Abstract
Objective:
In early 2020, the spread of coronavirus disease-2019 (COVID-19) led the World Health Organization to declare this disease a pandemic. Initial epidemiological data showed that patients with cancer were at high risk of developing severe forms of COVID-19. National scientific societies published recommendations modifying the patients’ breast cancer (BC) management to preserve, in theory, quality oncologic care, avoiding the increased risk of contamination. The Senology International Society (SIS) decided to take an inventory of the actions taken worldwide. This study investigates COVID-19-related changes concerning BC management and analyzes the will to maintain them after the pandemic, evaluating their oncological safety consequences.
Materials and Methods:
SIS network members participated in an online survey using a questionnaire (Microsoft® Forms) from June 15th to July 31st, 2020.
Results:
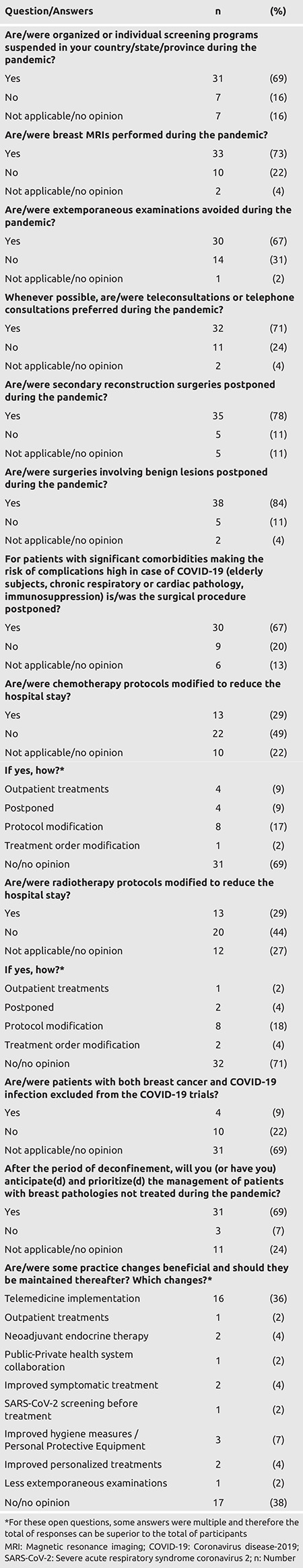
Forty-five responses from 24 countries showed that screening programs had been suspended (68%); magnetic resonance imagines were postponed (73%); telemedicine was preferred when possible (71%). Surgeries were postponed: reconstructive (77%), for benign diseases (84%), and in patients with significant comorbidities (66%). Chemotherapy and radiotherapy protocols had been adapted in 28% of patients in both. Exception for telemedicine (34%), these changes in practice should not be continued.
Conclusion:
The SIS survey showed significant changes in BC’s diagnosis and treatment during the first wave of the COVID-19 pandemic, but most of these changes should not be maintained. Indeed, women have fewer severe forms of COVID-19 and are less likely to die than men. The risk of dying from COVID-19 is more related to the presence of comorbidities and age than to BC. Stopping screening and delaying treatment leads to more advanced stages of BC. Only women aged over 65 with BC under treatment and comorbidities require adaptation of their cancer management.
Keywords: Breast cancer, COVID-19, SARS-CoV-2, clinical practices, survey, pandemic
Introduction
At the end of 2019, a new coronavirus (SARS-CoV-2) caused pneumonia in several patients epidemiologically linked to a Wuhan market (Hubei province, China). In early 2020, the spread of coronavirus disease-2019 (COVID-19) led the World Health Organization to declare this disease a pandemic. Despite extraordinary measures implemented in many countries, the epidemic spread, with mortality significantly higher than influenza. Initial epidemiological data showed that patients who were older and/or had comorbidities, and notably cancer, were at higher risk of developing severe forms of COVID-19 (1, 2). As breast cancer (BC) is the leading cancer among women worldwide, with more than 2 million new cases and more than 650,000 deaths each year (3), the situation was of particular concern for women with BC. Emergency health actions have been implemented in various countries, involving changes in the treatment and care circuits for numerous cancers, including BC. Many national scientific societies published a series of recommendations modifying BC patient management to preserve, in theory, quality oncologic care while avoiding an increased risk of contamination by SARS-CoV-2 (4, 5, 6). In addition, postponing BC surgeries freed equipment and health care staff to support COVID-19 patient care.
The Senologic International Society (SIS) has always been dedicated to promoting breast health and improving BC patients’ care, considering medical, social, economic, and ethical constraints. In this pandemic context, the SIS, by its active members, experts, and its global network, decided to assess the actions taken worldwide, the clinical practice changes, and the particularities observed in different countries regarding BC management. The SIS survey’s first objective was to investigate and share COVID-19-related changes in clinical practices concerning BC management since the beginning of the pandemic. The second objective was to analyze the will to maintain these changes later in treatment modalities and care pathways, considering the consequences of these oncological safety changes.
Materials and Methods
SIS network members were invited to participate in an online survey using the Microsoft® Forms questionnaire. Between June 15th and July 31st, 2020, participants were invited to answer the questionnaire via e-mail. The answers were directly recorded into an online database, and only one response per participant was allowed. However, more than one response was authorized for each country in case of national disparities.
The online survey consisted of 17 questions. Question 1 was about the participant’s origin. The number of deaths due to Coronavirus recorded in his/her country at the moment of the survey, and question 17 was about the participant’s profile. Next, we questioned the participants about BC screening programs, radiological practices (question 4), pathological analyses (question 5), telemedicine (question 6), secondary reconstruction surgeries (question 7), benign lesion surgeries (question 8), surgery for patients with comorbidities (question 9), chemotherapy practices (questions 10 and 11), radiotherapy practices (question 12 and 13), and clinical trials (question 14). We then asked about the management after the lockdown period, if applicable (question 15), and the practice changes that should be maintained thereafter (question 16). The questionnaire is available as Supplementary Material S1 in Appendix 1.
Results
We received 45 completed questionnaires in total. Participants came from 24 countries on six continents (Figure 1): Algeria, Australia, Brazil, Democratic Republic of Congo, Croatia, Ecuador, Egypt, France, Germany, Ghana, Greece, Israel, Jamaican Republic, Japan, Lithuania, Nigeria, Poland, Romania, Russia, Senegal, Spain, Switzerland, Turkey, and the United States. The survey results are reported in Table 1.
Figure 1.
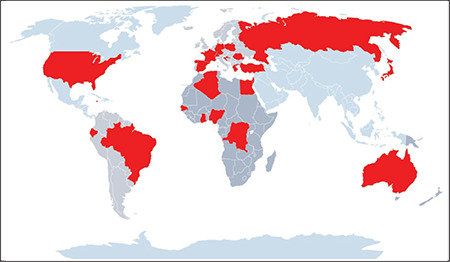
World map with countries that participated in this survey
Table 1. Survey results.
In our survey, 38% of participants were oncological surgeons, 4% medical oncologists, 4% radiotherapists, 4% radiologists, 2% nuclear physicians, and 2% anesthesiologists. The other 46% had more than one specialty (a radiologist and nuclear physician or radiotherapist and medical oncologist). Fifty-six percent of respondents had a public or governmental practice, 13% a practice in the private sector, and 31% were involved with both activities. No difference was noted between the public and private sectors regarding BC management.
Diagnosis and consultations
Most participants (69%) reported that organized or individual screening programs were suspended during the pandemic. Sixteen percent of participants reported that screening programs were maintained (Japan, Senegal, Switzerland-in one canton, Jamaican Republic, Croatia, and Algeria). No response was available in the other cases, as these countries have no screening programs.
Participants answered that breast magnetic resonance imaging (MRI) was more often maintained (73%). In contrast, it was suspended for 22% of participants (Switzerland in three cantons, France, Democratic Republic of Congo, Nigeria, Ecuador, and Turkey) due to the difficulty of adequately disinfecting the devices. No response was available in the other cases.
Concerning teleconsultations and phone consultations, most participants (71%) preferred this solution, when possible, during the pandemic. On the other hand, 24% of participants preferred classical consultations. No response was available in the other cases.
Treatment
Surgery was dramatically modified on different levels since the start of the pandemic. Participants reported that surgeries involving benign lesions were postponed in the majority of cases (84%). Similarly, secondary reconstruction surgeries were also postponed by most participants (78%). For 11% of participants, the question was not applicable since breast reconstruction was not performed in these centers. Most participants (67%) reported that extemporaneous examinations were avoided for BC surgery, whereas 31% continued with them. For one participant (2%), this question was not applicable. For fragile patients (patients with significant comorbidities at high risk of complications in the case of COVID-19), 67% of participants reported that surgeries were postponed, compared with 20% in whom they were not. This question was not applicable, or the participants had no opinion in the remaining other cases.
Other BC treatments were also impacted. Concerning chemotherapy, 29% of participants reported that protocols were modified to reduce hospital stays, whereas 49% remained unchanged. For the remaining participants, this question was not applicable, or the participant had no opinion. Participants who answered positively (n = 13) reported different methods (multiple responses were possible for each participant): protocol modifications (62%), outpatient treatments (31%), treatment postponement (31%) and/or treatment order modification (i.e., chemotherapy before radiotherapy, 8%).
Concerning radiotherapy, 29% of participants reported that protocols were modified to reduce hospital stays (hypofractionated protocols), whereas, in 44%, they were unchanged. For 27% of participants, this question was not applicable, or the participant had no opinion. Similarly, participants who answered positively (n = 13) reported different methods (multiple responses were possible for each participant): protocol modifications (62%), outpatient treatments (8%), treatment postponement (15%) and/or treatment order modification (15%).
Clinical trials
Four participants (9%) mentioned that patients with BC and COVID-19 were excluded from clinical trials concerning COVID-19. Ten participants responded negatively (22%). This question was not applicable, or the participant had no opinion in 69% of cases.
After the lockdown period
Most participants (69%) anticipated and prioritized the management of patients with breast pathologies not treated during the pandemic. We observed that 24% of participants did not respond, as, in some countries, there was no lockdown at the time of the survey.
Thirty-six percent of participants found that telemedicine implementation should be maintained after the pandemic, for example, for BC survivors. The remaining practice changes should not be maintained to avoid the pejorative evolution of some patients.
Mortality
Our survey did not provide any results regarding mortality among BC patients, as it concerned practice changes and was not an observational study.
Discussion and Conclusion
The SIS conducted an international survey to investigate and share COVID-19 related changes in clinical practices concerning BC management during the pandemic.
Strengths and limitations of the survey
Participants were from 24 countries, as shown in Figure 1. These countries represented 1.701 billion people and 22% of the world’s population. Participants had different disciplines and covered most breast specialties: surgery (general and gynecological), medical oncology, radiotherapy, radiology, nuclear medicine, and anesthesiology. In addition, they were from different types of practices, working in both university hospitals and private practices. In some cases, practices were heterogeneous among healthcare providers within each country, especially if the pandemic affected their regions differently. However, the SIS survey showed that many countries had adopted similar measures. Concerning diagnosis, screening programs had often been suspended, and MRI use was reduced. Therapeutically, non-urgent surgery had been postponed, whereas medical and radiotherapy treatments had been adopted.
All these changes were based on initial epidemiological data hypothesizing that patients with cancer were at a higher risk of developing severe forms of COVID-19. For example, at the beginning of the pandemic, a study published by Liang et al. (1) showed that patients with cancer had a higher risk of developing a severe form of COVID-19, including invasive ventilation, intensive care unit admissions, or death [odds ratio (OR): 5.34, 95% confidence interval (CI): 1.80-16.18; p = 0.0026]. However, even when the study included 1,590 patients, only 18 (1%) had a history of cancer, and among them, BC was present in only three patients. Similarly, Fu et al. (7) showed that cancer patients, in general, were at a higher risk of being infected with SARS-CoV-2 and had higher mortality rates. Likewise, de Azambuja et al. (8) showed that in a cohort of 13,594 patients (of whom 1,187 had solid cancers), cancer was associated with higher COVID-19 related mortality. However, in April 2020, Miyashita et al. (2) published a report on 5,688 patients, including 344 with cancer, of whom 57 had BC. They found that patients with cancer were at significantly higher risk of requiring invasive ventilation (relative risk: 1.89; 95% CI: 1.37–2.61) but not of death (relative risk: 1.15; 95% CI: 0.84–1.57) except for patients aged up to 50 years old (relative risk: 5.01; 95% CI: 1.55–16.2). Unfortunately, no subgroup analysis based on the cancer type was provided.
Since patients with cancer might be at a higher risk in COVID-19, several scientific societies published guidelines to adapt BC management during the pandemic. Worldwide, BC care pathways were disrupted (9, 10): screening was discontinued, surgeries were delayed, chemotherapy and radiotherapy protocols were adapted to reduce hospital stays or the number of sessions. BC treatments were modified since the beginning of the pandemic. First, chemotherapy protocols were changed to reduce hospital stays. For instance, taxane-based protocols with weekly administrations (i.e., paclitaxel) were replaced by docetaxel administrations every three weeks. Otherwise, some other protocols were discontinued or postponed. In some metastatic situations, chemotherapy regimens were changed to an oral treatment such as capecitabine. The main goal was to decrease potential exposure to SARS-CoV-2 and complications in concomitant chemotherapy and COVID-19. Similarly, an American team published results concerning medical treatment modifications in New York and found that adjuvant and neoadjuvant chemotherapy were modified in 41% of cases to reduce the risk of SARS-CoV-2 infection (11). In contrast, oral treatments were modified in only 15% of cases (11).
Radiotherapy was also changed during the pandemic. Hypofractionated regimens were preferred for BC treatment, whereas in other cases, treatment was discontinued. Spencer et al. (12) published a report on radiotherapy modifications in the United Kingdom during the pandemic and found similar results. For instance, treatment with ultra-hypofractionated regimens (26 Gy in 5 fractions) greatly increased from 0.2% in April 2019 to 60.6% in April 2020.
Finally, surgery was also impacted. As reported in the survey, benign and reconstructive surgeries were postponed. In fragile patients, cancer surgeries have also been postponed, and in some cases, neoadjuvant endocrine therapy was introduced. As reported in a survey in the United States published by Park et al. (13), most oncologists (medical, radiotherapists, and surgeons) changed their BC management, and neoadjuvant endocrine therapies went from rarely to frequently prescribed during the pandemic. In addition, most participants found it reasonable to delay surgery without the use of endocrine therapy for 1-2 months, but not for three months (13).
Moreover, during the pandemic, face masks were of paramount importance for COVID-19 prevention, and they were mandatory in healthcare structures in many countries. Clearly, since the beginning of the pandemic, the daily wearing of face masks had been another important change in worldwide practices.
So, important measures were taken at the beginning of the pandemic, even if they were based on preliminary data. Retrospectively, and based on the impact of cancer on the evolution of COVID-19, some proceedings were abandoned. The SIS survey showed that, apart from the development of telemedicine and the wearing of face masks, all these changes would not be definitively implemented by breast specialists’ members of the SIS for the following reasons.
Particularities of COVID-19 in women currently treated for BC
First, women have a lower risk of having COVID-19 than men. Growing evidence in the scientific literature shows that men are at higher risk of severe forms of COVID-19 and have higher mortality (14, 15, 16). These findings are true for most countries, except for Canada, Vietnam, and Belgium (17), where these differences can be explained by epidemiological factors such as age (15, 16), health behavior (15), socioeconomic context (15), different comorbidities (16), and different immune responses (18). Consequently, data concerning women with cancer was probably too alarming.
Second, women with BC have a lower risk of having COVID-19 than women with other cancers. It was supposed that SARS-CoV-2 infection could have higher direct mortality in BC patients, as they may develop more severe forms of the disease. However, new evidence was published that softened the initial fear. Indeed, COVID-19’s impact on mortality is not the same according to cancer type. By analyzing the cancer type, Lee et al. (19) found in a British cohort of 800 patients that BC was at low risk of mortality compared with other cancers (OR: 0.48 (0.28–0.84), p = 0.009). In addition, the authors found that COVID-19-related mortality was principally caused by age, gender, and comorbidities. Vuagnat et al. (20) published a study on 76 patients with early or metastatic BC and suspected COVID-19 among a French cohort of 15,600 patients. They found that 10% were transferred to an intensive care unit, and 7% died (all of whom had significant non-cancer comorbidities). The statistical analysis found that hypertension and age (>70) were the two factors associated with a higher risk of intensive care unit admission and/or death. Interestingly, a history of radiotherapy or current oncological treatment was not associated with mortality. Kalinsky et al. (21) published a report on 27 patients with BC in a cohort of 4,515 patients with COVID-19 from New York City. They found a mortality rate of 4% (n = 1), an 87-year-old male with coronary artery disease, hypertension, and smoking history. De Melo et al. (22) analyzed a population of 40 patients with BC in a Brazilian cohort of 181 patients with cancer and COVID-19. They found that mortality was associated with symptomatic COVID-19 and the presence of two or more metastatic sites in the multivariate analysis. According to the literature, COVID-19’s mortality in BC patients seems to be lower than initially estimated compared with other cancers.
Third, late diagnosis because of the lockdown and screening discontinuation may lead to increased BC-related mortality. Vanni et al. (23) conducted a multicentric cohort study in Italy to evaluate the impact of screening suspension and surgical delay on BC staging. They included 432 patients and found that the disease was more advanced at diagnosis with more lymph node involvement. In addition, Maringe et al. (24) studied the impact of COVID-19 and the lockdown period in England and established a predictive model of BC mortality. They estimated that there would be a 7.9%-9.6% increase in the number of deaths due to BC up to year five after diagnosis in England. Johnson et al. (25) conducted a meta-analysis to evaluate how surgical delay affected survival in breast, lung, and colon cancers. They included 25 articles, of which 12 concerned BC. They found that delaying surgery for 12 weeks might decrease overall BC survival (hazard ratio: 1.46, 95% CI: 1.28–1.65). When BCs were analyzed by stage, the authors found that survival was decreased in early stages (I and II, respectively 1.27, 95% CI: 1.16–1.40; and II 1.13, 95% CI: 1.02–1.24) but not in advanced BC.
Considering these findings, many BC specialists suggest that young and middle-aged patients with BC and without comorbidities should be treated without delay during the pandemic. Only patients aged 65 years old or older and with one or more comorbidities (hypertension, diabetes, chronic respiratory disease, and obesity) should have their treatment adapted to lower COVID-19 risk.
Should caution be maintained for patients formerly treated for BC?
Women treated over five years ago for BC are not at increased risk of having the severe form of COVID-19. However, the effects of COVID-19 on BC recurrence were hypothesized. For example, Francescangeli et al. (26) suggested that potential mechanisms could be implicated in reawakening dormant BC cells. In particular, pulmonary dormant BC cells could be reactivated by COVID-19 infection via immune pathways. In a review published by Silvin et al. (27), the authors highlight that severe COVID-19 is linked to an inflammatory burst and lymphopenia related to carcinogenesis and may aggravate cancer prognosis. Even if data are published on COVID-19 immune-mediated cancer recurrence, further studies are needed to assess this potential risk. When possible, telemedicine should be encouraged for BC survivors’ follow-up to avoid contact with SARS-CoV-2.
In conclusion, the SIS survey showed significant changes in BC diagnosis and treatment changes during the first wave of the COVID-19 pandemic. Participants in this survey emphasized that most of these changes should not be maintained. Indeed, women have less severe forms of COVID-19 and are less likely to die from COVID-19 than men. The risk of dying from COVID-19 is more related to the presence of comorbidities and age than to BC. Suspending screening and delaying cancer treatment led to more advanced stages of BC. All these delays in BC management may potentially influence BC mortality, even if this effect will not become apparent before probably 7–10 years. Only women aged over 65 with cancer under treatment and comorbidities require an adaptation of their cancer management. When possible, telemedicine should be encouraged for BC survivors’ follow-up.
Key Points
• Breast cancer diagnosis and treatment were deeply impacted since the beginning of the SARS-CoV-2 pandemic.
• In the light of recent findings on COVID-19 risk among women with breast cancer, most of these changes should not be maintained as the risk of severe COVID-19 is related to comorbidities and age rather than breast cancer.
• Only women with breast cancer aged over 65 or with comorbidities require adaptation of their cancer management, according to the Senologic International Society.
Acknowledgments
We thank Gérard Hrodej for the help to contact the SIS network members.
Footnotes
Ethics Committee Approval: Please find attached the positive advice, reference CE-2021-38, of our Ethics Committee «Comité d’Ethique des Facultés de Médecine, d’Odontologie, de Pharmacie, des Ecoles d’Infirmières, de Kinésithérapie, de Maïeutique et des Hôpitaux» of March 22nd, 2021.
Informed Consent: Retrospective study.
Peer-review: Externally peer-reviewed.
Authorship Contributions
Conception: C.M., S.A., M.L., M.M.C.; Design: C.M., M.L., M.M.C.; Data Collection or Processing: C.M., St.A., E.A., W.M.B., K.B., H.A.A., J.C.C., V.D., E.E., C.E., T.E., E.I., S.I., L.I.M., E.A.K., M.K., Mi.K., F.L., M.M., Ma.M., A.M., R.O., V.O., S.Ö., V.Ö., O.P., T.P., S.S., E.S., Z.P., M.L., M.M.C.; Analysis or Interpretation: C.M., St.A., E.A., W.M.B., K.B., H.A.A., J.C.C., V.D., E.E., C.E., T.E., E.I., S.I., L.I.M., E.A.K., M.K., Mi.K., F.L., M.M., Ma.M., A.M., R.O., V.O., S.Ö., V.Ö., O.P., T.P., S.S., E.S., Z.P., M.L., M.M.C.; Literature Search: C.M., S.A., M.L., M.M.C.; Writing: C.M., S.A., M.L., M.M.C.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study received no financial support.
References
- 1.Liang W, Guan W, Chen R, Wang W, Li J, Xu K, et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21:335–337. doi: 10.1016/S1470-2045(20)30096-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Miyashita H, Mikami T, Chopra N, Yamada T, Chernyavsky S, Rizk D, et al. Do patients with cancer have a poorer prognosis of COVID-19? An experience in New York City. Ann Oncol. 2020;31:1088–1089. doi: 10.1016/j.annonc.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. doi: 10.3322/caac.21492. [DOI] [PubMed] [Google Scholar]
- 4.Darai E, Mathelin C, Gligorov J. Breast cancer management during the COVID 19 pandemic: French guidelines. Eur J Breast Health. 2020;16:160–161. doi: 10.5152/ejbh.2020.200420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Soran A, Gimbel M, Diego E. Breast cancer diagnosis, treatment and follow-up during COVID-19 pandemic. Eur J Breast Health. 2020;16:86–88. doi: 10.5152/ejbh.2020.240320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cakmak GK, Ozmen V. Sars-CoV-2 (COVID-19) outbreak and breast cancer surgery in Turkey. Eur J Breast Health. 2020;16:83–85. doi: 10.5152/ejbh.2020.300320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fu L, Wang B, Yuan T, Chen X, Ao Y, Fitzpatrick T, et al. Clinical characteristics of coronavirus disease 2019 (COVID-19) in China: a systematic review and meta-analysis. J Infect. 2020;80:656–665. doi: 10.1016/j.jinf.2020.03.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.de Azambuja E, Brandão M, Wildiers H, Laenen A, Aspeslagh S, Fontaine C, et al. Impact of solid cancer on in-hospital mortality overall and among different subgroups of patients with COVID-19: a nationwide, population-based analysis. ESMO Open. 2020;5:e000947. doi: 10.1136/esmoopen-2020-000947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.de Azambuja E, Trapani D, Loibl S, Delaloge S, Senkus E, Criscitiello C, et al. ESMO Management and treatment adapted recommendations in the COVID-19 era: breast cancer. ESMO Open. 2020;5(Suppl 3):e000793. doi: 10.1136/esmoopen-2020-000793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Seely JM, Scaranelo AM, Yong-Hing C, Appavoo S, Flegg C, Kulkarni S, et al. COVID-19: safe guidelines for breast imaging during the pandemic. Can Assoc Radiol J. 2020;71:459–469. doi: 10.1177/0846537120928864. [DOI] [PubMed] [Google Scholar]
- 11.Lin DD, Meghal T, Murthy P, Mo L, D’Silva A, Huang Y, et al. Chemotherapy treatment modifications during the COVID-19 outbreak at a Community Cancer Center in New York City. JCO Glob Oncol. 2020:1298–1305. doi: 10.1200/GO.20.00309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Spencer K, Jones CM, Girdler R, Roe C, Sharpe M, Lawton S, et al. The impact of the COVID-19 pandemic on radiotherapy services in England, UK: a population-based study. Lancet Oncol. 2021;22:309–320. doi: 10.1016/S1470-2045(20)30743-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Park KU, Gregory ME, Lustberg MB, Bazan JG, Shen C, Rosenberg SM, et al. Abstract SS2-05: emerging from COVID-19 pandemic: provider perspective on use of neoadjuvant endocrine therapy (NET) in early stage hormone receptor positive breast cancer. Cancer Res. 2021;81(Suppl 4):SS2-05-SS2. [Google Scholar]
- 14.Chen N, Zhou M, Dong X, Qu J, Gong F, Han Y, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020;395:507–513. doi: 10.1016/S0140-6736(20)30211-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gebhard C, Regitz-Zagrosek V, Neuhauser HK, Morgan R, Klein SL. Impact of sex and gender on COVID-19 outcomes in Europe. Biol Sex Differ. 2020;11:29. doi: 10.1186/s13293-020-00304-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Meng Y, Wu P, Lu W, Liu K, Ma K, Huang L, et al. Sex-specific clinical characteristics and prognosis of coronavirus disease-19 infection in Wuhan, China: a retrospective study of 168 severe patients. PLoS Pathog. 2020;16:e1008520. doi: 10.1371/journal.ppat.1008520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Global Health 5050. The Covid-19 sex-disaggredated data tracker. Available from: [Internet] https://globalhealth5050.org/2020 .
- 18.Takahashi T, Ellingson MK, Wong P, Israelow B, Lucas C, Klein J, et al. Sex differences in immune responses that underlie COVID-19 disease outcomes. Nature. 2020;588:315–320. doi: 10.1038/s41586-020-2700-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee LY, Cazier JB, Angelis V, Arnold R, Bisht V, Campton NA, et al. COVID-19 mortality in patients with cancer on chemotherapy or other anticancer treatments: a prospective cohort study. Lancet. 2020;395:1919–1926. doi: 10.1016/S0140-6736(20)31173-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vuagnat P, Frelaut M, Ramtohul T, Basse C, Diakite S, Noret A, et al. COVID-19 in breast cancer patients: a cohort at the Institut Curie hospitals in the Paris area. Breast Cancer Res. 2020;22:55. doi: 10.1186/s13058-020-01293-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kalinsky K, Accordino MK, Hosi K, Hawley JE, Trivedi MS, Crew KD, et al. Characteristics and outcomes of patients with breast cancer diagnosed with SARS-Cov-2 infection at an academic center in New York City. Breast Cancer Res Treat. 2020;182:239–242. doi: 10.1007/s10549-020-05667-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.de Melo AC, Thuler LCS, da Silva JL, de Albuquerque LZ, Pecego AC, Rodrigues LOR, et al. Cancer inpatients with COVID-19: a report from the Brazilian National Cancer Institute. PLoS One. 2020;15:e0241261. doi: 10.1371/journal.pone.0241261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vanni G, Tazzioli G, Pellicciaro M, Materazzo M, Paolo O, Cattadori F, et al. Delay in breast cancer treatments during the first COVID-19 lockdown. a multicentric analysis of 432 Patients. Anticancer Res. 2020;40:7119–7125. doi: 10.21873/anticanres.14741. [DOI] [PubMed] [Google Scholar]
- 24.Maringe C, Spicer J, Morris M, Purushotham A, Nolte E, Sullivan R, et al. The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study. Lancet Oncol. 2020;21:1023–1034. doi: 10.1016/S1470-2045(20)30388-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Johnson BA, Waddimba AC, Ogola GO, Fleshman JW. A systematic review and meta-analysis of surgery delays and survival in breast, lung and colon cancers: implication for surgical triage during the COVID-19 pandemic. Am J Surg. 2020;S0002-9610(20)30793:5. doi: 10.1016/j.amjsurg.2020.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Francescangeli F, De Angelis ML, Zeuner A. COVID-19: a potential driver of immune-mediated breast cancer recurrence? Breast Cancer Res. 2020;22:117. doi: 10.1186/s13058-020-01360-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Silvin A, Chapuis N, Dunsmore G, Goubet AG, Dubuisson A, Derosa L, et al. Elevated calprotectin and abnormal myeloid cell subsets discriminate severe from mild COVID-19. Cell. 2020;182:1401–18 e18. doi: 10.1016/j.cell.2020.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]


