl-d-aspartate receptor (NMDAR), anti-ribosomal P protein (RP; targeting neuronal surface P antigen (NSPA)) and anti-microtubule-associated protein 2 (MAP2) antibodies, which might have direct neurotoxic effects and provide a source of intrathecal immune complexes. Anti-aquaporin 4 (AQP4) antibodies, directed against the myelin sheath, are found in some patients with SLE who have demyelinating disease. The above pathogenetic mechanisms, along with studies in animal models, suggest that several drugs might prove to be effective in treating NPSLE, including belimumab (a BAFF inhibitor), anifrolumab (a type I interferon receptor antagonist), macrophage colony-stimulating factor-1 receptor (CSF1R) inhibitors (which block activation of microglia and infiltrating macrophages) and tyrosine-protein kinase BTK (also known as Bruton tyrosine kinase) inhibitors (BTKis), which interrupt inflammatory activation of B cells and macrophages or microglia.
