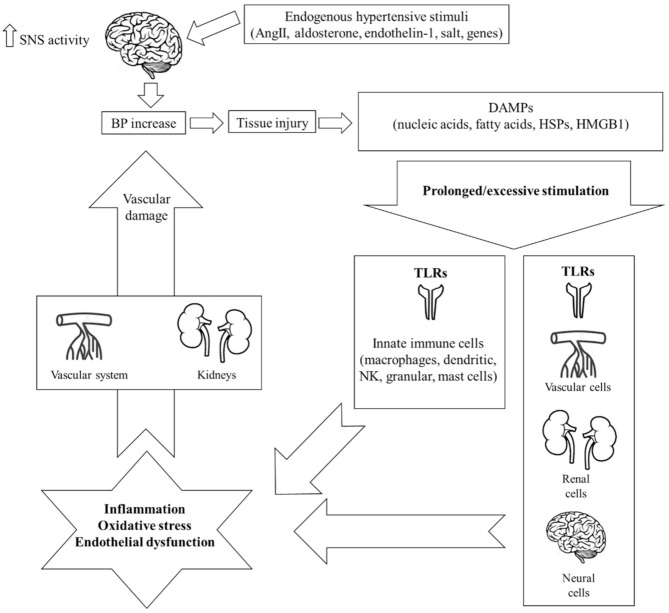
Figure 1.
Schematic representation of the mechanisms of innate immunity implicated in the pathogenesis of hypertension. Endogenous stimuli including angiotensin II (AngII), aldosterone, endothelin-1, salt, and several genes initially increase central nervous signaling and thus sympathetic nervous system (SNS) activity, which, in turn, provokes a slight elevation in blood pressure (BP). This event leads to tissue injury and the release of endogenous intra- or extracellular molecules including cell-derived nucleic acids, fatty acids, heat shock proteins (HSPs), and high-mobility group box-1 (HMGB1), all termed damage-associated molecular patterns (DAMPs). In the hypertensive environment, an excessive or prolonged DAMP-mediated stimulation of innate immunity leads to an aberrant immunologic response through the activation of toll-like receptors (TLRs). The result is chronic low-grade inflammation, oxidative stress, and endothelial dysfunction, all of which inflict damage on the kidneys and the vascular system, thus further increasing BP. Importantly, increased TLR expression and subsequent activation has been documented not only on immune but also on non-immune cells of the central nervous, renal, and vascular system, all major contributors in the pathogenesis of hypertension.