Highlights
-
•
Esophageal perforation is an uncommon complication may occur during bariatric surgery.
-
•
The early diagnosis and the optimal therapeutic approach may reduce the mortality rate.
-
•
The bougie transoral insertion should be done by an anesthesiologist to prevent unwanted complications such as perforation.
Keywords: Esophageal perforation, Laparoscopic sleeve gastrectomy, Subcutaneous emphysema
Abstract
Introduction and importance
Esophageal perforation (EF) is an uncommon complication of bariatric procedures, mostly related to the intraoperative use of bougie that is used for gastric calibration.
Case presentation
Here, we present a 33-year-old woman who underwent laparoscopy sleeve surgery (LSG). Due to perforation in the cervical site of the esophagus caused by bougie insertion, she developed subcutaneous emphysema on the first post-operative day. She immediately underwent reconstructive esophageal surgery under the probable diagnosis of having a cervical esophagus perforation. The patient’s condition was stable in the postoperative period and discharged after 10 days.
Clinical discussion
The patients who present symptoms including subcutaneous emphysema, cervical pain, dysphagia, dysphonia, and fever post-surgery have to be considered for probably EF. The early optimal diagnosis works up and therapeutic approach should be performed as soon as possible to prevent mortality.
Conclusion
EP caused by a bougie insertion is an uncommon complication that is associated with high mortality rates if the diagnosis and treatment were delayed. The risk of using a bougie during surgery should not be underestimated and have to be inserted with extreme caution and careful guide of surgeon.
1. Introduction
Esophageal perforation (EP) is a well-defined and critical clinical status. The mortality rate associated with esophageal perforation is high due to the complexity of locating the esophagus, lack a potent serosa, remarkable blood flow in the organ, and closeness of the esophagus to vital organs [1,2]. The early diagnosis and the optimal therapeutic approach reduce the mortality rate [3]. EP seems to be very rare in bariatric surgery since the operation does not directly affect the esophagus [4]. Laparoscopic sleeve gastrectomy (LSG) is a restrictive bariatric procedure for treating obesity disorder by removing some parts of the stomach. Even though LSG is relatively safe for losing weight, esophageal perforation following the use of bougie that is an uncommon complication may occur during surgery. To our knowledge, esophageal perforation after LSG has only been reported twice [5,6]. Here, we present a case report describing a patient with a cervical esophageal perforation, which occurred during LSG. This case report has been reported in line with the SCARE criteria [7].
2. Case presentation
This is a report about a 33-year-old woman, with morbid obesity (BMI: 41.5) who underwent laparoscopic sleeve gastrectomy (LSG) in Mother and Child Hospital in Shiraz, a center of excellence of bariatric surgery by an experienced bariatric surgery team. Patients past medical history was unremarkable, except for seasonal allergy which she had been using antihistamine medication for alleviation of her symptoms. There were no relevant past medical, previous surgeries, family history or psychosocial history. Pre-operational work-ups including abdominal pelvic sonography, endoscopy, routine blood tests, ECG, bone densitometry (dual-energy X-ray absorptiometry imaging) was conducted with no major variations from normal levels.
Sleeve gastrectomy was performed successfully on bougie 36 Fr from 4 cm above pylorus with six 60 mm EndoGIA stapler cartridges up to cardia in the evening and there were no intraoperative complications. She was transferred to the ward under acceptable medical conditions. During the night she developed mild edema on her right side of her head and neck. Her vital signs were checked regularly and were normal. With an impression of angioedema, steroid and anti-histamine medication were prescribed.
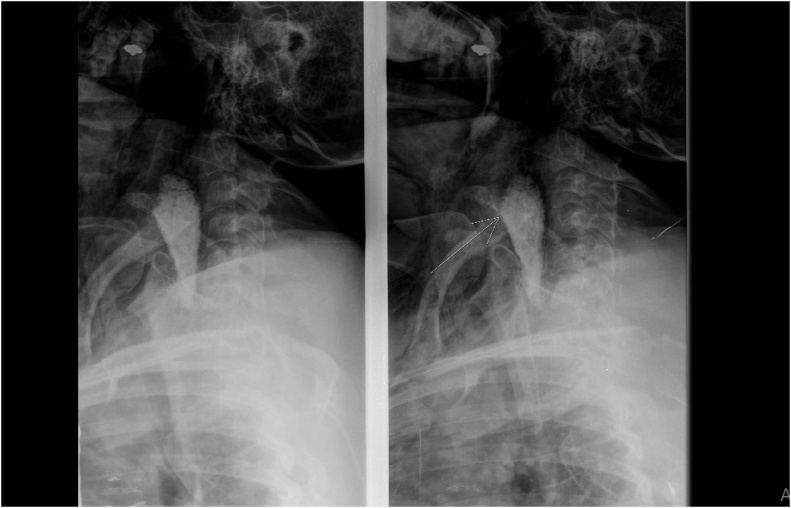
The next morning, the patient developed respiratory distress and subcutaneous emphysema on her right side of her head and neck. A lateral neck x-ray and a contrast study were performed, which showed contrast extravasation in the cervical esophagus (Fig. 1). The patient immediately underwent surgery under the probable diagnosis of having a cervical esophagus perforation.
Fig. 1.
Barium swallow showed contrast extravasation from site of perforation.
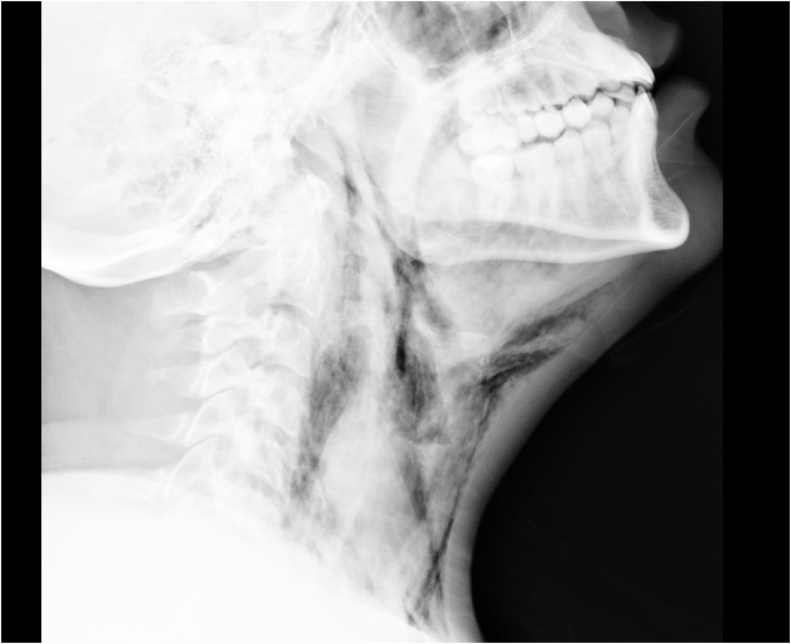
With neck in extended position via classic left side neck incision, a 0.5 × 1 cm long perforation located on the left side of the posterior wall of the cervical esophagus was found (Fig. 2). Due to the clean wound on the defect, simple closure of the perforation was done by interrupted sutures (with PDS 3/0). After placing drains in the thoracic cavity, the jejunostomy feeding tube was located about 30 cm after ligament of Treitz by laparoscopy procedure, and operation was terminated. The patient transferred to the ward and was hospitalized for 10 days. The patient’s hemodynamic status was stable in the postoperative period. On post-operative day 7, after further barium swallow performance, oral feeding started and the jejunostomy tube was removed. The patient was discharged 48 h hours later when she tolerated advanced oral feeding with prescription of oral antibiotic and anti-acid medication. The patient was visited 10 days after the hospital discharge in an out-patient clinic and she was in a favorable health condition. Moreover, no complications were detected in 3 months postoperative period and she tolerated the post-bariatric food intake as well as other bariatric patients. The patient was satisfied with the course of recovery after the surgery.
Fig. 2.
Cervical emphysema post esophageal perforation.
3. Discussion
Esophageal perforation is a possible but uncommon complication of bariatric procedures, mostly related to the intraoperative use of esophageal tubes [6]. In the LSG usually a bougie size 36 Fr is used and placed into the stomach. The gastrectomy is performed over this tube, a maneuver that calibrates the width of the remaining stomach during the resection [8]. Despite bougie-induced esophageal perforation during surgery is uncommon; in our case, a bougie with a diameter of 35Fr caused the perforation on the posterior wall of the cervical esophagus. The standard technique is that the anesthesiology team should do a transoral bougie insertion to prevent unwanted complications such as perforation [9].
The clinical presentation differs according to the perforation’s location. Perforation of the cervical esophagus presents commonly with subcutaneous emphysema (95%), cervical pain (90%), dysphagia, dysphonia, and fever [2]. Cervical esophageal perforations tend to incite less systemic inflammatory response than thoracic and abdominal perforations, due to the containment of the contents within the facial planes of the neck. Perforations occurring in this area are not as well contained, eliciting local and systemic inflammatory responses [10]. The diagnostic workup includes CT scan and plain cervical or chest X-ray films, which can reveal pleural effusion, pneumo- or hydropneumothorax, pneumomediastinum, subcutaneous emphysema and/or pneumoperitoneum. 90% of chest X-rays are abnormal in EP [10].
Upper gastrointestinal swallow study with water soluble contrast is also used to lesser extent compared to CT scan because of its lower sensitivity, which is around 50% for the detection of cervical perforations and 75–80% for thoracic perforations [11]. Although the CT scan is more sensitive in diagnosis of EP than other imaging studies, in this case, the cervical EP was confirmed by contrast study, therefore, no other imaging studies were done.
The fundamental principles in the management of EP are aggressive drainage and debridement of the mediastinum, diversion of the esophagus and the leak site, and an enterostomy for enteral feedings [3]. The outcome of surgical treatments is affected by the size and location of the perforation, degree of local tissue necrosis, and time elapsed since the perforation occurred. Lesions treated within the first 24 h have substantially better results than those treated after the 1 st day with a 7.4% and 20.3% mortality rate, respectively [12]. Vague symptoms and physician inexperience may delay diagnosis and subsequent therapy, further increasing the mortality risk [13]. Tiller et al. reported that early recognition of esophageal perforation after insertion of an NGT is the best prognostic indicator of outcome [14]. Similar to our case, studies by both Lovece and Theodorou revealed bougie-induced perforations in the upper and lower esophagus in the bariatric procedures. Lovece et al. described a 42-year old female patient who underwent LSG with a cervical EP, treated with an emergency thoracoscopy and evacuation of a mediastinal fluid collection, with additional neck incision for primary closure of the esophageal defect which was reinforced with a sternocleidomastoid muscle flap, and discharged 7 days later [5]. In Theodorou study, a 56-year-old woman who underwent LSG and a 41-year-old woman who underwent laparoscopic adjustable gastric banding presented with lower and middle EP, respectively. Despite the late identification of the first patient, she was treated successfully with a reconstructive operation. Unlike the first patient, the second patient with rapid identification and treatment of the EP did not recover from the septic shock and eventually expired from multi-organ failure [6].
In the presented case, a patient underwent LSG for treatment of her morbid obesity complicated by EP occurring during bougie insertion. The cervical EP is usually symptomatic by subcutaneous emphysema that should be identified as soon as possible, because of dangerous complications in later diagnosis. Therefore, we recommend that the surgeon must guide and pay attention in the momento of insertion of the bougie to prevent of this complication and carefully evaluate the patient’s symptoms post-operatively.
4. Conclusion
EP is an uncommon complication with high mortality rate. The risk of using a bougie during surgery should not be underestimated and an anesthesiologist must insert the bougie with extreme caution and careful guide of surgeon. The patients should be observed for the symptoms, especially in the first 24 h post-surgery. The available diagnostic tests should be done without delay. The early diagnosis seems to be the key to success. A surgical approach is a gold standard when the defect is large.
Conflict of interest
The authors have nothing to disclose.
Source of funding
This research did not receive any specific grant from funding agencies.
Ethical approval
The study is exempt from ethical approval.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author contribution
Writing the paper, Study Concept : Neda Haghighat, Seyed Mohammad Kazem Tadayon.
Data collection, Study Concept: Nader Moeinvaziri, Maryam Sotoodeh.
Supervision: Seyed Mohammad Kazem Tadayon, Masoud Amini.
Registration of research studies
N/A.
Guarantor
Seyed Mohammad Kazem Tadayon is the guarantor of submission and accepts full responsibility.
Provenance and peer review
Not commissioned, externally peer-reviewed.
References
- 1.Skinner D.B., Little A.G., De Meester T.R. Management of esophageal perforation. Am. J. Surg. 1980;139:760–764. doi: 10.1016/0002-9610(80)90379-7. [DOI] [PubMed] [Google Scholar]
- 2.Ryom P., Ravn J.B., Penninga L. Aetiology, treatment and mortality af¬ter oesophageal perforation in Denmark. Dan. Med. Bull. 2011;58:A4267. [PubMed] [Google Scholar]
- 3.Vallböhmer D., Hölscher A.H., Hölscher M., Bludau M., Gutschow C., Stippel D. Options in the management of esophageal perforation: analysis over a 12-year period. Dis. Esophagus. 2010;23:185–190. doi: 10.1111/j.1442-2050.2009.01017.x. [DOI] [PubMed] [Google Scholar]
- 4.Signorini F.J., Gorodner V., Marani M., Viscido G., Moser F. Iatrogenic injury of the intrathoracic oesophagus with bougie during sleeve gastrectomy. J. Minim. Access Surg. 2018;14(1):79–82. doi: 10.4103/jmas.JMAS_21_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lovece A., Rouvelas I., Hayami M., Lindblad M., Tsekrekos A. Cervical esophageal perforation caused by the use of bougie during laparoscopic sleeve gastrectomy: a case report and review of the literature. BMC Surg. 2020;20(January (1)):9. doi: 10.1186/s12893-020-0679-1. PMID: 31924187; PMCID: PMC6954567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Theodorou D., Doulami G., Larentzakis A., Almpanopoulos K., Stamou K., Zografos G., Menenakos E. Bougie insertion: a common practice with underestimated dangers. Int. J. Surg. Case Rep. 2012;3:74–77. doi: 10.1016/j.ijscr.2011.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Agha R.A., Franchi T., Sohrabi C., Mathew G., for the SCARE Group, The SCARE Guideline: updating consensus surgical CAse REport (SCARE) guidelines. Int. J. Surg. 2020;2020(84):226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 8.Rosenthal R.J., International Sleeve Gastrectomy Expert Panel, Diaz A.A., Arvidsson D., Baker R.S., Basso N., Bellanger D., Boza C., El Mourad H., France M., Gagner M., Galvao-Neto M., Higa K.D., Himpens J., Hutchinson C.M., Jacobs M., Jorgensen J.O., Jossart G., Lakdawala M., Nguyen N.T., Nocca D., Prager G., Pomp A., Ramos A.C., Rosenthal R.J., Shah S., Vix M., Wittgrove A., Zundel N. International Sleeve Gastrectomy Expert Panel Consensus Statement: best practice guidelines based on experience of&12,000 cases. Surg. Obes. Relat. Dis. 2012;8(1):8–19. doi: 10.1016/j.soard.2011.10.019. [DOI] [PubMed] [Google Scholar]
- 9.LowhamAS Filipi C.J., Hinder R.A. Mechanisms and avoidance of esophageal perforation by anesthesia personnel during laparoscopic foregut surgery. Surg. Endosc. 1996;10(10):979–982. doi: 10.1007/s004649900218. [DOI] [PubMed] [Google Scholar]
- 10.Chirica M., Champault A., Dray X., Sulpice L., Munoz-Bongrand N., Sarfati E. Esophageal perforations. J. Visc. Surg. 2010;147(3):117–128. doi: 10.1016/j.jviscsurg.2010.08.003. [DOI] [PubMed] [Google Scholar]
- 11.Chirica M., Champault A., Dray X., Sulpice L., Munoz-Bongrand N., Sarfati E. Esophageal perforations. J. Visc. Surg. 2010;147(3):117–128. doi: 10.1016/j.jviscsurg.2010.08.003. [DOI] [PubMed] [Google Scholar]
- 12.Horvath P., Lange J., Stüker D., Wichmann D., Hilbert J., Götz M., Königsrainer A., von Feilitzsch M., Zdichavsky M. Multimodal treatment strategies for esophageal perforation. Surg. Laparosc. Endosc. Percutan. Tech. 2018;28(4):232–238. doi: 10.1097/SLE.0000000000000549. [DOI] [PubMed] [Google Scholar]
- 13.Onat S., Ulku R., Cigdem K.M. Factors affecting the outcome of surgically treated non-iatrogenic traumatic cervical esophageal perforation: 28 years experience at a single center. J. Cardiothorac. Surg. 2010;5 doi: 10.1186/1749-8090-5-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tiller H.J., Rhea W.G., Jr Iatrogenic perforation of the esophagus by a nasogastric tube. Am. J. Surg. 1984;147:423–425. doi: 10.1016/0002-9610(84)90182-x. [DOI] [PubMed] [Google Scholar]