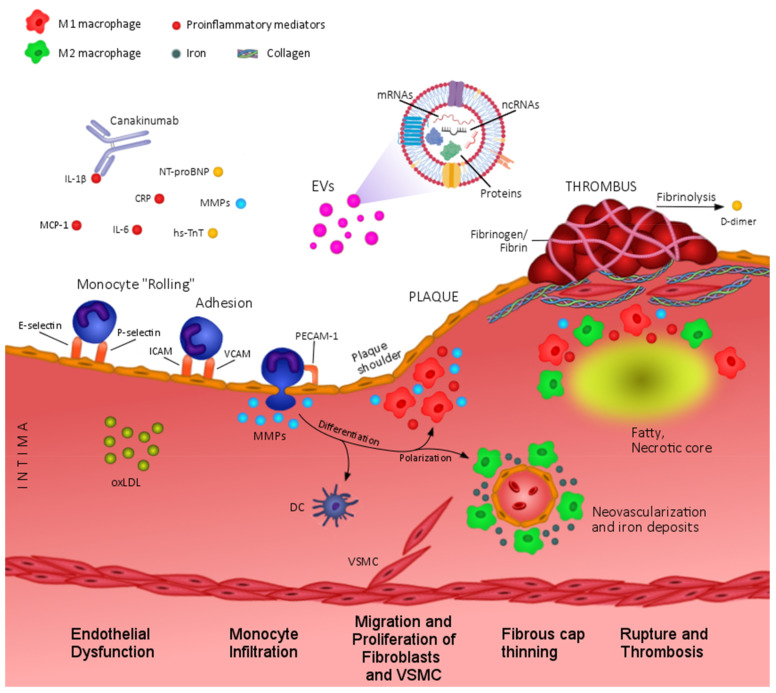
Figure 1.
Circulating biomarkers in atherosclerosis and PAD pathophysiology. At early stages of atherosclerosis, endothelial dysfunction leads to increased levels of proinflammatory cytokines (IL1β, IL6, CRP, MCP-1), extracellular vesicles (EVs), proteases (MMPs), and adhesion molecules (E-selectin, P-selectin, ICAM, VCAM,) that contribute to monocyte recruitment and infiltration into the intima. Microenvironmental factors such as MMPs orchestrate plaque progression by regulating macrophage polarization towards proinflammatory (M1) or anti-inflammatory (M2) phenotypes, which are predominantly located in unstable areas (i.e.,: plaque shoulder) or neovascularization regions, respectively. In advanced lesions, inflammatory factors and MMPs exacerbate fibrous cap thinning and contribute to plaque instability, rupture, and formation of fibrin clot. Extracellular vesicles (EVs), mainly of platelet origin, also participate in thrombus formation according to the exposure of procoagulant factors (e.g.,: tissue factor and phosphatidylserine). In addition, reduced tissue perfusion due to arterial stenosis and thrombosis might cause increased levels of tissue damage-related biomarkers such as NT-proBNP or hs-TnT. CRP, C reactive protein; DC, dendritic cells; ICAM, intercellular adhesion molecule; IL, interleukin; MCP-1, monocyte chemoattractant protein; MMPs, matrix metalloproteinases; NT-proBNP, N-terminal pro-brain natriuretic peptide; oxLDL, oxidized Low Density Lipoproteins; hs-TnT, high sensitivity troponin T; VCAM, vascular cell adhesion molecule; VSMC, vascular Smooth Muscle Cells.