Abstract
The authors investigated the relationship between the awareness of dietary salt and genetics and the intent to maintain a low‐salt diet. In particular, they assessed whether hypothetical genetic information regarding salt‐sensitive hypertension motivates the intent to reduce dietary salt for communicating the health benefits of lower salt consumption to citizens. A self‐administered questionnaire survey was conducted with 2500 randomly sampled residents aged 30 to 69 years living in Nagahama, Japan. Genetic information regarding higher salt sensitivity increased motivation to reduce salt intake for both those who agreed that genes cause hypertension and those who did not. Less than 50% of those who agreed that genes cause hypertension lost their intention to lower their salt consumption when they found they did not possess the susceptibility gene. Communicating genetic information positively affected motivation to reduce salt intake. The present study clarifies the difficulty in changing the behavioral intent of those who have significantly less incentive to reduce salt intake. Therefore, a multidimensional approach is crucial to reduce salt consumption.
Numerous studies have demonstrated the association of high salt intake with high blood pressure (BP),1, 2, 3, 4 which increases the risk of cardiovascular disease. Salt intake is also associated with an increased risk of stomach cancer5, 6 as well as obesity, renal disease, osteoporosis, and other diseases.7, 8 Several countries have initiated salt‐reduction programs that include efforts such as encouraging food suppliers to voluntarily decrease salt content and improving public awareness and knowledge.7, 8, 9, 10 Moreover, the controlled rate of hypertension has improved as a result of an education program involving healthcare physicians that was designed by a group of nationwide multidisciplinary professionals in Canada.11, 12
The Japan Society of Hypertension recommends a daily salt intake >6 g.13 However, the average daily salt intake in Japan is 11.3 g among adult men and 9.6 g among adult women.14 The average Japanese salt intake has been decreasing by approximately 2% annually for 10 years but remains far from the goal, and Japan lacks a nationwide cross‐disciplinary campaign to reduce salt in the diet.
Katsuya and colleagues15 compared the allele frequency of candidate genes for salt‐sensitive hypertension between Japanese and Caucasians and found that 81% of Japanese individuals have a polymorphism in the gene encoding angiotensinogen (AGT/T235), which is a candidate risk factor for salt‐sensitive hypertension. AGT/T235 and other polymorphisms in four other candidate genes for salt‐sensitive hypertension occur at significantly higher frequencies in Japanese compared with Caucasians. Hunt and associates16 suggested that preventatively reducing salt is the ideal intervention for people with high salt sensitivity. Therefore, salt reduction is likely the most effective approach for the prevention of hypertension in Japanese persons who are genetically sensitive to dietary salt.17
So far, the results of analyses of the genotypes of individuals acquired through genomic cohorts have not been returned to the study participants. However, public knowledge of genetics and genomics is increasing, and clinicians are starting to treat patients in light of their genetic constitution. Thus, there have been intensive discussions on returning genetic results for the participants' own good.18 In 2008, the Kyoto University Graduate School of Medicine and Nagahama City in Japan initiated the Nagahama Study for Comprehensive Human Bioscience (the Nagahama study) for promoting public health and developing community‐based genome‐epidemiologic studies.19 In 2007, the Nagahama study conducted a preliminary survey of Nagahama residents' willingness to participate in these studies.20 The results indicated that approximately 75% of respondents desired health benefits for themselves and their families through their genetic information, revealing a significant willingness to participate in the Nagahama study.
Genetic information regarding disease susceptibility does not provide benefits unless those informed of their genetic risks are motivated to develop healthy behaviors.21, 22 Therefore, identifying the public's prior knowledge of risk factors is required for successful health communication.23, 24 However, very few studies have addressed public attitudes toward genetic information, such as awareness of genetic and other risk factors of multifactorial diseases.
Therefore, the goals of the present study were as follows: (1) to investigate public awareness of salt and genes as risk factors for disease, and the relationship between awareness and the intent to reduce dietary salt; and (2) to determine whether genetic information on salt‐sensitive hypertension motivates the intent to reduce dietary salt to serve as the foundation for future communication designed to lower salt intake among the residents of Nagahama.
Methods
Participants and Setting
The Nagahama City Health Promotion Section conducted this study as part of its survey on health/lifestyle to evaluate residents' health awareness and provide effective health services. In March and April 2012, data were collected using an anonymous, self‐administered questionnaire delivered by regular mail. The questionnaire packet included a briefing paper about the study and instructions for completing the questionnaire. Returning the questionnaire was viewed as implied consent. In compliance with local regulations, a random sampling of 2500 participants (aged 30–69 years) was selected from the Basic Resident Register. The Kyoto University Graduate School and Faculty of Medicine Ethics Committee approved the study protocol.
Measures
The questionnaire was developed according to the results of a preliminary survey conducted by the Nagahama study20 and the Japanese nationwide survey on public attitudes toward genetic studies.25 Revisions were made according to the advice of public health researchers and recommendations by staff members of the Nagahama City Health Promotion Section (see Appendix). The survey items were as follows:
Association of Following a Low‐Salt Diet With Awareness of Salt and Genes as Protective Factors for Hypertension and Cancer
The self‐rated presence or absence of following a low‐salt diet was queried. Each participant chose three or fewer behaviors among the items according to the Japanese Health Promotion Act26 as follows: (1) low‐salt diet, (2) sufficient vegetables and fruit, (3) appropriate exercise, (4) adequate sleep, (5) protection against stress, (6) enjoying a hobby, (7) no smoking, (8) no drinking alcohol, and (9) gene or inherited constitution as protective factors associated with hypertension and cancer. Respondents were asked to choose three or fewer behaviors to avoid the choice of only familial risk factors, and because other factors might be ignored when choosing a single answer from the list. For example, people tend to mistakenly regard multifactorial diseases such as cancer as caused by only a single risk factor.27 According to a study of public awareness of lifestyle risk factors, in answering open‐ended questions, respondents identified an average of 2.1 and 1.4 risk factors for heart disease and cancer, respectively.27 Therefore, a choice of three or fewer behaviors was offered to minimize this bias.
Willingness to Adopt a Low‐Salt Diet After Receiving Genetic Information Regarding Salt‐Sensitive Hypertension
Questions were asked related to the hypothetical scenarios as follows: (1) “Hypothetically speaking, if you were informed of being predisposed to high blood pressure because of a susceptibility gene for salt‐sensitive hypertension, would you further reduce your salt intake?” (2) “Hypothetically speaking, if you were informed that you are not predisposed to high blood pressure because you do not have a susceptibility gene for salt‐sensitive hypertension, would you reduce further your salt intake?” The answers were scored on a five‐point Likert scale ranging from 1 (completely disagree) to 5 (completely agree).
Individual Factors
Each participant provided his or her age, sex, employment status, formal education, and family structure.
Analyses
All analyses were performed using the statistical software package SPSS version 22.0J for Windows (IBM Corp, Armonk, NY). Chi‐square tests were used to examine associations between self‐reported maintenance of a low‐salt diet as a dependent variable and demographic items and protective factors for hypertension and cancer as independent variables. The length of formal education was dichotomized as “12 and less than 12 years” or “13 and more than 13 years.” Thirteen years or >13 years of formal education applied to participants who received a university education in Japan or not. Logistic regression analyses were employed to identify factors (P<.05, chi‐square test) associated with self‐reported maintenance of a low‐salt diet. Respondents in their 30s and 40s were then combined, because their numbers were fewer than respondents of other ages, and the results of their chi‐square tests revealed that the differences among them were similar. Family structure was dichotomized as “two or more generations living together in the family home” and “one‐generation family and living alone,” because a parent‐child relationship is more important than marital status in Japan. The Mann‐Whitney test was applied to analyze motivation for maintaining a low‐salt diet after receiving genetic information.
Results
Respondents' Characteristics
Among the 2500 questionnaires distributed, 1477 were returned (59.1% response rate). Two who returned blank papers and two respondents of unknown sex were excluded from subsequent analyses. Missing data for other items were negligible (≤1.5% for all variables). Table 1 lists the respondents' demographic and other individual factors.
Table 1.
Respondent Characteristics and Intention to Follow a Low‐Salt Diet
| Characteristics | Intention to Follow a Low‐Salt Diet | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Man | Woman | Man | Woman | |||||||||
| % | No. | % | No. | % | OR | 95% CI | P Value | % | OR | 95% CI | P Value | |
| Total | 100 | 704 | 100 | 769 | ||||||||
| Age group, y | ||||||||||||
| 30–39 | 16 | 112 | 21 | 159 | 13 | 1.00 | <.001 | 23 | 1.00 | <.001 | ||
| 40–49 | 20 | 140 | 23 | 175 | 21 | 1.83 | 0.91–3.66 | 30 | 1.43 | 0.87–2.34 | ||
| 50–59 | 24 | 166 | 26 | 202 | 32 | 3.22 | 1.68–6.17 | 39 | 2.11 | 1.32–3.36 | ||
| 60–69 | 40.0 | 279 | 30 | 232 | 40 | 4.74 | 2.58–8.72 | 59 | 1.75 | 3.02–7.47 | ||
| Formal education period | ||||||||||||
| 12 and < 12 years | 59 | 392 | 56 | 414 | 33 | 1.00 | .023 | 43 | 1.00 | .184 | ||
| 13 and > 13 years | 41 | 271 | 44 | 322 | 24 | 0.66 | 0.47–0.94 | 38 | 0.82 | 0.60–1.10 | ||
| Employment statusa | ||||||||||||
| Full‐time employee | 45 | 316 | 19.0 | 145 | 24 | 1.00 | .006 | 29 | 1.00 | <.001 | ||
| Part‐time employee | 11 | 79 | 33 | 254 | 30 | 1.34 | 0.77–2.32 | 33 | 1.21 | 0.78–1.90 | ||
| Company executive | 4.9 | 34 | 1.4 | 11 | 32 | 1.53 | 0.71–3.29 | 64 | 4.25 | 1.18–15.29 | ||
| Self‐employed | 16 | 111 | 6.7 | 51 | 30.0 | 1.37 | 0.85–2.22 | 42.0 | 1.46 | 0.90–3.43 | ||
| Full‐time homemaker | 0.0 | 0 | 32 | 244 | – | – | – | 50 | 2.41 | 1.55–3.38 | ||
| Unemployed | 16 | 113 | 4.6 | 35 | 42.0 | 2.31 | 1.47–3.65 | 49 | 2.29 | 1.08–4.88 | ||
| Other | 6.7 | 47 | 3.1 | 24 | 41 | 2.25 | 1.19–4.28 | 46 | 2.06 | 0.85–4.95 | ||
| Family structure | ||||||||||||
| Living alone | 6.3 | 44 | 3.9 | 30 | 43 | 1.00 | .005 | 60.0 | 1.00 | <.001 | ||
| One generation | 19 | 130 | 17 | 126 | 40 | 0.87 | 0.44–1.74 | 54 | 0.80 | 0.35–1.79 | ||
| Two generations | 50 | 345 | 52 | 393 | 27 | 0.48 | 0.25–0.90 | 37 | 0.39 | 0.18–0.83 | ||
| Three or more generations | 26 | 178 | 28.0 | 214 | 26.0 | 0.46 | 0.23–0.92 | 35 | 0.35 | 0.16–0.77 | ||
| Do you habitually follow a low‐salt diet? | ||||||||||||
| Yes | 30 | 209 | 40.0 | 303 | ||||||||
| No | 70 | 490 | 60.0 | 454 | ||||||||
| Low‐salt diet is a protective factor of hypertension | ||||||||||||
| Agree | 30 | 1.00 | .093 | 40 | 1.00 | .720 | ||||||
| Disagree | 20 | 0.60 | 0.33–1.09 | 36 | 0.86 | 0.42–1.78 | ||||||
| Low‐salt diet is a protective factor against cancer | ||||||||||||
| Agree | 34 | 1.00 | .098 | 55 | 1.00 | <.001 | ||||||
| Disagree | 27.0 | 0.73 | 0.50–1.06 | 36 | 0.45 | 0.31–0.64 | ||||||
| Hypertension is caused by genes or inherited constitution | ||||||||||||
| Agree | 25 | 1.00 | .263 | 36.0 | 1.00 | .125 | ||||||
| Disagree | 30 | 1.26 | 0.84–1.90 | 42 | 1.29 | 0.94–1.77 | ||||||
| Cancer is caused by genes or inherited constitution | ||||||||||||
| Agree | 29 | 1.00 | .856 | 37 | 1.00 | .085 | ||||||
| Disagree | 29 | 1.03 | 0.73–1.45 | 44 | 1.32 | 0.97–1.79 | ||||||
Abbreviations: CI, confidence interval; OR, odds ratio. aThe classification of the employment status is used by Nagahama City Health Promotion section and were followed here. Data were evaluated using the chi‐square test.
Association of Low‐Salt Diet With Awareness of Dietary Salt and Genes as Risk Factors for Hypertension and Cancer
Thirty percent of the men and 40% of the women reported that they followed a low‐salt diet. Women, compared with men, were significantly more likely to follow a low‐salt diet (P<.001). The number of respondents who followed a low‐salt diet increased with age and when living with fewer generations of family (Table 1).
Common behaviors that respondents engaged in to protect against hypertension included a “low‐salt diet” (80%) followed by “appropriate exercise” (40%). Responses to questions regarding preventing cancer were as follows: “no smoking” (66%) and “gene or inherited constitution” (50%). These results are shown in Figure 1.
Figure 1.

Awareness of the factors associated with reduced risk of hypertension and cancer. Three or fewer answers allowed.
Logistic regression analyses were performed to identify demographic factors and the awareness of salt and the gene associated with the intent to reduce dietary salt. Men in their 50s (P=.028) and 60s (P=.002) who lived in a one‐generation family or lived alone (P=.018) reported significantly more often that they followed a low‐salt diet compared with men in their 30s and 40s and those who lived with two or more generations. Women in their 50s (P=.030) and 60s (P<.001) and those who thought salt causes cancer (P=.001) reported significantly more frequently that they followed a low‐salt diet. For women, living with fewer family generations was not a significant factor but was still somewhat associated with following a low‐salt diet (P=.072). No other factors were associated with the intent to reduce dietary salt (Table 2).
Table 2.
Factors Associated With the Intention of Following a Low‐Salt Diet
| Man | Woman | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | P Value | OR | 95% CI | P Value | |
| Age group, y | ||||||
| 30–49 | 1 | 1 | ||||
| 50–59 | 1.78 | 1.07–2.97 | .028 | 1.58 | 1.05–2.40 | .030 |
| 60–69 | 2.50 | 1.39–4.49 | .002 | 3.42 | 2.12–5.51 | <.001 |
| Formal education period | ||||||
| 12 and <12 years | 1 | 1 | ||||
| 13 and >13 years | 0.84 | 0.56–1.28 | .422 | 1.40 | 0.97–2.01 | .075 |
| Employment status | ||||||
| Full‐time employee | 1 | 1 | ||||
| Part‐time employee | 0.75 | 0.36–1.56 | .447 | 0.92 | 0.56–1.50 | .722 |
| Company executive | 1.36 | 0.59–3.14 | .478 | 3.05 | 0.78–11.85 | .108 |
| Self‐employed | 0.83 | 0.44–1.56 | .567 | 1.13 | 0.52–2.48 | .759 |
| Full‐time homemaker | – | – | – | 1.40 | 0.85–2.32 | .185 |
| Unemployed | 1.23 | 0.63–2.37 | .547 | 0.84 | 0.32–2.20 | .962 |
| Other | 1.84 | 0.76–4.47 | .180 | 0.68 | 0.45–1.03 | .720 |
| Family structure | ||||||
| Living alone and with one generation | 1 | 1 | ||||
| Living with two or more generation | 0.60 | 0.39–0.91 | .018 | 0.68 | 0.45–1.03 | .072 |
| Low‐salt diet is a protective factor of cancer | ||||||
| Agree | 1 | 1 | ||||
| Disagree | 0.76 | 0.51–1.16 | .207 | 0.51 | 0.35–0.76 | .001 |
Abbreviations: CI, confidence interval; OR, odds ratio. Data were evaluated using logistic regression analysis.
Willingness to Adopt a Low‐Salt Diet After Receiving Genetic Information Regarding Salt‐Sensitive Hypertension
Answers to the first hypothetical question of possessing a susceptibility gene were as follows: 82% agreed (“completely agree” and “somewhat agree”), 9% were undecided, and 8% disagreed (“completely disagree” and “somewhat disagree”). Answers to the second hypothetical question of not having a susceptibility gene scenario were as follows: 35% agreed, 25% were undecided, and 40% disagreed. To assess the effect of genetic information on the intent to reduce dietary salt, the Mann‐Whitney test was used to compare those who chose “gene or inherited constitution” as a protective factor against hypertension and those who did not choose this item. No significant differences were detected between these two groups related to the presence of a susceptibility gene for salt‐sensitive hypertension (P=.793). Although there was a significant difference in the frequency of answers to not having a susceptibility gene (P<.001), those who chose “gene or inherited constitution” were less motivated to follow a reduced‐salt diet (Table 3).
Table 3.
Differences in Willingness to Follow a Low‐Salt Diet Between Patients Who Agree that Genes Cause Hypertension and Those Who Disagree
| Genes Cause Hypertension | P Value | ||||
|---|---|---|---|---|---|
| Agree | Disagree | ||||
| Mean | SD | Mean | SD | ||
| Want to reduce salt after receiving information of having a gene for salt‐sensitive hypertension | 4.01 | 0.84 | 4.00 | 0.85 | .793 |
| Want to reduce salt after receiving information of not having a gene for salt‐sensitive hypertension | 2.80 | 0.98 | 3.01 | 1.02 | <.001 |
Abbreviation: SD, standard deviation. Data were evaluated using the Mann‐Whitney test.
Willingness to adopt a low‐salt diet after receiving genetic information regarding salt‐sensitive hypertension was compared between those following a low‐salt diet and those who did not (Figure 2). Irrespective of whether the respondents harbored the susceptibility gene for hypertension, there were significant differences between those following a low‐salt diet and those who did not (P<.001). However, <50% of those who responded that they did not follow a low‐salt diet did not agree to reduce salt consumption in the absence a susceptibility gene.
Figure 2.
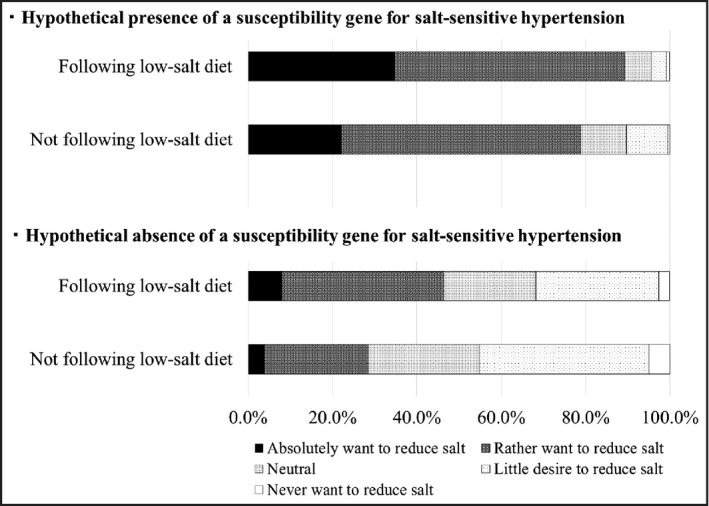
Willingness to follow a low‐salt diet after receiving genetic information.
Discussion
In the present study, women responded that they followed a low‐salt diet more frequently than men. Further, the results indicated that participants living with fewer family generations were more cautious about dietary salt intake. Other studies that address the public's knowledge of the health effects of dietary salt report sex differences in objective and/or subjective opinions regarding salt intake.11, 28 For example, Chung and colleagues28 suggested that women are more knowledgeable about heart failure than men and that men had difficulty eating what they desired because women often planned and prepared their meals. Gee and coworkers11 reported that younger men were less likely to adhere to limited salt consumption. The most common barrier for men against salt reduction was a lack of will power/self‐discipline. Most of the younger men in this study lived with their family (see Figure A1) and thus might not have prepared their own meals, ie, they may leave the choice of restricted salt intake to their mothers or wives. These findings are consistent with those reported in the present study, reinforcing the importance of considering low‐salt diet recommendations in light of the person's personal situation.
In studies of the relationship between a low‐salt diet and family structure, no robust evidence has yet been provided. According to a nationwide survey in Japan29 unmarried women consumed less salt than married women, while there was no significant association with salt intake among married or unmarried men. In a Korean study30 the number of family members did not affect 24‐hour urinary sodium excretion. In the present study, men who lived with one generation of family or lived alone were significantly more likely to follow a low‐salt diet. For women, a difference was also observed between those who lived with one generation of family and lived alone and their counterparts until entering formal education and age into the model simultaneously as the independent variable (see Figure A2). These findings might affect the intention to follow a low‐salt diet. Bentley and colleagues31 found that “interference with socialization” was a reason for patients with heart failure not to adhere to a low salt‐diet. Further, participants described family conflicts about consuming salty dishes that prevented the implementation of a reduced‐salt diet. Nørgaard and associates32 found that parents compromised their children's food choices to maintain harmony within the family, and this finding is consistent with those of the present study. Because a higher proportion of extended families live in Nagahama compared with the national average,33 it is recommended that all family members participate in reducing dietary salt intake.
Sanderson and colleagues27 found that awareness of associations between lifestyle and heart disease was higher compared with associations between lifestyle and cancer. According to the study, 68% of respondents identified “eating an unhealthy diet” and 53% identified “being physically inactive” as causal factors of heart disease, which may be explained by the success of public health campaigns. Similarly, in the present study, respondents considered hypertension as a controllable illness associated with salt intake and physical inactivity, likely because of the success of public health communication campaigns.34, 35 However, in the present study, there was no significant association between awareness that a low‐salt diet can prevent hypertension and following such a diet. Protection motivation theory proposed by Rogers36 attempts to understand behavior changes to avoid risks. Rogers hypothesizes that protection motivation is aroused by two integrated processes, ie, threat appraisal by evaluating negative outcomes posed by risk behavior, and coping appraisal by evaluating one's ability to cope with risk‐averse behaviors that consist of the response efficacy, self‐efficacy, and response costs. Participants might perceive the threat of hypertension as low. Indeed, several studies have reported that, for the public, hypertension does not seem to pose a threat.12, 37, 38 Steiner and coworkers38 suggested that the majority of the public does not know that hypertension is mostly an asymptomatic disease known as “the silent killer.” According to a study by Petrella and Campbell,12 most of the general public in Canada is unaware of the association between hypertension and heart disease and believes that hypertension is not a serious medical condition. Women, but not men, who were aware that a low‐salt diet is a protective factor for cancer reported following a low‐salt diet. This might suggest the possibility that a high threat of disease, high awareness of risk factors, and their ability to cope with risk‐averse behaviors (ie, preparing a low‐salt diet) lead to appropriate behaviors.
Most of the respondents in the present study might perceive genetic risk as conquerable, as many of them desired to reduce their salt intake if they carried a susceptibility gene. This view is supported by findings that most participants believed in “a gene for heart disease,” which means that genetic and environmental factors play roles in developing disease and increased risk.39 Moreover, more than half of the respondents to questions regarding the absence of a susceptibility gene for salt‐sensitive hypertension were not discouraged from reducing their salt intake. This observation indicates that informed genetic risk is helpful in promoting a low‐salt diet, because most Japanese citizens will be informed of the possibility of carrying the susceptibility gene for salt‐sensitive hypertension when returning the results of genetic testing,15 and that those without the gene are motivated, nevertheless, to follow a low‐salt diet. Nielsen and El‐Sohemy40 compared the effects of providing genotype‐based personalized dietary advice with general advice without genetic information on salt reduction behavior. According to the study, there was a significant difference in reducing salt intake between those with the wild‐type angiotensin‐converting enzyme, which affects salt sensitivity, and receiving targeted recommendations for salt and those receiving general recommendations for their diet without genetic information (control group). Meanwhile, there was no difference between those without the wild‐type angiotensin‐converting enzyme with targeted recommendation and those in the control group. The present study's results also support these previous findings. In particular, the conclusion of Nielsen and El‐Sohemy's study,40 showing that it is more effective to communicate genetic information to motivate favorable lifestyle changes than to test for disease susceptibility, should be appreciated.
Analysis of the willingness to follow a low‐salt diet among those with a susceptibility gene for salt‐sensitive hypertension showed no significant difference between those with or without a “gene or inherited constitution” that causes hypertension. It is therefore concluded that it is unreasonable to expect those who do not believe that genes cause disease will be motivated to change their behavior according to the information provided to them about their genotype. Moreover, respondents in the present study exhibited attitudes toward reducing salt intake by separating “health to behavior” and “health to genes.” However, more than half of those who believed that a “gene or inherited constitution” causes hypertension were not demotivated to follow a low‐salt diet in the absence of a susceptibility gene. The availability of genetic information had a greater impact on its relation to disease than to good health.22
Study Limitations
This study had several limitations. First, adhering to a low‐salt diet was self‐reported. According to a study by Okuda and colleagues,41 there was no difference in salt intake between those reporting a reduced salt diet and others by subgroup analyses in light of their hypertensive conditions. Thus, additional study is needed to determine to what extent a self‐reported low‐salt diet reflects true salt consumption. In the present study, however, self‐rated salt intake was useful as a baseline to measure motivational changes when genetic information was communicated. For example, behavioral intention is crucial for changing behavior.42, 43 Moreover, after receiving genetic information, those who reported following a low‐salt diet improved their motivation to reduce salt consumption more than those who did not. This result indicates that those who reported following a low‐salt diet did not consider their salt intake sufficiently low and thought that they should reduce their salt intake further. In fact, no ceiling effect was observed. Second, respondents were not asked about their history of hypertension and cancer, which might affect their perception of these diseases. Finally, Nagahama is historically traditional in that more extended families live together than in the rest of the country. Therefore, the findings of this study might not apply to emerging and urban areas where more nuclear families reside.
Health communication for promoting a low‐salt diet might be suggested as follows: (1) increase the perception of threat by heightening awareness of the adverse outcomes of hypertension; (2) increase efficacy by publicizing that excess salt is associated with cancer, which is perceived by some as uncontrollable; and (3) provide genetic information on salt‐sensitive hypertension to be shared by family members so that all generations will adopt a low‐salt diet. It is necessary to conduct future research on increasing awareness and designing a program that includes all family members.
Conclusions
The present study clarifies the difficulty in changing the behavioral intent of those who show significantly less incentive to reduce their salt intake, whether or not they harbor a susceptibility gene for salt‐sensitive hypertension, compared with those who reported following a low‐salt diet. Therefore, a multidimensional approach is crucial to reduce salt consumption. The data from this study show that communicating genetic information regarding salt‐sensitive hypertension will serve as an acceptable approach for motivating the intention to reduce salt consumption and that it is difficult to manage healthy behaviors without the cooperation of family members.
Acknowledgments
We would like to thank the citizens of Nagahama and the Nagahama City Health Promotion section for their cooperation in this research. This project was supported in part by the Nagahama Regional Open Genome Epidemiology Study of RISTEX in the Japan Science and Technology Agency.
Conflicts of Interest
There are no conflicts of interest to declare for all authors.
Figure A1.

Association between family structure and age.
Figure A2.

Association between family structure and formal education period.
Appendix Table A. Questionnaire

J Clin Hypertens (Greenwich). 2017;19:270–279. 10.1111/jch.12897 © 2016 Wiley Periodicals, Inc.
References
- 1. Intersalt Cooperative Research Group . Intersalt: an international study of electrolyte excretion and blood pressure: results for 24 hour urinary sodium and potassium excretion. BMJ. 1988;297:319–328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. He FJ, Li J, Macgregor GA. Effect of longer‐term modest salt reduction on blood pressure: Cochrane systematic review and meta‐analysis of randomised trials. BMJ. 2013;3:f1325. [DOI] [PubMed] [Google Scholar]
- 3. Siervo M, Lara J, Chowdhury S, et al. Effects of the Dietary Approach to Stop Hypertension (DASH) diet on cardiovascular risk factors: a systematic review and meta‐analysis. Br J Nutr. 2014;28:1–15. [DOI] [PubMed] [Google Scholar]
- 4. Strazzullo P, D'Elia L, Kandala NB, Cappuccio FP. Salt intake, stroke, and cardiovascular disease: meta‐analysis of prospective studies. BMJ. 2009;24:b4567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ge S, Feng X, Shen L, et al. Association between habitual dietary salt intake and risk of gastric cancer; a systematic review of observational studies. Gastroenterol Res Pract. 2012;2012:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Shikata K, Kiyohara Y, Kubo M, et al. A prospective study of dietary salt intake and gastric cancer incidence in a defined Japanese population; the Hisayama Study. Int J Cancer 2006;119:196–201. [DOI] [PubMed] [Google Scholar]
- 7. He FJ, MacGregor GA. A comprehensive review on salt and health and current experience of worldwide salt reduction programmes. J Hum Hypertens. 2009;23:363–384. [DOI] [PubMed] [Google Scholar]
- 8. Campbell NR, Willis KJ, L'Abbe M, et al. Canadian initiatives to prevent hypertension by reducing dietary sodium. Nutrients. 2011;3:756–764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Legowski B, Legetic B. How three countries in the Americas are fortifying dietary salt reduction: a north and south perspective. Health Policy. 2011;102:26–33. [DOI] [PubMed] [Google Scholar]
- 10. Strazzullo P, Cairella G, Camponozzi A, et al. The GIRCSI Working Group. Population based strategy for dietary salt intake reduction: Italian initiatives in the European framework. Nutr Metab Cardiovasc Dis. 2012;22:161–166. [DOI] [PubMed] [Google Scholar]
- 11. Gee ME, Bienek A, Campbell NRC, et al. Prevalence of, and barriers to, preventive lifestyle behaviors in hypertension (from a national survey of Canadians with hypertension.). Am J Cardiol. 2012;109:570–575. [DOI] [PubMed] [Google Scholar]
- 12. Petrella RJ, Campbell NR. Awareness and misconception of hypertension in Canada: results of national survey. Can J Cardiol. 2005;21:589–593. [PubMed] [Google Scholar]
- 13. Japanese Society of Hypertension . The Japanese Society of Hypertension Guidelines for the Management of Hypertension. 2004.
- 14. Ministry of Health, Labour and Welfare . National Health and Nutrition Examination Survey. 2012.
- 15. Katsuya T, Ishikawa K, Sugimoto K, et al. Salt sensitivity of Japanese from the viewpoint of gene polymorphism. Hypertens Res. 2003;26:521–525. [DOI] [PubMed] [Google Scholar]
- 16. Hunt SC, Cook NR, Oberman A, et al. Angiotensinogen genotype, sodium reduction, weight loss, and prevention of hypertension trials of hypertension prevention. Phase II. Hypertension. 1998;32:393–401. [DOI] [PubMed] [Google Scholar]
- 17. Katsuya T, Morishita R, Rakugi H, Ogihara T. Genetic basis of hypertension for the development of tailored medicine. Hypertens Res. 2009;32:643–648. [DOI] [PubMed] [Google Scholar]
- 18. Wallace SE, Kent A. Population biobanks and returning individual research results: mission impossible or new directions? Hum Genet. 2011;130:393–401. [DOI] [PubMed] [Google Scholar]
- 19. Miyamoto K, Iwakuma M, Nakayama T. Residents' awareness and attitudes about an ongoing community‐based genome cohort study in Nagahama. Japan. Public Underst Sci. 2015;24:957–969. [DOI] [PubMed] [Google Scholar]
- 20. Tomoda M. Evaluating the current attitude toward practice and research on human genetics in Japan. Kyoto University School of Public Health Master Thesis. 2008;7:173–180. [Google Scholar]
- 21. Marteau TM, French DP, Griffin SJ, et al. Effects of communicating DNA‐based disease risk estimates on risk‐reducing behaviors. Cochrane Database Syst Rev 2010;610:CD007275. [DOI] [PubMed] [Google Scholar]
- 22. Condit CM, Shen L. Public understanding of risks from gene‐environment interaction in common diseases: implications for public communications. Public Health Genomics. 2011;14:115–124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Marteau TM, Weinman J. Self‐regulation and the behavioral response to DNA risk information: a theoretical analysis and framework for future research. Soc Sci Med. 2006;62:1360–1368. [DOI] [PubMed] [Google Scholar]
- 24. Smerecnik CMR, Mesters I, de Vries NK, de Vries H. Educating the general public about multifactorial genetic disease: applying a theory‐based framework to understand current public knowledge. Genet Med. 2008;10:251–258. [DOI] [PubMed] [Google Scholar]
- 25. Ishiyama I, Nagai A, Muto K, et al. Relationship between public attitudes toward genomic studies related to medicine and their level of genomic literacy in Japan. Am J Med Genet A. 2008;146A:1696–1706. [DOI] [PubMed] [Google Scholar]
- 26. Ministry of Health, Labour and Welfare . Health promotion of a population movement in the twenty‐first century: Kenko Nippon 21. 2000.
- 27. Sanderson SC, Waller J, Jarvis MJ, et al. Awareness of life style risk factors for cancer and heart disease among adults in the UK. Patient Educ Couns. 2009;74:221–227. [DOI] [PubMed] [Google Scholar]
- 28. Chung ML, Moser DK, Lennie TA, et al. Gender differences in adherence to the sodium‐restricted diet in patients with heart failure. J Card Fail. 2006;12:628–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Fukuda Y, Hiyoshi A. Associations of household expenditure and marital status with cardiovascular risk factors in Japanese adults: analysis of nationally representative surveys. J Epidemiol. 2013;23:21–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Hong JW, Noh JH, Kim DJ. Factors associated with high sodium intake based on estimated 24‐hour urinary sodium excretion. Medicine. 2016;95:e2864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Bentley B, De Jong MJ, Moser DK, Peden AR. Factors related to nonadherence to low sodium diet recommendation. Eur J Cardiovasc Nurs. 2005;4:331–336. [DOI] [PubMed] [Google Scholar]
- 32. Nørgaard MK, Brunsø K. Family conflicts and conflict resolution regarding food choices. J Consumer Behav. 2011;10:141–151. [Google Scholar]
- 33. Ministry of Internal Affairs and Communications , Statistics Bureau , Japan National Census: Subregion block. 2010.
- 34. Yokota K, Harada M, Wakabayashi Y, et al. Evaluation of a community‐based health education program for salt reduction through media campaigns. Nihon Koshu Eisei Zassi. 2006;53:543–553. [PubMed] [Google Scholar]
- 35. Matsumura H. Salt‐reduction campaign–new approaches. Cardiongiology. 2013;73:698–704. [Google Scholar]
- 36. Rogers RW. A protection motivation theory of fear appeals and attitude change. J Psych. 1975;91:93–114. [DOI] [PubMed] [Google Scholar]
- 37. Qvist I, Thomsen MD, Lidholt JS, et al. Self‐reported knowledge and awareness about blood pressure and hypertension: a cross‐sectional study of a random sample of men and women aged 60‐74 years. Clin Epidemiol. 2014;6:81–87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Steiner S, Domer TE, Fodor JG, et al. Blood pressure awareness in Austria: lessons from a 30 year horizon. Am J Hypertens. 2011;24:408–414. [DOI] [PubMed] [Google Scholar]
- 39. Bates BB, Templeton A, Achter PJ, et al. What does “A gene for heart disease” mean? A focus group study of public understandings of genetic risk factors. Am J Med Genet. 2003;119A:156–161. [DOI] [PubMed] [Google Scholar]
- 40. Nielsen DE, El‐Sohemy A. Disclosure of genetic information and change in dietary intake: a randomized controlled trial. PLoS ONE. 2014;9:e112665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Okuda N, Stamler J, Brown IJ, et al; for the INTERMAP Research Group. J Hypertens. 2014;32:2385–2392. [DOI] [PubMed] [Google Scholar]
- 42. Ajzen I. The theory of planned behavior: reactions and reflections. Psychol Health. 2011;26:1113–1127. [DOI] [PubMed] [Google Scholar]
- 43. Ludolph R, Schulz PJ. Does regulatory fit lead to more effective health communication? A systematic review Soc Sci Med. 2015;128:142–150. [DOI] [PubMed] [Google Scholar]


