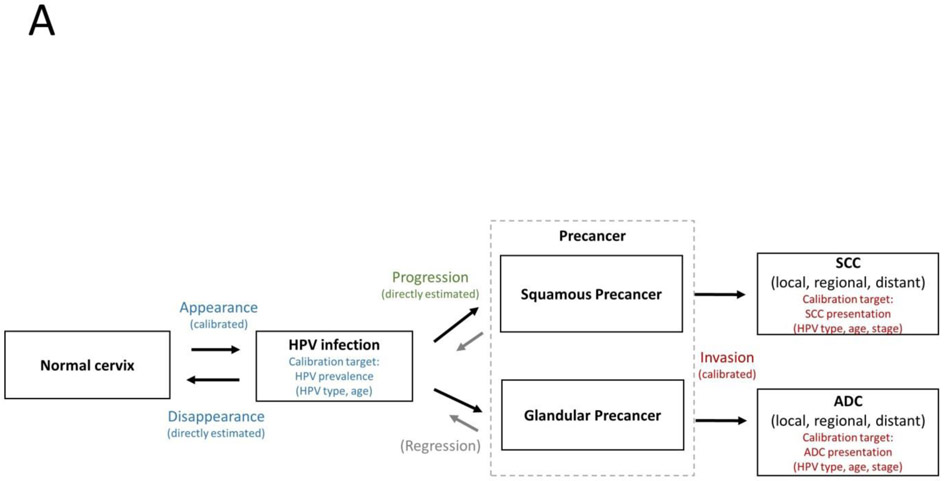
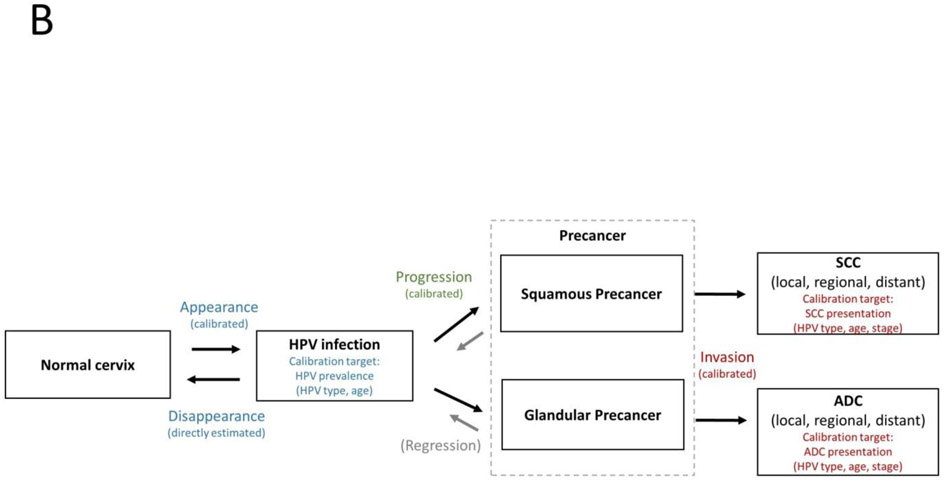
Figure 4. Direct estimation versus calibration of transition probabilities.
In the Lower HPV Prevalence Model (A), data are available to directly estimate transition risks for disappearance and progression from longitudinal studies. We assume these risks are consistent across Lower HPV Prevalence populations. The transition risks for appearance vary according to sexual behavior in a population, and can only be directly estimated when population-based longitudinal data are available. Thus, in most cases, the risk of appearance is calibrated to fit HPV prevalence (by genotype and age) while using direct estimates for disappearance. We will explore the impact of individual-level frailty and how it may impact clustering of infections appearing within a woman (due to sexual behavior or immune factors). We assume the risk of disappearance is the same whether an infection was newly acquired or reactivated.
In the Higher HPV Prevalence Model (B), data will soon be available from longitudinal studies to directly estimate transition risks for disappearance. We assume these risks are consistent across Higher HPV Prevalence populations with a low burden of HIV. As in Lower HPV Prevalence settings, direct estimates for the risk of appearance are rarely available, so this transition risk will be calibrated to fit HPV prevalence while using direct estimates for disappearance. Due to limited data, direct estimates for progression risks in Higher HPV Prevalence settings are not available. We are exploring the relationship between the prevalence of precancer among women with hrHPV in Lower and Higher HPV prevalence settings to determine whether progression risks (conditional on hrHPV infection) are similar to Lower HPV Prevalence settings or would need to be calibrated.
In both the Lower and Higher HPV Prevalence models, the risk of invasion is unobserved for ethical reasons, and must be calibrated to fit cancer presentation data for squamous cell carcinoma and adenocarcinoma (by HPV genotype, age and stage at presentation prior to widespread screening). Whether the risk of invasion is initially calibrated in a Higher HPV Prevalence setting (where screening may be less widespread and HPV prevalence patterns may better reflect sexual behavior patterns among more recent cohorts) or a Lower HPV Prevalence setting (where more data are available to directly estimate progression risk and prevalence of precancer), we anticipate holding the risk of invasion constant between models, as we hypothesize that this transition does not change as a function of cell-mediated immunity.
The HIV Model is not shown, as it is not yet clear which transition risks can be directly estimated versus calibrated.