Abstract
Improving hypertension control is a public health priority and could reduce health disparities. Self blood pressure monitoring (SBPM) is effective but not widely integrated into clinical care. A pragmatic study distributing blood pressure (BP) monitors was conducted to assess its effectiveness in the management of uncontrolled hypertension under conditions consistent with clinic resources. Patients, predominantly black and Hispanic adults from clinics in low‐income, medically underserved communities with uncontrolled BP were enrolled. Follow‐up assessments were conducted 9 months after enrollment. Approximately half (53%) of the patients had controlled hypertension at follow‐up. Systolic and diastolic BP decreased by 18.7 mm Hg and 8.5 mm Hg, respectively, at follow‐up. Although attenuated, decreases persisted after adjustment for regression to the mean. Clinicians were supportive of the program, although collecting follow‐up data from enrolled patients was a common challenge. The integration of SBPM into routine management of uncontrolled hypertension demonstrated substantial improvements in control. Systems to identify and track patients who are self‐monitoring may increase impact. J Clin Hypertens (Greenwich). 2013;00:00–00. ©2013 Wiley Periodicals, Inc.
Although a longstanding priority for both public health and clinical care communities, hypertension remains uncontrolled in just over half of people with this condition in the United States. 1 High blood pressure (BP) is a major and modifiable risk factor for cardiovascular disease, the leading cause of death, and a predominant contributor to health disparities in cardiovascular morbidity and mortality. 2 Improved hypertension control in blacks and Hispanics has the potential to decrease related health disparities because the prevalence of hypertension is higher in black patients and because rates of control are lower in black and Hispanic patients compared with white patients. 3 , 4 Improving control of hypertension could prevent thousands of deaths annually. 5
While lifestyle change should not be overlooked as an important therapeutic component of treatment, 6 the availability of effective and affordable BP‐lowing medications makes widespread control of hypertension an achievable goal. Even among those treated, however, control remains low at 69%. 3 As a result, the integration of new and effective disease management tools into routine clinical care are needed to improve population‐level control. One such approach is self BP monitoring (SBPM). Meta‐analyses of randomized trials have demonstrated improved hypertension control and lower mean diastolic and systolic pressures with home monitor use. 7 , 8 , 9 Still, evidence is limited in low‐income and minority populations, and barriers to using SBPM exist. Barriers include a lack of clear clinical provider guidance, and the out‐of‐pocket cost of the monitor to the patient resulting from inconsistent third‐party reimbursement. 6 , 10
We describe a project of the New York City Department of Health and Mental Hygiene (Health Department) initiated in collaboration with ambulatory care clinics in medically underserved neighborhoods. The project aimed to implement and evaluate the effectiveness of integrating SBPM into the regular management of care for patients with uncontrolled hypertension under conditions consistent with existing clinic resources and infrastructure. The pragmatic study approach allows us to consider whether findings from randomized controlled trials translate in the real‐world setting to achieve improved hypertension control in low‐income, largely minority populations.
Methods
Clinic and Participant Selection
Health Department staff recruited ambulatory clinics located in neighborhoods that are predominantly black and Hispanic, low‐income, and medically underserved. Interested clinics were formally engaged through Letters of Agreement, and patients were recruited by clinic staff.
Patient eligibility criteria included: (1) age 18 years or older, (2) a diagnosis of hypertension for at least 6 months, and (3) current and last healthcare provider visit BP measurement of systolic BP (SBP) ≥140 mm Hg and/or diastolic BP (DBP) ≥90 mm Hg or in those with diabetes or kidney disease, SBP ≥130 mm Hg or DBP ≥80 mm Hg. Patient ineligibility criteria included: (1) physically/mentally unable to use a home BP monitor or record measurements as determined by their health care provider, (2) arm size outside the range noted by the BP monitor manufacturer specifications as appropriate for accurate use, or (3) already engaged in SBPM in the management of their hypertension.
Description of Intervention
Multidisciplinary clinical staff (ie, attending physicians, residents, nurses, medical assistants, and other office staff) received a formal 1‐hour, on‐site training session from the Health Department. Ideally, these were to be held in a combined group setting, although segmented, multiple training sessions were provided on request. The training included a review of the Seventh Report of the Joint National Committee on Prevalence, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7) guidelines for the management of hypertension, 6 teaching on how to use and integrate SBPM into hypertension management, and instructions on data collection and other study logistics. While providers received sample protocols for the recommended frequency of home measurement, we did not require providers to prescribe specific protocols for monitor use or treatment, in order to be consistent with our goal of assessing the use of monitors in the real world.
Each site was given, free of charge, up to 200 automated, upper‐arm BP monitors (Omron HEM‐711AC), patient tote bags, and provider and patient educational materials. During the start‐up phase, Health Department program staff worked with clinic staff to develop workflows for patient referral, monitor distribution, patient training on monitor use, and patient follow‐up. Because clinic operational models varied, workflows were tailored to each site’s capacity, resources, and organizational culture.
During the course of regular office visits, healthcare providers (ie, physicians, nurse practitioners, and physician assistants) identified and referred eligible patients for SBPM training. Trained clinic staff, usually nurses and medical assistants, instructed patients on monitor use, encouraged patients to record home measurements, and gave patients the monitor, educational materials, and a tote bag to carry these items home. Providers were advised to inform participants about the importance of SBPM, provide individual BP targets and recommend actions to take in case of abnormally high or low measurements, encourage patients to record home measurements on a BP tracking card provided by the Health Department, and ask patients to bring this home record to subsequent office visits to discuss with the providers. The program did not dictate a specific follow‐up protocol, and appointments for participating patients were scheduled at the discretion of the patient care staff. For the purposes of program evaluation, the patients were followed for 9 months. All participating patients were given the monitors to keep as their own.
Data Collection
Health Department program staff developed and provided to clinics a tracking log to capture baseline and follow‐up office BP measurements, as well as basic demographic data (age, sex, race/ethnicity) for all enrollees. Clinic staff was trained in data collection and was responsible for entering the data in the tracking log during the program. For the process evaluation we assessed the clinic implementation experience and staff attitudes toward the program by conducting key informant interviews. Interviews were administered in person when logistically feasible and by telephone otherwise. Key informants included the clinical champion(s) and health care providers, medical assistants, nurses, and health educators involved in the program. Using a semi‐structured interview guide we collected information on program implementation (eg, how participants were identified and who was responsible for training patients on monitor use), the perceived effect on clinic workflow, how home BP measurements were used in clinical management, and what challenges were experienced, as well as suggestions for improvement.
Definition of Follow‐Up and Covariates
The goal observation period was 9 months, with inclusion of BP measurements collected between 7 and 11 months to account for usual health care utilization patterns in the real‐world setting. Control of hypertension was defined as office measurements of SBP <140 mm Hg and DBP <90 mm Hg at follow‐up. Information on diabetes or chronic kidney disease was not collected, and thus we did not differentially define control of hypertension at follow‐up based on these conditions.
Statistical Analysis
A pre‐post intervention analysis was conducted to determine the effect of the program on BP measurements taken in the clinical setting. The primary outcomes of interest were change in mean BP measurement and the percentage of patients who had controlled hypertension at follow‐up. Because enrollment into the program was on a rolling ongoing basis, only those who had been enrolled at least 9 months prior to the start of our data collection were included in this statistical analysis. Change in BP was calculated as the difference between baseline and follow‐up systolic and diastolic office BP measurements. Outcomes were also analyzed by site. The percentage with hypertension controlled by age, race/ethnicity, and sex subcategories was calculated, and statistical differences were assessed using t tests. Distributions of age, sex, and race/ethnicity of those who were controlled vs uncontrolled were compared using χ2 tests. We created a second dataset to conduct a sensitivity analysis by imputing the baseline office BP measurement as follow‐up BP measurement for the 751 participants who were enrolled but were lacking a final measurement at 7 to 11 months, adding them to the primary dataset of those with complete data at 7 to 11 months. Imputation in this way provides conservative estimates of BP change and percent with hypertension controlled, with the assumption that there is no change in BP measurement due to the intervention in those who did not return within the specified observation time frame. We chose not to use the imputed dataset for primary data analysis because the goal of this study is to understand the impact of this evaluation on patients as they are seen by providers. Results from our primary and imputed dataset were further adjusted for regression to the mean (RTTM) using previously described methods 11 , 12 and additionally reported in the current manuscript. All analyses were performed using Stata version 8.2 (College Station, TX).
The program evaluation protocol was reviewed by the NYC Department of Health and Mental Hygiene institutional review board and was determined to be exempt research. Sixteen of the 20 sites used were covered under the Department of Health and Mental Hygiene institutional review board, while 4 sites had independent institutional review board review and approval.
Results
A total of 20 ambulatory care clinics across 13 health care facilities participated in this collaboration. Nine were hospital‐based clinics or diagnostic treatment centers that are part of the public health care system in New York City, 9 were free‐standing clinics or hospital‐affiliated clinics, and 2 were federally qualified health centers. Of the 20, 18 were primary care clinics and 2 were nephrology subspecialty clinics. The latter were included in conjunction with the co‐located primary care clinic because the subspecialty clinics were already part of the existing clinics’ team management arrangement for patients with uncontrolled hypertension.
Of the 1616 patients enrolled, 98 were removed from this analysis because they: (1) did not have an adequate period of observation (n=46), (2) had missing BP data at enrollment (n=1), or had been errantly enrolled (ie, had SBP of <130 mm Hg and DBP <80 mm Hg at baseline; n=51). Of the remaining 1518 participants with baseline data, a total of 751 participants did not have follow‐up measurements, leaving 767 (50.5% of 1518) participants with both baseline and follow‐up BP measurements (Figure). Compared with those with follow‐up data available, participants who were missing follow‐up data and, thus, excluded from the main analysis were more likely to be Hispanic, black, or white and not in the “other” race category (among those missing follow‐up data: 3.5% other race; among those with follow‐up data available: 6.7% other race; P=.04 for χ2 test) and male (among those missing follow‐up data: 38.7% men; among those with follow‐up data available, 31.2% men; P<.01 for χ2 test).
Figure FIGURE.
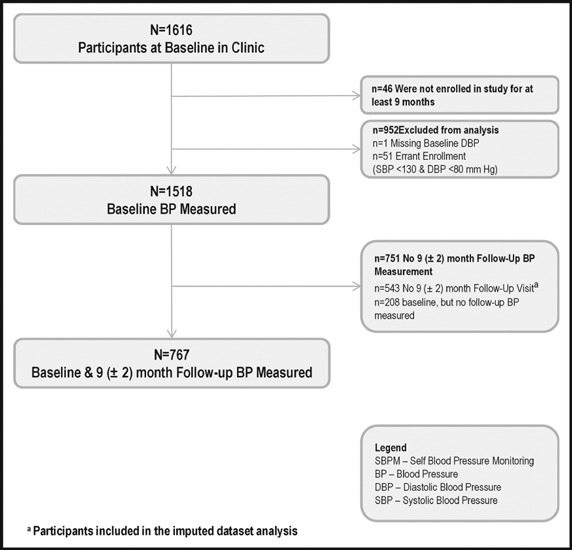
Participant flow. BP indicates blood pressure; DBP, diastolic blood pressure; SBP, systolic blood pressure.
Mean age of participants was 58.7±12.9 years. Participants were predominantly 45 to 64 years of age (50.6%), black (51.2%), and female (68.6%) (Table I). Mean office baseline SBP and DBP measurements were 156.7±18.9 mm Hg and 87.2±12.3 mm Hg, respectively (Table II). Office SBP and DBP measurements decreased a mean of 18.7 mm Hg and 8.5 mm Hg, respectively. After adjustment for RTTM, these results were attenuated at follow‐up but remained significant (adjusted SBP and DBP measurement decreased, respectively, 9.0 mm Hg and 3.4 mm Hg, P<.01 for both). At follow‐up, 52.5% had controlled hypertension. These results did not vary widely when stratified by health care facility, with a range of hypertension control from 41.1% to 70.8% (results not shown). Hypertension control at follow‐up was more likely among those aged 45 to 64 compared with those aged 18 to 44, but otherwise did not differ by age, race/ethnicity, or sex (Table III). Participants who achieved BP control at follow‐up did not differ from those who did not achieve control by age (P for χ2=0.06), race/ethnicity (P for χ2=0.20), or sex (P for χ2=0.07).
Table I.
Characteristics of Participants at Baseline and at 9 (±2)‐Month Follow‐Up Clinic Visit (n=767)
| Participant Characteristics, No. (%) | Mean Baseline Blood Pressure, mm Hg | ||
|---|---|---|---|
| Systolic | Diastolic | ||
| Overall | 767 (100) | 156.7±18.9 | 87.2±12.3 |
| Age group, y, No. (%) | |||
| 18–44 | 110 (14.3) | 151.7±17.3a,b | 93.5±10.5a,b |
| 45–64 | 388 (50.6) | 155.7±18.0b | 88.9±11.8b |
| ≥65 | 263 (34.3) | 159.5±20.3 | 82.2±11.9 |
| Race, No. (%) | |||
| Hispanic | 274 (35.7) | 156.7±18.7c | 87.5±11.4c |
| Black | 393 (51.2) | 157.5±19.6c | 87.8±13.0c |
| White | 20 (2.6) | 154.3±17.5 | 87.6±8.5c |
| Other | 49 (6.4) | 148.4±13.7 | 81.3±11.9 |
| Sex, No. (%) | |||
| Male | 238 (31.0) | 155.8±16.9 | 88.7±12.4d |
| Female | 526 (68.6) | 156.7±19.7 | 86.5±12.3 |
a P<.05 compared with age group 45 to 64 years. b P<.05 compared with age group 65 years and older. c P<.05 compared with “other” race group. d P<.05 compared with female sex. All other comparisons were nonsignificant. Missing data on age (n=6), race (n=31), or sex (n=3); therefore, percentages do not add up to 100%.
Table II.
Baseline and Follow‐Up SBP and DBP, Changes, and Percent Controlled
| Baseline BP, mm Hg, mean ± SD | Follow‐Up BP, mm Hg, mean ± SD | Change in SBPa | P Value | Change in DBPa | P Value | Controlledb,n (%) | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. | SBP | DBP | SBP | DBP | ||||||
| Primary Dataset | 767 | 156.7±18.9 | 87.2±12.3 | 137.7±19.2 | 78.7±12.2 | −18.7 | <.01 | −8.5 | <.01 | 403 (52.5) |
| Adjustment for RTTM | −9.0 | <.01 | −3.4 | <.01 | NA | |||||
| Imputed Dataset | 1518 | 157.5±19.2 | 88.2±12.6 | 148.1±22.0 | 83.9±13.6 | −9.5 | <.01 | −4.3 | <.01 | 462 (30.4) |
| Adjustment for RTTM | −8.8 | <.01 | −3.1 | <.01 | NA | |||||
Abbreviations: DBP, diastolic blood pressure; NA, not applicable; RTTM, regression to the mean; SBP, systolic blood pressure; SD, standard deviation. The primary dataset includes those with baseline and follow‐up data completed. The imputed dataset adds to the primary those with imputed follow‐up data due to missing data at 7 to 11 months. aChange=Follow‐up BP − Baseline BP. bOffice‐controlled BP defined as SBP <140 mm Hg AND DBP <90 mm Hg.
Table III.
Factors Associated With Control Defined by Office BP, n=767
| No. | Controlled, No. (%)a | P Value | |
|---|---|---|---|
| Age group, y | |||
| 18–44 | 110 | 50 (45.4) | Reference |
| 45–64 | 388 | 220 (56.7) | .04 |
| ≥65 | 263 | 132 (50.2) | .40 |
| Race | |||
| Hispanic | 274 | 143 (52.2) | .81 |
| Black | 393 | 194 (49.4) | .62 |
| White | 20 | 11 (55.0) | Reference |
| Other | 49 | 32 (65.3) | .42 |
| Sex | |||
| Male | 238 | 136 (57.1) | Reference |
| Female | 526 | 264 (50.2) | .07 |
aControlled blood pressure (BP) defined as systolic BP <140 mm Hg AND diastolic BP <90 mm Hg at follow‐up.
Reductions were attenuated but remained significant with the addition of 751 participants with imputed values for missing follow‐up BP data at 7 to 11 months. In this larger sample (n=1518), decrease in BP was 9.5 mm Hg SBP and 4.3 mm Hg DBP (P<.01 for both). After adjustment for RTTM, SBP decreased by 8.8 mm Hg (P<.01) and DBP decreased by 3.1 mm Hg (P<.01). The percentage of total participants with controlled BP in this larger dataset was 30.4%.
Process Evaluation
All 20 clinical sites participated in the key‐informant interviews, with a total of 13 participants. In some instances, a single key informant responded on behalf of multiple sites because they were part of the same network.
A majority of clinics reported integrating patient recruitment into the general clinic flow during check‐in for regular clinic visits, but 3 clinics identified eligible patients in subspecialty ambulatory care hypertension clinics or prior to the patients’ arrival for appointments. These clinics “prescreened” potentially eligible patients and flagged their records prior to the scheduled visit. Most sites trained patients on SBPM use during the course of their regular visit and relied heavily on nurses and health educators for this task. Two sites, however, scheduled specific patient training sessions conducted by allied health staff such as lay health promoters, and one site enrolled most of its patients through a single provider. Regardless of training methods, the reported time needed to train patients on SBPM ranged from 10 to 30 minutes. Six clinics reported a negative impact on clinic work flow, 12 reported no impact or were neutral, 1 reported a positive impact, and 1 did not respond.
A majority of clinics reported being able to track and collect follow‐up BP measurements during regularly scheduled office visits, but this activity was noted to be challenging for 15 clinics. Several methods of identifying participating patients during their regular visits were employed, including using stickers on charts or clinic cards and referring back to the clinic tracking log. Approximately one third relied on providers remembering that the patient was enrolled at the time of the visit. All key informants reported both using the home BP measurements in their patients’ clinical management and finding SBPM a useful component of hypertension management.
Discussion
Approximately half of the nearly 800 participants with uncontrolled hypertension at baseline achieved control by 7 to 11 months of SBPM. Although the extent varied to some degree by clinic, the achievement of hypertension control was seen in all subgroups and remained robust even after adjustment for RTTM and with imputation to include participants missing follow‐up values. This is a noteworthy finding, given that eligibility criteria intentionally sought to include only patients with difficult‐to‐control BP, ie, those whose BP was not well controlled through traditional medical management. Specifically, eligible patients had elevated BP on enrollment and in the previous visit, as well as a diagnosis of hypertension for >6 months. Further, control rates at follow‐up did not vary by race, suggesting that the use of SBPM may have a role in addressing persistent race/ethnic disparities in BP control.
“Explanatory” studies are designed to measure the efficacy of an intervention under specialized conditions. In contrast, “pragmatic” trials measure effectiveness of a treatment under regular practice conditions with typical patients. 13 Findings from our pragmatic study were consistent with those from randomized controlled clinical trials. 7 , 8 , 9 While pragmatic study design does not preclude the use of a separate control group, in our case, such a design would have interrupted the real world conditions we sought to examine, and would have made inclusion of specific clinic locations and, thus, their populations, extremely challenging. Results from pragmatic studies are relevant to outcomes research and an increased focus on patient‐centered care; however, they are less robust compared with findings from randomized controlled trials. With respect to study design to assess change in BP, one important consideration is RTTM, which is a statistical phenomenon that occurs independent of clinical intervention. Here, RTTM can be defined as “the tendency of BP measurements of a group of persons selected on the basis of the above average values to be lower on rescreening or follow‐up even without an intervening hypertension control program,” and arises because “the baseline BP is also used as a selection criterion for initiating active BP control.” 12 The presence of a separate control group in a study helps to mitigate the effect of RTTM, in addition to addressing other potential study biases; however, as noted, control groups are not always easily incorporated into pragmatic study design. For more valid results, we used the technique of adjusting for RTTM to account for some of the bias that can occur in the absence of a control group, and still found statistically significant and, likely, clinically relevant outcomes. To our knowledge, ours is one of the few published studies to account for this statistical phenomenon in this type of study design. While we acknowledge that this adjustment does not fully account for the design limitations of a pre‐post analysis, we conclude that analytic techniques that enhance findings from pragmatic studies with less robust study designs should become the norm.
Study Strengths
Our study suggests that incorporating SBPM into the management of hypertension is feasible and worthwhile. We found that clinics of varying sizes and resource levels were able to successfully implement the SBPM program, even in busy settings. Secular increases in the use of electronic medical records may facilitate this process in the future and alleviate the most commonly noted implementation challenge reported by clinics, collection of follow‐up data from patients using SBPM during their regular clinic visits. Embedding patient tracking systems within a traditional electronic health record could increase the uniformity of patient identification, simplify follow‐up, and facilitate targeted clinician response for patients whose BP remains uncontrolled.
Even when clinics have the capacity to implement evidence‐based interventions, the active uptake of beneficial interventions requires systematically addressing barriers at the patient and provider level. Our study overcame the patient barrier of cost by providing BP monitors for free. For broader implementation, however, a careful investigation of existing insurance policies related to coverage of monitors is needed.
To overcome practice barriers, our study illustrates the value of a local health department in disseminating and evaluating clinic‐based activities, with the potential to address health disparities. Translation of relevant clinical study findings into provider practice has been, and remains, an important function of public health. Federal agencies, such as the National Heart Lung and Blood Institute and Centers for Disease Control and Prevention, as well as state and local health departments, promote guidelines for screening and treatment and provide technical assistance in the prevention and control of various diseases. 14 , 15 , 16 , 17 Collaborations between local health departments and primary care clinics have great potential to promote effective treatment approaches that have yet to be widely adapted and disseminated.
Study Limitations
Our study has several limitations. While we corrected for RTTM, the lack of a prospective control group meant that we were unable to account for secular trends in hypertension control or account for potential selection bias. We do not expect secular trends to have had a great impact on our findings; the study reporting period was only up to 11 months. It is possible that patients with higher motivation may have been preferentially referred or self‐selected to participate in the program. In general, this bias would tend to overestimate the “true” effect of the intervention in the research population, although it does not likely distort the impact of the intervention under normal clinical conditions, where more motivated patients are more likely to engage with the provider and adhere to recommendations. Another limitation of this analysis is the lack of information on the diagnosis of diabetes or chronic kidney disease, precluding the ability to calculate control rates among patients with these conditions (for whom BP control is defined by lower systolic and diastolic values) and potentially leading to a small overestimation of impact. Thus, the value we present may be an overestimate of BP control for the study sample overall and for those with these conditions.
Conclusions
Despite these limitations, our results support broader efforts to integrate SBPM into the routine clinical management of uncontrolled hypertension. Our collaborative method provides a model in which public health agencies initiate development of a specific clinical initiative, identify clinical partners in high‐priority communities, and provide content expertise and technical assistance to support roll‐out in these limited‐resource settings.
Note: For contact purposes only, Dr. Angell’s affiliation is currently with the Centers for Disease Control and Prevention.
References
- 1. Gillespie C, Kuklina EV, Briss PA, Blair NA, Hong Y. Vital Signs: Prevalence, Treatment, and Control of Hypertension – United States, 1999–2002 and 2005–2008. http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6004a4.htm. Accessed June 27, 2011.
- 2. Wang TJ, Vasan RS. Epidemiology of uncontrolled hypertension in the United States. Circulation. 2005;112:1651–1662. [DOI] [PubMed] [Google Scholar]
- 3. Egan BM, Zhao Y, Axon RN. US trends in prevalence, awareness, treatment, and control of hypertension, 1988–2008. JAMA. 2010;303:2043–2050. [DOI] [PubMed] [Google Scholar]
- 4. Fiscella K, Holt K. Racial disparity in hypertension control: tallying the death toll. Ann Fam Med. 2008;6:497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Farley TA, Dalal MA, Mostashari F, Frieden TR. Deaths preventable in the US by improvements in use of clinical preventive services. Am J Prev Med. 2010;38:600–609. [DOI] [PubMed] [Google Scholar]
- 6. Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206–1252. [DOI] [PubMed] [Google Scholar]
- 7. Agarwal R, Bills JE, Hecht TJW, Light RP. Role of home blood pressure monitoring in overcoming therapeutic inertia and improving hypertension control. A systematic review and meta‐analysis. Hypertension. 2011;57:29–38. [DOI] [PubMed] [Google Scholar]
- 8. Cappuccio FP, Kerry SM, Forbes L, Donald A. Blood pressure control by home monitoring: meta‐analysis of randomised trials. BMJ. 2004;329:145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Glynn LG, Murphy AW, Smith SM, et al. Self‐monitoring and other non‐pharmacological interventions to improve the management of hypertension in primary care: a systematic review. Br J Gen Pract. 2010;60:e476–e488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Pickering TG, Miller NH, Ogedegbe G, et al. Call to action on use and reimbursement for home blood pressure monitoring: a joint scientific statement from the American Heart Association, American Society of Hypertension, and Preventive Cardiovascular Nurses Association. Hypertension. 2008;52:10–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Mee R, Chua T. Regression toward the mean and the paired sample t test. Am Stat. 1991;45:39–42. [Google Scholar]
- 12. Shepard DS, Finison LJ. Blood pressure reductions: correcting for regression to the mean. Prev Med. 1983;12:304–317. [DOI] [PubMed] [Google Scholar]
- 13. Roland M, Torgerson DJ. What are pragmatic trials? BMJ. 1998;316:285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Centers for Disease Control and Prevention: WISEWOMAN. http://www.cdc.gov/wisewoman/. Accessed July 26, 2011.
- 15. About ALLHAT/JNC7 Dissemination – ALLHAT Clinical Trial. http://allhat.uth.tmc.edu/Health/DissAbout.aspx?SubSite=Hlth. Accessed July 26, 2011.
- 16. Wrobel MJ, Figge JJ, Izzo JL Jr. Hypertension in diverse populations: a New York State Medicaid clinical guidance document. J Am Soc Hypertens. 2011;5:208–229. [DOI] [PubMed] [Google Scholar]
- 17. Antman EM, Hand M, Armstrong PW, et al. 2007 Focused update of the ACC/AHA 2004 Guidelines for the Management of Patients with ST‐Elevation Myocardial Infarction. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2008; 51:210–247. [DOI] [PubMed] [Google Scholar]


