Summary:
Achieving primary closure of lower extremity fasciotomy wounds is difficult. Surgeons are faced with the option of waiting potentially long periods of time for edema to reside, in order to attempt delayed primary closure (DPC) versus closing at an earlier time with a split thickness skin graft. DPC offers superior aesthetic outcomes than split thickness skin grafts but traditionally cannot occur until later in the clinical course once excessive edema has subsided. We present a case of a young athlete with compartment syndrome, which was managed with an alternative technique for achieving DPC: serial partial closure under tension with retention sutures and negative pressure wound therapy. The successful outcome in this single case should prompt further studies investigating the objective benefits of this novel method to achieve DPC following fasciotomy.
Primary closure of fasciotomy wounds is challenging; the muscles bulge outward because they are no longer held compact by their fascial sheaths, the skin retracts due to this muscle bulging, and the soft tissue swells in the acute inflammatory response. Surgeons must choose between using a split thickness skin graft (STSG), which allows for earlier closure, or attempting delayed primary closure (DPC) later in the course once edema has subsided.
When compared with STSG, DPC offers a more aesthetically pleasing result and limits the number of surgical sites. Furthermore, patients treated with STSG have also reported higher levels of pain and discomfort than patients who were not treated with STSG,1 and not all surgeons performing fasciotomies have access to a surgery team for skin graft coverage. The benefits of DPC come at the cost of a longer time to closure and increased rates of wound complications. Johnson et al found that the incidence of wound complications was significantly higher in patients who had dermotomy-fasciotomy wounds closed with primary or secondary closure (51%) relative to those closed with skin grafts (5%; P < 0.01).2 Furthermore, DPC is not a feasible closure option in some wounds, particularly those involving an open fracture or those where it is thought that tissue edema or loss of tissue domain is significant enough that it will preclude future primary closure.3 Weaver et al found that only 21.2% patients could be closed primarily without any wound edge retention method.3
Despite its possible disadvantages relative to STSG, DPC is often chosen as the preferred method for wound closure. Multiple techniques take advantage of mechanical and biological creep for DPC of fasciotomy wounds, with the most common being the rubber band or vessel loop method. Although effective and low cost, closure with this method may take up to 2–3 weeks and requires daily tightening, which is uncomfortable and exposes the wound bed to a nonsterile environment.4–10
Several studies comparing the rubber band or vessel loop method with negative pressure wound therapy (NPWT) have demonstrated that the former method was superior in achieving primary closure without skin grafts: Johnson et al8 found that 5/5 wounds closed with the shoelace method in an average of 8 days versus 1/9 with NPWT in 13 days; Kakagia et al11 found that 40/40 wounds closed with the shoelace method in 15 days versus 36/42 with NPWT in 19 days. DermaClose is a newer, off-the-shelf product that is marketed as a continuous external tissue expander that facilitates DPC in a manner very similar to that of the vessel loop method.12
This case report presents an alternative method to achieve DPC in lower extremity fasciotomy wounds: serial partial closure with retention sutures and NPWT. This closure method takes advantage of the biological and mechanical creep employed by the rubber band and vessel loop techniques as well as NPWT to facilitate wound healing.
CASE
We present a 19-year-old, healthy, male college football player who developed compartment syndrome of his left leg following blunt trauma sustained during football practice. He was taken urgently to the operating room for 4-compartment fasciotomies via medial and lateral leg incisions for spontaneous compartment syndrome. His medial leg incision was closed primarily on postoperative day 3; however, the lateral incision could not be closed at this time due to extensive muscle bulk and swelling. The patient was motivated to try methods alternative to skin grafting due to concerns over the donor site and poor aesthetic outcome.
On postoperative day 5, the patient returned to surgery for attempted closure of the lateral incision. Initial left lateral leg wound measured 28 cm × 8.5 cm (Fig. 1). Bacterial cultures were obtained but were ultimately negative. There were no visual signs of muscle necrosis. Superficial debridement was performed to remove surface-level biofilm and hypergranulation tissue. Debridement was stopped once healthy, bleeding tissue was observed, and the wound bed was irrigated with a total of 3 L of saline. The anterior and posterior skin flaps were undermined approximately 1 cm without devascularizing the skin bridge between the medial and lateral leg incisions, which was functionally a bipedicled flap. 0-Prolene interrupted vertical mattress sutures were placed 0.5 cm from the skin edge and tagged along the incision. An NPWT sponge and nonadherent Mepitel dressing (Mölnlycke Health Care AB, Gothenberg, Sweden) were placed into the defect. The sutures were sequentially tied down under tension over the sponge. Skin edges were visually assessed for skin blanching to ensure that the retention sutures were not under ischemia-inducing tension (Fig. 2). After retention suture placement over the sponge, the size of the wound reduced by 71% percent, to 23 cm × 3 cm (238–69 cm2). At the end of surgery, skin edges and muscle were pink with good turgor, and there were triphasic AT, PT, and peroneal signals. To minimize postoperative edema, his leg was wrapped in a lymphedema wrap, and he was instructed to keep his leg elevated. The NPWT device was set at a continuous pressure of 125 mm Hg.
Fig. 1.

Photograph of the patient showing initial left lateral leg wound measuring 28 cm (length) × 8.5 cm (width).
Fig. 2.
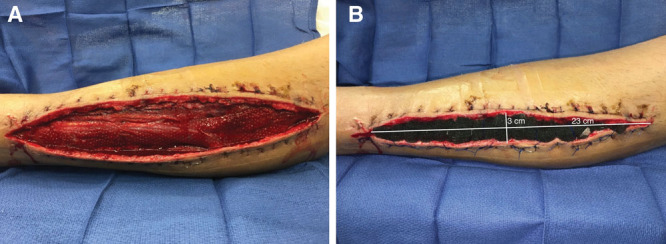
Photographs depicting the use of NPWT and retention sutures to achieve DPC. A nonadherent dressing and NPWT sponge were applied directly onto the muscle (A), with retention sutures placed on the skin edges to allow for creep and stretch of the skin (B).
On postoperative day 9, the patient was taken back to the operating room for closure. Bacterial and fungal cultures were obtained but were ultimately negative. The NPWT device and retention sutures were removed, and on visual examination, the muscles were healthy with no signs of necrosis. 2-0 Prolene interrupted vertical mattress sutures were placed, and the skin edges were closed primarily without undue tension or skin blanching. Skin staples were also used (Fig. 3). A Prevena incision management system (3M, St. Paul, Minn.) was applied. The patient was discharged home and he remains well-healed at 12 months after surgery (Fig. 4).
Fig. 3.

Picture depicting DPC achieved 9 days after placement of retention sutures.
Fig. 4.

Photograph of the patient showing final healed incision 1 year after definitive closure.
DISCUSSION
In this case, retention sutures with NPWT offered a simple alternative to achieving DPC for a lower extremity fasciotomy wound. In our experience, tying down large 0-strength sutures allowed greater tissue reapproximation compared with our experience with the shoelace/rubber band method. Unlike the shoelaces, retention sutures (1) do not require tightening, (2) are less likely to break, (3) do not require staple removal, and (4) reduce exposure of the wound bed to a nonsterile environment. NPWT facilitates wound healing via a variety of mechanisms, including removal of edematous fluid, promotion of wound bed contraction, and enhancement of the inflammatory response.13–15 This case study and report of technique should prompt further studies investigating the objective benefits of this novel method to achieve DPC following fasciotomy.
CONCLUSIONS
Closing fasciotomy wounds with DPC can be challenging. Further clinical studies are warranted to determine the objective benefits of serial retention sutures with NPWT, as our experience has demonstrated that it may offer a simple alternative to reliably achieve DPC in patients with lower extremity fasciotomy wounds.
Footnotes
Published online 8 April 2021.
Disclosure: The authors have no financial interest in relation to the content of this article.
REFERENCES
- 1.Giannoudis PV, Nicolopoulos C, Dinopoulos H, et al. The impact of lower leg compartment syndrome on health related quality of life. Injury. 2002; 33:117–121 [DOI] [PubMed] [Google Scholar]
- 2.Johnson SB, Weaver FA, Yellin AE, et al. Clinical results of decompressivedermotomy-fasciotomy. Am J Surg. 1992; 164:286–290 [DOI] [PubMed] [Google Scholar]
- 3.Weaver MJ, Owen TM, Morgan JH, et al. Delayed primary closure of fasciotomy incisions in the lower leg: do we need to change our strategy? J Orthop Trauma. 2015; 29:308–311 [DOI] [PubMed] [Google Scholar]
- 4.Zorrilla P, Marín A, Gómez LA, et al. Shoelace technique for gradual closure of fasciotomy wounds. J Trauma. 2005; 59:1515–1517 [DOI] [PubMed] [Google Scholar]
- 5.Asgari MM, Spinelli HM. The vessel loop shoelace technique for closure of fasciotomy wounds. Ann Plast Surg. 2000; 44:225–229 [DOI] [PubMed] [Google Scholar]
- 6.Berman SS, Schilling JD, McIntyre KE, et al. Shoelace technique for delayed primary closure of fasciotomies. Am J Surg. 1994; 167:435–436 [DOI] [PubMed] [Google Scholar]
- 7.Kenny EM, Egro FM, Russavage JM, et al. Primary closure of wide fasciotomy and surgical wounds using rubber band-assisted external tissue expansion: a simple, safe, and cost-effective technique. Ann Plast Surg. 2018; 81:344–352 [DOI] [PubMed] [Google Scholar]
- 8.Johnson LS, Chaar M, Ball CG, et al. Management of extremity fasciotomy sites prospective randomized evaluation of two techniques. Am J Surg. 2018; 216:736–739 [DOI] [PubMed] [Google Scholar]
- 9.Suliman MT, Aizaz S. Closing fasciotomy wounds using plastic bands: an alternative simple and cheap method. Ann Vasc Surg. 2008; 22:697–700 [DOI] [PubMed] [Google Scholar]
- 10.Eid A, Elsoufy M. Shoelace wound closure for the management of fracture-related fasciotomy wounds. ISRN Orthop. 2012; 2012:528382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kakagia D, Karadimas EJ, Drosos G, et al. Wound closure of leg fasciotomy: comparison of vacuum-assisted closure versus shoelace technique. A randomised study. Injury. 2014; 45:890–893 [DOI] [PubMed] [Google Scholar]
- 12.Synovis Micro Alliance Companies. DermaClose. Available at: https://dermaclose.com. Accessed September 10, 2020
- 13.Dong J, Qing C, Song F, et al. Potential molecular mechanisms of negative pressure in promoting wound healing. Int Wound J. 2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Argenta LC, Morykwas MJ. Vacuum-assisted closure: a new method for wound control and treatment: clinical experience. Ann Plast Surg. 1997; 38:563–576 [PubMed] [Google Scholar]
- 15.Orgill DP, Bayer LR. Update on negative-pressure wound therapy. Plast Reconstr Surg. 2011; 127Suppl 1105S–115S [DOI] [PubMed] [Google Scholar]


