Figure 2. New health decision model schematic: Universal natural history of cervical carcinogenesis.
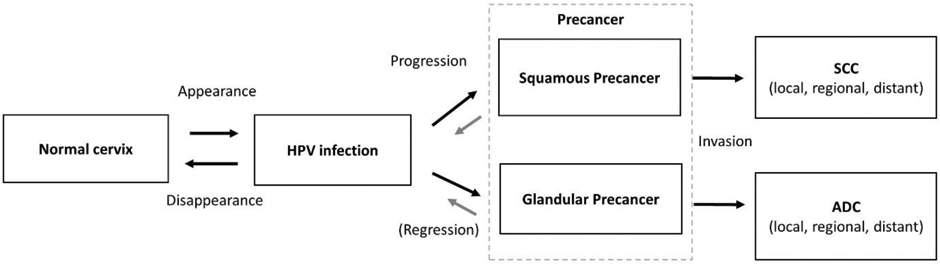
Each box represents a necessary stage, or health state, on the path to cervical cancer, including acquisition of a carcinogenic, “high-risk” HPV infection; progression of a persistent hrHPV infection to precancer (defined as persistent lesions with a high likelihood of invasion if left untreated); and invasion to cervical cancer. Each arrow represents the risk of transitioning between stages. Appearance— the risk of transitioning from No HPV infection to HPV infection— may include new acquisition of a particular genotype, re-infection with the same genotype, or reactivation of a latent infection. Disappearance— the risk of transitioning from HPV infection to No HPV infection— refers to the shift from a would-be detectable infection to non-detectable by a clinical HPV DNA assay, whether attributable to complete viral clearance or viral latency. The model distinguishes progression to squamous precancer (which may transition to squamous cell carcinoma) from progression to glandular precancer (which may transition to adenocarcinoma). Precancer occurs when a hrHPV infection that is primarily a productive infection (i.e., producing more viral particles) becomes instead an abortive transforming infection (i.e., associated clone of cells with severe disruption of cellular growth and differentiation controls, decreased programmed cell death [apoptosis] and increased genetic mutability). Regression of precancer through immune recognition and cell-mediated immune control is still possible, but much less likely than the control of earlier productive infections. The probability of invasion of a precancer is a function of time and the accumulation of genetic changes needed to overcome the coded cellular safeguards against growth inward into the cervical stroma across the epithelial basement membrane. Although invasion can occur quickly in unfortunate, but rare occurrences, precancers typically grow circumferentially within the epithelial layer for years if not decades before acquiring an invasive phenotype. Multiple precancers can occur on a cervix. If any invades, cancer results.
