Abstract
Background
Vaccination against coronavirus disease 2019 (COVID-19) has become an important public health solution. To date, there has been a lack of data on COVID-19 vaccination willingness, vaccine hesitancy, and vaccination coverage in China since the vaccine has become available.
Methods
We designed and implemented a cross-sectional, population-based online survey to evaluate the willingness, hesitancy, and coverage of the COVID-19 vaccine among the Chinese population. 8742 valid samples were recruited and classified as the vaccine-priority group (n = 3902; 44.6%) and the non-priority group (n = 4840; 55.4%).
Results
The proportion of people’s trust in the vaccine, delivery system, and government were 69.0%, 78.0% and 81.3%, respectively. 67.1% of the participants were reportedly willing to accept the COVID-19 vaccination, while 9.0% refused it. 834 (35.5%) reported vaccine hesitancy, including acceptors with doubts (48.8%), refusers (39.4%), and delayers (11.8%). The current coverage was 34.4%, far from reaching the requirements of herd immunity. The predicted rate of COVID-19 vaccination was 64.9%, 68.9% and 81.1% based on the rates of vaccine hesitancy, willingness, and refusal, respectively.
Conclusions
The COVID-19 vaccine rate is far from reaching the requirements of herd immunity, which will require more flexible and comprehensive efforts to improve the population’s confidence and willingness to vaccinate. It should be highlighted that vaccination alone is insufficient to stop the pandemic; further efforts are needed not only to increase vaccination coverage but also to maintain non-specific prevention strategies.
Keywords: Vaccination, Willingness, Vaccine hesitancy, Confidence, COVID-19 vaccine
1. Introduction
Coronavirus disease 2019 (COVID-19) has caused huge losses to the world. As of January 30, 2021, the cumulated number of confirmed COVID-19 cases worldwide has exceeded 100 million, with the death total exceeding 2 million [1]. The development of a safe and effective vaccine against COVID-19 is expected to be the long-term solution to control the pandemic. As of January 29, 2021, there are over 292 COVID-19 vaccine candidates globally, of which more than 70 have entered clinical evaluation [2]. The China State Food and Drug Administration licensed the Sinopharm’s inactivated COVID-19 vaccine for marketing with conditions on December 30, 2020 [3], and the Sinovac’s inactivated COVID-19 vaccine for marketing with conditions on February 05, 2021; in addition, four other vaccines have entered phase III clinical trials and are expected to be approved in the near future [3]. From June to November 2020, over 1.5 million emergency vaccine doses of COVID-19 were distributed among the high-risk population in China [3]. In addition, the vaccination of employees of nine high-risk occupations was initiated on December 15, 2020 [4]. By February 3, 2021, over 31 million COVID-19 vaccination doses have been administered in total [5].
The effectiveness of the COVID-19 vaccine in controlling the pandemic depends on the coverage of vaccination in the population. Adequate uptake of the COVID-19 vaccine ensures protection for the vaccinated population and has the potential to stop the pandemic by generating herd immunity, thereby protecting everyone [6]. Thus, high vaccination coverage is the key to controlling the COVID-19 pandemic; when setting the R0 of COVID-19 to 3.0, it was estimated that at least 67% of the population needs to be vaccinated [7]. At the beginning of the Wuhan COVID-19 outbreak, the R0 was estimated to be between 2.2 and 5.7, indicating the necessary coverage of vaccination should be at least 55% [8]; Rt can be changed if active surveillance, contact tracing, quarantine, and early strong social distancing efforts have been taken [9]. However, these estimations were based on the condition of 100% COVID-19 vaccine efficacy; higher vaccination coverages are needed to ensure pandemic control because the efficacy of the current COVID-19 vaccines is <80% (79.34% for Sinopharm’s vaccine and 50% for Sinovac’s vaccine) [10], [11].
Vaccination willingness and vaccine hesitancy are the key factors for vaccination coverage. A nationally representative survey in the United Kingdom reported 27% were hesitant and 9% resistant to accepting the COVID-19 vaccination [12]. In Canada, 19% reported somewhat likely, 9% unknown, and 14% unlikely to get the COVID-19 vaccine when available [13]. Many adverse events following immunization have occurred in the past, which have significantly decreased the public’s confidence in vaccines in China [14], [15]. In addition, its short development duration, less public awareness, and adverse events reported both domestically and abroad may contribute to vaccine hesitancy to the COVID-19 vaccine [16]. To date, there has been a lack of data on COVID-19 vaccination willingness, vaccine hesitancy, and vaccination coverage in China since the vaccine has become available. This information is urgently needed to understand the current vaccination situation and facilitate vaccination in a more efficient way. Therefore, at the beginning of the COVID-19 vaccination in China, we designed an online questionnaire to evaluate vaccination willingness, vaccine hesitancy, and vaccination coverage to provide evidence on vaccination strategies.
2. Methods
2.1. Study design
We conducted a cross-sectional, population-based online survey among the Chinese population using a structured questionnaire from January 10 to January 22, 2021. It was an open online survey for all the population aged 18 to 60 years residing in China. Those willing to respond could complete the questionnaire by mobile phone or computer. The online survey was prompted through primary social networks, including WeChat and Weibo. Participants could complete the survey questionnaire, which took approximately three minutes on average, either by mobile phone or computer. Data was collected on Wen Juan Xing, an online platform providing functions equivalent to Amazon Mechanical Turk, Qualtrics, SurveyMonkey or CloudResearch, which provides online questionnaire design and survey functions. Importantly, its personal identification function allows for an authentic, diverse and representative sample.
2.2. Data collection
The structured questionnaire contained information on demographic characteristics, the status of COVID-19 vaccination, willingness to accept the COVID-19 vaccination, vaccine confidence, and vaccine hesitancy (Supplemental Table 1).
We collected demographic characteristics, including gender, age, education, residence, and occupation. According to the guidelines of National Health Commission of China, employees of specific occupations were set to be priority vaccination population, including medical employees, government or Social order, public service, going abroad, transportation and port affairs or customs, which was as the priority group. Participants of other occupations were classified as non-priority group. Participants’ geographic information was obtained from the associated IP address. Five questions were related to information on the COVID-19 vaccination.
2.3. Vaccine confidence
Vaccine confidence was considered to be one of the important influencing factors to vaccination. We collected three dimensions of vaccine confidence, including vaccine trust, delivery system trust, and government trust through seven items, according to the recommendation from the World Health Organization Strategic Advisory Group of Experts on Immunization [17], [18]. Trust in the COVID-19 vaccine was measured by the extent to which the population agreed with the vaccine’s importance, effectiveness, and safety. Trust in the delivery system was measured according to the confidence in healthcare providers, professional institutions, and vaccine manufacturers. Total scores on trust in vaccine and trust in delivery system ranged from 3 to 9 and were categorized into agree (trust score ≥ 5) and disagree (trust score ≤ 4). Trust in the government was measured through one question, which was scored as agree, not sure, or disagree directly, and categorized into agree and disagree (including not sure and disagree). Vaccination confidence was based on the score of the three dimensions as a whole, which ranged from 7 to 21.
2.4. Vaccination willingness
Vaccination willingness to COVID-19 was measured by the question “To what extend you want to take the COVID-19 vaccine?” and scored as eager, intend to, not sure, unwilling, and absolutely no. The responses to willingness to accept COVID-19 vaccination were classified into three categories: willing (eager and intend to), not sure and unwilling (unwilling and absolutely no).
2.5. Vaccine hesitancy
Vaccine hesitancy was defined as hesitant, delayed, or refusal to accept the vaccine due to reasons other than vaccine availability or contraindication. It was measured among the priority population for this study since the non-priority population had no access to the COVID-19 vaccine at this stage. Vaccine-priority participants were categorized as acceptors with no hesitancy, acceptors with doubt, delayers, or refusers, and the last three categories were considered as vaccine hesitancy.
2.6. Quality control
We monitored the progress of the survey every day. After the deadline, we checked the accuracy of the data. A quality control question (What year is this year?) was set for detecting inattentive samples. Answers from duplicate IP addresses were recruited by the first record, and the following records were excluded. Moreover, questionnaires would be excluded if (1) the IP addresses were outside the mainland of China, or (2) there were logical contradictions between the answers to the questionnaire.
2.7. Statistical analysis
Categorical variables are expressed as absolute and relative frequencies in different groups, and the differences in their distribution were tested by the Chi-square test. Age was re-classified into four categories according to the distribution, including 18–29 years, 30–39 years, 40–49 years, and ≥50 years. The multivariate logistic regression model was used to explore the factors associated with confidence and vaccine hesitancy. The ordinal logistic regression model was used to explore the factors associated with vaccination willingness. The odds ratio (OR) and 95% confidence interval (CI) were calculated. We predicted the possible overall COVID-19 vaccination rates in the mainland of China, which were directly estimated by the standardized method using the observed rates of vaccine hesitancy, willingness, and refusal in the study on the basis of 26 subgroups by age and gender. Briefly, 12 subgroups of patients were classified by age groups (18–19, 20–24, 25–39, 40–44, 45–59, 50–54, 55–59, 60–64, 65–69,70–74 and >75 years old) and gender (male and female). Population data at the prefecture (city) level in 2017 were obtained from the National Bureau of Statistics of the People’s Republic of China. SPSS (version 22.0, IBM, Armonk, NY, USA) was used for data cleaning and statistical analysis. Spatial data analyses were conducted using ArcGIS (version 10.7, ESRI Corp, Redlands, CA, USA). The significance level was considered when P value was <0.05.
2.8. Ethical approval
This study was approved by Peking University Institutional Review Board (IRB00001052-21001); exemption for informed consent was granted.
3. Results
3.1. Study participants and characteristics
In total, 9508 out of 9531 respondents completed the questionnaires, with a response rate of 99.6%. Among them, 667 were excluded due to IP addresses that were duplicated or outside the mainland of China, 78 were excluded due to a quality issue, and 21 were excluded because of logical error. Finally, 8742 questionnaires underwent data analysis, with the valid response rate of 91.7%.
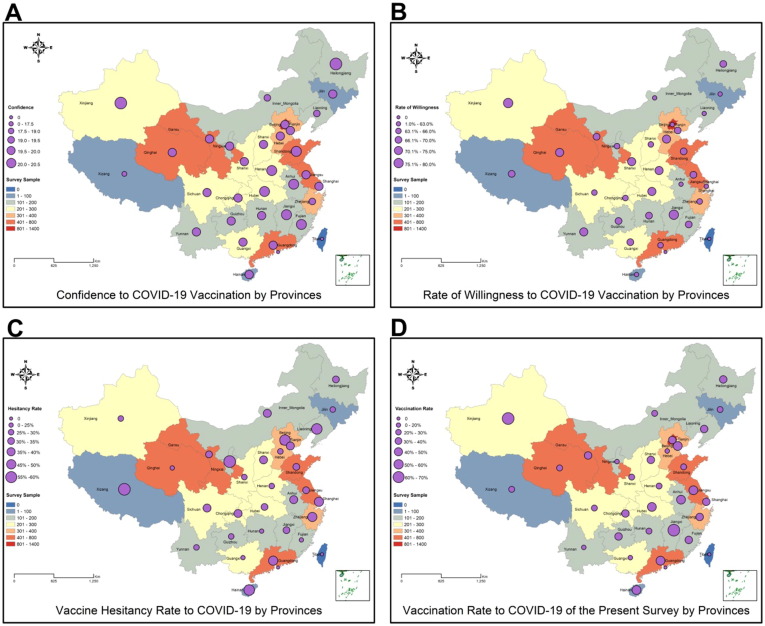
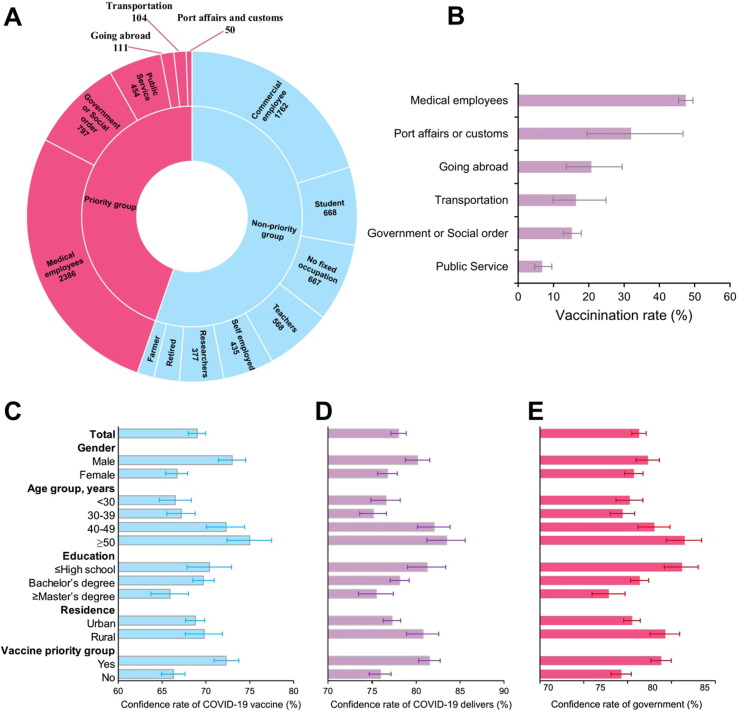
The participants were from 31 provinces in the mainland of China, and the top three provinces were Beijing (1321, 15.1%), Qinghai (714, 8.2%), and Guangdong (506, 5.8%) (Fig. 1 ). Among the participants, 3207 (33.6%) were male, and 3277 (37.5%) were aged 30–39 years (Table 1 ). About 63.5% participants had a bachelor’s degree, and 78.9% were from urban areas. 3902 (44.6%) were classified in the vaccine-priority group, and 4840 (55.4%) were in the non-priority group (Fig. 2 A). Among the vaccine-priority group, medical employees showed the highest proportion (84.5%) of vaccination among occupations (Supplemental Table 2). Data from the Population and Employment Statistical Yearbook of China, 2017, showed that males occupied 51.2% of the total population. And participants aged 18–29, 30–39, 40–49 or 50–60 occupied 28.4%, 22.4%, 26.6% or 22.9% in China, which were different with our study population, indicating standardized rates were necessary for practice consideration at national level (Supplemental Table 3).
Fig. 1.
Distribution of sample sizes, scores of vaccine confidence, rate of willingness or hesitancy to accept vaccination, and current coverage of vaccination in the mainland of China by province. Sample sizes of each province were symbolized by different colors on the map. A, Scores of confidence to the COVID-19 vaccination. Scores ranged from 17.26 to 20.14 and were classified into five categories based on their distribution and symbolized by different sizes. B, The rate of willingness to the COVID-19 vaccination. The rate of willingness ranged from 57.6% to 79.9% and was classified into five categories based on their distribution and symbolized by different sizes. C, Vaccine hesitancy rate to the COVID-19 vaccination. The rate of willingness ranged from 21.1% to 58.8% and was classified into six categories based on their distribution and symbolized by different sizes. D, Vaccination rate of the COVID-19 vaccination in the present survey. The rate of willingness ranged from 10.0% to 70.0% and was classified into six categories based on their distribution and symbolized by different sizes.
Table 1.
Characteristics of study participants in the vaccine-priority group and non-priority group.
| Characteristics | Total n (%) | Vaccine Priority group n (%) | Non-priority group n (%) | P value |
|---|---|---|---|---|
| Total | 8742 (100) | 3902 (44.6) | 4840 (55.4) | |
| Gender | ||||
| Male | 3207 (36.7) | 1529 (39.2) | 1678 (34.7) | <0.001 |
| Female | 5535 (63.3) | 2373 (60.8) | 3162 (65.3) | |
| Age group, years | ||||
| <30 | 2632 (30.1) | 993 (25.4) | 1639 (33.9) | <0.001 |
| 30–39 | 3277 (37.5) | 1402 (35.9) | 1875 (38.7) | |
| 40–49 | 1677 (19.2) | 924 (23.7) | 753 (15.6) | |
| ≥50 | 1156 (13.2) | 583 (14.9) | 573 (11.8) | |
| Education | ||||
| ≤High school | 1275 (14.6) | 463 (11.9) | 812 (16.8) | <0.001 |
| Bachelor’s degree | 5547 (63.5) | 2643 (67.7) | 2904 (60.0) | |
| ≥Master’s degree | 1920 (22.0) | 796 (20.4) | 1124 (23.2) | |
| Residence | ||||
| Urban | 6895 (78.9) | 2966 (76.0) | 3929 (81.2) | <0.001 |
| Rural | 1847 (21.1) | 936 (24.0) | 911 (18.8) |
Fig. 2.
Distribution of occupations, current vaccination rate, and vaccine confidence. A, Occupations and sample sizes among the priority and non-priority groups. B, The current vaccination rates of different priority occupations. C, The rate of trust in the COVID-19 vaccine among the total population. D, The rate of trust in the vaccine delivery system among the total population. E, The rate of trust in the government among the total population.
3.2. Vaccine confidence to COVID-19
The total scores of participants’ confidence in COVID-19 vaccine are mapped in Fig. 1A. The provinces with the top five median total scores were Xinjiang, Jiangxi, Hunan, Shandong, and Henan, and those with the bottom three scores were Jilin, Liaoning, and Tibet. However, the differences in the total score were small among the provinces. The rates of people’s trust in the vaccine, delivery system, and government were 69.0% (95% CI 68.0%–70.0%), 78.0% (95% CI 77.1%–78.9%), and 81.3% (95% CI 80.5%–82.1%), respectively (Fig. 2C-E and Supplemental Table 4). All three dimensions of vaccine confidence revealed significantly higher rates in males, rural residents, and the vaccine-priority group (all P < 0.05), excepting gender for trust in government (P = 0.065) and residence for trust in the vaccine (P = 0.403). Vaccine confidence rates increased with increasing age and decreasing education levels (all P < 0.05), respectively. Similar trends were observed in both the vaccine-priority and non-priority groups (Supplemental Table 4). For the priority group, medical employees reported higher rates in all three dimensions of vaccine confidence. Significant differences were observed in age, gender (only in trust in vaccine), and education (only in trust in government). While for the non-priority group, most comparisons were significant (P < 0.05).
The multivariate logistic regression model revealed that distrust in the vaccine was associated with female sex, younger age, higher education level, and being in the non-priority group (all P < 0.05, Supplemental Table 5); distrust in the delivery system was associated with female sex, younger age, and being in the non-priority group (all P < 0.05, Supplemental Table 6); distrust in the government was associated with younger age, higher education level, and being in the non-priority group (all P < 0.05, Supplemental Table 7).
3.3. Vaccination willingness to COVID-19
The rates of vaccination willingness to COVID-19 were mapped in Fig. 1B. The top five provinces with vaccination willingness to COVID-19 were Xinjiang (79.9%), Jiangxi (77.3%), Qinghai (74.2%), Shanxi (73.0%), and Hubei (71.8%). There were nine provinces with COVID-19 vaccination willingness rates under 65%.
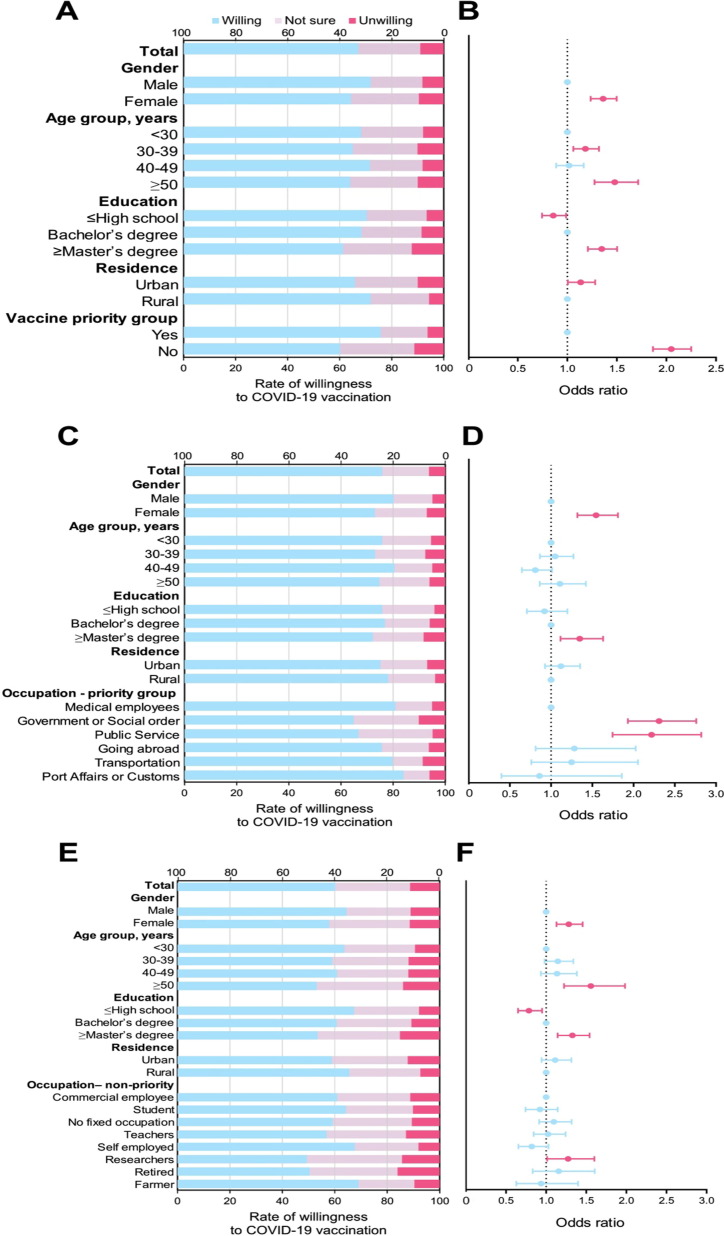
As a whole, 67.1% (95% CI 66.1%–68.1%) participants reported willingness to accept the COVID-19 vaccination and 9.0% (95% CI 8.4%–9.6%) reportedly refused the COVID-19 vaccination (Fig. 3 and Supplemental Table 8–9). The rate of willingness to accept the COVID-19 vaccination was higher in males than in females (71.9% vs. 64.4%, P < 0.001). Participants aged 40–49 years reported the highest rate (71.7%) of vaccination willingness among the four age groups. The rate of willingness to accept the COVID-19 vaccination also increased with decreasing education levels (P < 0.001) and in participants from rural areas and in the vaccine-priority groups (both P < 0.05). Among the vaccine-priority group, those working in port affairs or customs reported the highest rate of vaccine willingness (84.0%), followed by medical employees (80.8%), and transportation (79.8%). Lower rates of vaccine willingness were observed in the non-priority group, in which the top three occupations with vaccine willingness were farmer (69.0%), self-employed (67.6%), and student (64.2%). Multivariate logistic regression model showed that an unwillingness to accept the COVID-19 vaccination was associated with female sex, older age, higher education level, urban residence, and being in the non-priority group (Fig. 3 and Supplemental Table 10). In comparison, no significant association between unwillingness to accept COVID-19 vaccination existed in the variables of age and residence for the vaccine-priority and non-priority groups, respectively.
Fig. 3.
Distribution of willingness to accept the COVID-19 vaccine among different study participants. A, Rate of willingness to accept the COVID-19 vaccination among the total participants. B, Odds ratios comparing the rate of willingness to accept the COVID-19 vaccination within populations with different characteristics. C, Rate of willingness to accept the COVID-19 vaccination among the priority group. D, Odds ratios comparing within different characteristics the rate of willingness to accept the COVID-19 vaccination among the priority group. E, Rate of willingness to accept the COVID-19 vaccination among the non-priority group. F, Odds ratios comparing within different characteristics the rate of willingness to accept the COVID-19 vaccination among the non-priority group.
3.4. Vaccine hesitancy to COVID-19 vaccine
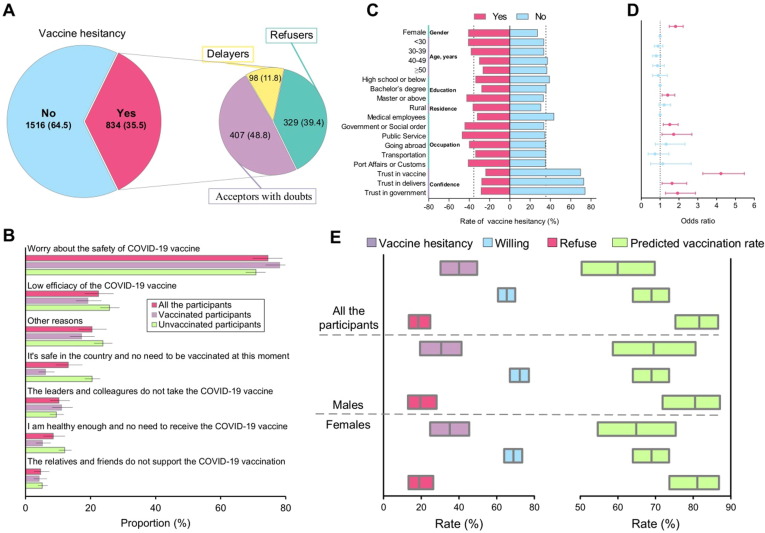
Among the 2350 participants in priority group, 834 (35.5%) reported vaccine hesitancy, including acceptors with doubts (48.8%), refusers (39.4%), and delayers (11.8%) (Fig. 4 A and Supplemental Table 11). The highest rate of vaccine hesitancy was observed in Tibet (55.8%), followed by Ningxia (53.3%), Liaoning (49.0%), Beijing (49.0%), and Hainan (48.4%) (Fig. 1C). The rates of vaccine hesitancy were below 30% in 11 provinces. The most prevalent reason for vaccine hesitancy was concern about the safety of the COVID-19 vaccine (74.6%), followed by low efficacy of the COVID-19 vaccine (22.4%); the reasons were the same among vaccinated and unvaccinated participants (Fig. 4B and Supplemental Table 12). Females had a higher rate of vaccine hesitancy (41.1% vs. 27.5%) compared to males, with an OR of 1.821 (95% CI 1.489–2.226) by multivariate analysis. The rate of vaccine hesitancy decreased with increasing age. The participants with a master’s degree or above had a higher rate (42.8%) of vaccine hesitancy compared to those with a bachelor’s degree. Compared to medical employees, all other priority occupations had higher rates of vaccine hesitancy. The participants with distrust in the vaccine, delivery system, or government showed higher rates of vaccine hesitancy (Fig. 4C and Supplemental Table 10). The multivariate logistic regression model showed that participants with female sex, education level of master’s degree or above, who were employees of the government or in public service, and those with distrust in vaccines, delivery system, or the government were associated with vaccine hesitancy (Fig. 4D).
Fig. 4.
Distribution, reasons for vaccine hesitancy, and the predicted coverage rates based on vaccine hesitancy, vaccine willingness, and vaccine refusal rate. A, Proportion of vaccine hesitancy among the priority group. B, Reasons for hesitancy to the COVID-19 vaccine. C, Rate of vaccine hesitancy among populations with different characteristics and confidence D, Odds ratios comparing within different characteristics on the rate of hesitancy to vaccination among the priority group. E, The predicted vaccination coverage based on vaccine hesitancy, vaccine willingness, and vaccine refusal rate.
3.5. Current rate of vaccination and predicted rate among unvaccinated people
A total of 34.4% (1341/3902) of the vaccine-priority participants had received the COVID-19 vaccine [35.6% (545) males and 33.5% (796) females], among which 393 (42.5%) were aged between 40 and 49 years, and 29.1% were aged below 30 years. Higher rates of vaccination were observed in Jiangxi, Xinjiang, and Tianjin (Fig. 1D). The rate of vaccination among participants with a master’s degree or above was 37.8%, compared to 20.3% among those with a high school or below education level. Urban participants (37.1%) received more vaccinations compared to rural participants (25.9%). Medical employees had the highest vaccination rate at 47.5%, while the vaccination rate among public service workers was 6.8% (Fig. 2B). Among the 1341 vaccine acceptors, 263 (19.6%) had injection site reaction pain, itching, or redness. The fatigue rate was 7.8% (105 persons), followed by lethargy, headache, nausea, pain, fever, and vomiting.
The rates of COVID-19 vaccine hesitancy, willingness, and refusal were standardized using population data in China by age and gender (Fig. 4E and Supplemental Table 13). The predicted rate of COVID-19 vaccination was 64.85% (95% CI 54.6%–75.4%), 68.92% (95% CI 63.9%–73.6%), and 81.1% (95% CI 73.7%–86.8%) based on rates of vaccine hesitancy, vaccination willingness, and vaccination refusal, respectively.
4. Discussions
As an important intervention in controlling the COVID-19 pandemic, all countries have been actively promoting the allocation of the COVID-19 vaccine. Our results demonstrated a relatively high willingness or confidence in the COVID-19 vaccine in the mainland of China, which was associated with high vaccine uptake.
4.1. Vaccination willingness
Given the current concerns on the COVID-19 pandemic, the willingness to be vaccinated against COVID-19 has become an important public health issue. Our study reported 67.1% of participants were willing to accept the available COVID-19 vaccine, which was lower than the surveyed willingness rate to COVID-19 vaccine (91.3%) in 2020 in China by Wang et al. [19]. Yoda et al. reported that 65.7% of their participants indicated willingness to receive COVID-19 vaccine in Japan [20], and Sun et al. showed that 64% indicated a willingness to participate in COVID-19 vaccine trials among young adults in China [21]. These results suggest that vaccination willingness may be postponed now that a vaccine is available than when it was not available.
As a high-risk group for COVID-19, the priority population showed a relatively higher willingness to be vaccinated than that of the non-priority population [22]. Particularly, people more closely or directly responsible for pandemic control showed more vaccination willingness. We identified that participants with a master’s degree or above reported the lowest willingness which may due to the reason that this population believed themselves to be more knowledgeable about the disease and ways to protect themselves [23], and the short clinical observation time of the newly developed COVID-19 vaccine increased their worries regarding vaccine safety and effectiveness [24]. Females showed a significantly lower willingness to be vaccinated compared to males, which is consistent to Thunstrom’s report [25]. Notably, nearly 3.7% of people who reported a willingness to receive the vaccination refused to accept it. These results highlight the importance of considering not only technical and medical issues but also social issues when developing vaccination plans that address the needs of the society.
4.2. Vaccination confidence
Population trust in the COVID-19 vaccine was obviously below that of previous studies in other vaccines and reflected the uncertainty to the newly developed vaccine among the Chinese population [14], [26]. In addition, a higher proportion (81.3%) reported trust in the government. We also found the priority population’s confidence in the three dimensions was significantly higher than that of the non-priority population. However, it should be noted that nearly 10% of the people who reported high confidence in the vaccine still refused to accept the COVID-19 vaccination. Therefore, more efforts are needed to improve the public’s knowledge of the vaccine and to enhance the public’s trust in delivery systems or government by providing accurate and timely information [27].
4.3. Vaccination hesitancy
We found that vaccination willingness or confidence made a significant difference in participants’ vaccine hesitancy. Moreover, by our results, nearly 10% of the people who reported high confidence in the vaccine, as well as 3.7% of people who were willing to be vaccinated, still refused to accept COVID-19 vaccination. As a previous study claimed, providing information on the safety and effectiveness of the COVID-19 vaccine is crucial for people with vaccination hesitancy [28], as vaccine refusers or hesitators lacked trust in the health service system or government and would be more sensitive to misinformation about the COVID-19 vaccine [29]. The vaccine delivery system and government were important sources of vaccine-related information for the public and played key roles in addressing vaccine hesitancy [14]. Therefore, it is indicated that even if there were adequate vaccines available for the population, sufficiently high vaccination coverage may not be achieved when public willingness or confidence in vaccination remains at a low level.
Our results showed that the proportion of vaccine hesitancy to the COVID-19 vaccine was similar to those of other vaccines in previous reports among the American population, but higher than the 6% COVID-19 vaccine resistance rate reported among the Australian population [30]. Du et al. reported in 2020 that a 3% overall refusal rate to general vaccines was observed among 2124 participants from the mainland of China [14]. In our study, the resistance rate to the COVID-19 vaccine was higher than that reported in those previous reports. This might be due to several reasons. Firstly, because of the low incidence rate of COVID-19, many people may think it is not necessary to receive the vaccine. Second, negative reports on vaccine adverse events may impact confidence and vaccination willingness among Chinese people [31]. Our results supported this hypothesis as public trust in the government or delivery systems on the issue of the COVID-19 vaccine was around 80%, while their trust in the vaccine was relatively low at 69%. In the meantime, meaningful differences were found between the vaccinated and unvaccinated group in the questions of belief that one is not at risk and one is healthy enough to be vaccinated, which support Wang et al.'s finding that many willing individuals would like to postpone their willingness until there is more experience with the vaccine [19]. As discussed before, non-priority public might tend to underestimate the pandemic since China has conducted strict measures in disease prevention.
Multivariate analysis indicated that trust in the vaccine was a main determinant of vaccine hesitancy. As newly developed and has had a short clinical evaluation, scientific data or evidence on the effectiveness or safety, COVID-19 vaccine has not been convincing enough among general population, especially those with insufficient medical knowledge. The frequency of uncertain scientific conclusions is at a very high level, which may reduce the public’s confidence and willingness to vaccinate, along with a high proportion of hesitancy. Participants in our study with master’s degree or above education reported the lowest proportion of vaccination willingness or confidence in COVID-19 vaccine; however, they had the highest proportion (nearly 30%) of vaccine uptake with hesitancy. Although participants with higher education may have better access to more information and might be more suspicious, they simultaneously had a higher awareness of the value of the vaccine in preventing COVID-19 [14].
4.4. Vaccination coverages
Our survey showed that the present coverage of the COVID-19 vaccination was 34.4%. A large gap remains between the current vaccination coverage and the targeted coverage of ≥70% by the Chinese National Health Commission [32]. Coverage was further predicted based on the rates of vaccine hesitancy, willingness, and refusal to accept COVID-19 vaccination.
In the present survey, differences were shown from the comparison of specific characteristics between study sample and Chinese population. Thus, standardized rates of vaccine hesitancy, willingness or refusal to vaccination were calculated by age and gender. The most conservative prediction was estimated on the standardized rate of vaccine hesitancy as 35.2%, anticipating that 64.8% of the Chinese population would receive the vaccine without hesitancy when it was fully accessible. As discussed above, people with vaccine willingness had the highest probability of receiving the vaccination, despite some resistance. Thus, the anticipated coverage is 68.9%, including the potential population with hesitancy that still accept the vaccination. The most vigorous anticipated future vaccine coverage is 81.1% if we only exclude those who will certainly refuse the vaccination. To acquire this, more flexible and comprehensive efforts, including but not limited to dissemination of low rate and mild adverse reactions, and high protective efficiency, are needed to improve the population’s confidence and willingness to accept vaccination, along with an efficient vaccination mechanism with sufficient vaccine production capacity.
As reported on December 31, 2020; January 21, 2021; January 29, 2021; and February 3, 2021, three million, 15 million, 22.7 million, and 33.1 million COVID-19 vaccine doses have been distributed in the mainland of China, respectively. The vaccination rate has increased from nearly 570 thousand doses/day to over 2 million/day, and the rate is still accelerating [3], [5], [32], [33]. Based on the most current vaccination scenario, the necessary vaccination coverage of 70% among the priority population will be reached within one month. At the reported current vaccine production capacity of nearly 1 billion doses per year, 64.8% to 81.1% (nearly 650 to 800 million people) of the public aged between 18 and 59 years would be vaccinated within 11 to 14 months [34].
5. Limitations
There are some limitations to our study. First, the online questionnaires led to a biased selection, which may suffer from lack of representativeness of the target population. The respondents were mainly female, medical employees, urban residents, and those with higher education levels, which may interfere with the estimation of the population’s willingness and confidence rate of vaccination. To mitigate the representative bias to a large extent, the rate of vaccine hesitancy, willingness and refuse to accept COVID-19 vaccination were standardized by age and gender from the whole population data in 2017 in China (Supplemental Table 13). Also, the unstandardized rates of vaccine hesitancy, willingness and refusal would be helpful in policy making among specific targeted populations. Second, although we performed quality control, there may be errors in the information because the online questionnaire cannot be modified after filling in; however, these errors were unlikely to change our findings. Third, this study is a cross-sectional survey and cannot show dynamic trends. Fourth, the vaccination coverage may be affected by other factors. Hence, we might have over- or under-estimated the coverage. In order to dynamically assess vaccination willingness, confidence, and coverage of the Chinese population, a follow-up survey should be conducted to look at this issue.
6. Conclusions
This study proved that vaccination willingness and confidence, which were affected by the demographic characteristics of participants, are key factors driving people’s behaviors to receive the COVID-19 vaccine. Moreover, this study also showed that people who were confident and willing to receive the vaccination might not necessarily choose to be vaccinated; vaccine hesitancy was the key factor preventing people from receiving the vaccine. It is necessary to provide accurate and timely education on the COVID-19 vaccine and adopt comprehensive measures to improve the population’s willingness and confidence before vaccination. The study also pointed out that based on the current vaccination situation, coverage of the COVID-19 vaccine is far from reaching the requirements of herd immunity, which is anticipated to be acquired based on more flexible and comprehensive efforts to improve the population’s confidence, improve vaccination willingness, and reduce vaccine hesitancy. Furthermore, it should be highlighted that vaccination alone is not sufficient to stop the pandemic; further efforts are needed not only to increase the vaccination coverage, but also to maintain non-specific prevention strategies, such as wearing a face mask, washing hands, quarantining patients, tracing the infection, and maintaining a physical distance.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgements
This work was supported by Fundamental Research Funds for the Central Universities and Peking University Health Science Center (grant numbers BMU20170607), Peking University Medicine Fund of Fostering Young Scholars’ Scientific & Technological Innovation and Joint Research Fund for Beijing Natural Science Foundation and Haidian Original Innovation (L202007).
Data availability
Original data are available on request. These were stored on password protected computers at Department of Laboratorial Science and Technology & Vaccine Research Center, School of Public Health, Peking University. Readers who wish to gain access to the data can write to the corresponding author.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.vaccine.2021.04.020.
Appendix A. Supplementary material
The following are the Supplementary data to this article:
References
- 1.WHO. WHO Coronavirus Disease (COVID-19) Dashboard. 2021. Available from: https://covid19.who.int/.
- 2.WHO. COVID-19 vaccines. 2021. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/covid-19-vaccines.
- 3.People's Daily. The first new coronavirus vaccine is listed on conditional conditions (State Council Joint Prevention and Control Mechanism Press Conference). 2020. Available from: https://news.china.com/social/1007/20210101/39137891.html.
- 4.Jiale F. National Health Commission: Vaccination for key populations launched on December 15 Individuals do not bear the cost and vaccination expenses. 2021. Available from: https://www.360kuai.com/pc/9d13a28d1c996adb4?cota=3&kuai_so=1&tj_url=so_vip&sign=360_57c3bbd1&refer_scene=so_1.
- 5.Shuli W. National Health Commission: As of February 3, a total of 31.236 million doses of new coronavirus vaccines have been reported to key populations across the country. 2021. Available from: http://news.cri.cn/20210204/180737da-3f71-e44a-b97d-67c3be4e8055.html.
- 6.Persad G., Peek M.E., Emanuel E.J. Fairly Prioritizing Groups for Access to COVID-19 Vaccines. JAMA, J Am Med Assoc. 2020;324(16):1601–1602. doi: 10.1001/jama.2020.18513. [DOI] [PubMed] [Google Scholar]
- 7.Randolph H.E., Barreiro L.B. Herd Immunity: Understanding COVID-19. Immunity. 2020;52(5):737–741. doi: 10.1016/j.immuni.2020.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sanche S., Lin Y.T., Xu C., Romero-Severson E., Hengartner N., Ke R. High contagiousness and rapid spread of severe acute respiratory syndrome coronavirus 2. Emerg Infect Dis. 2020;26(7):1470–1477. doi: 10.3201/eid2607.200282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Irtesam M.K., Wenyi Z., Sumaira Z., et al. COVID-19 in China: risk factors and R0 revisited. ACTA TROP. 2021;213:105731. doi: 10.1016/j.actatropica.2020.105731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xiao W, Yiyin Q. Sinopharm's new crown vaccine was approved for marketing, with a protection rate of 79.34%. 2021. Available from: https://www.163.com/dy/article/FVOK3II705373W47.html.
- 11.Bin W. The effective rate of Kexing's new crown vaccine is only 50%? The chairman responded how to understand this number. 2021. Available from: https://www.sohu.com/a/445726378_161795.
- 12.Sherman SM, Smith LE, Sim J, Amlôt R, Cutts M, Dasch H, et al. COVID-19 vaccination intention in the UK: results from the COVID-19 vaccination acceptability study (CoVAccS), a nationally representative cross-sectional survey. HUM VACC IMMUNOTHER 2020 2020-11-26:1-10. [DOI] [PMC free article] [PubMed]
- 13.Frank K, Arim R Canadians’ willingness to get a COVID-19 vaccine: Group differences and reasons for vaccine hesitancy. Statistics Canada Catalogue 45280001: No. 00043.
- 14.Du F., Chantler T., Francis M.R., Sun F.Y., Hou Z. The determinants of vaccine hesitancy in China: A cross-sectional study following the Changchun Changsheng vaccine incident. Vaccine. 2020;38(47):7464–7471. doi: 10.1016/j.vaccine.2020.09.075. [DOI] [PubMed] [Google Scholar]
- 15.Chen B., Zhang J.M., Jiang Z., Shao J., Jiang T., Wang Z., et al. Media and public reactions toward vaccination during the 'hepatitis B vaccine crisis' in China. Vaccine. 2015;33(15):1780–1785. doi: 10.1016/j.vaccine.2015.02.046. [DOI] [PubMed] [Google Scholar]
- 16.Chou W.Y.S., Budenz A. Considering emotion in COVID-19 vaccine communication: addressing vaccine hesitancy and fostering vaccine confidence. Health Commun. 2020;35(14):1718–1722. doi: 10.1080/10410236.2020.1838096. [DOI] [PubMed] [Google Scholar]
- 17.Macdonald N.E. Vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015;32(34):4161–4164. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 18.Domek G.J., O’Leary S.T., Sheana B., Michael B., Contreras-Roldan I.L., Antonio B.O.V.G., et al. Measuring vaccine hesitancy: Field testing the WHO SAGE Working Group on Vaccine Hesitancy survey tool in Guatemala. Vaccine. 2018;36(35):5273–5281. doi: 10.1016/j.vaccine.2018.07.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang J., Jing R., Lai X., Zhang H., Lyu Y., Knoll M.D., et al. Acceptance of COVID-19 vaccination during the COVID-19 Pandemic in China. Vaccines. 2020;8(3):482. doi: 10.3390/vaccines8030482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yoda T., Katsuyama H. Willingness to Receive COVID-19 Vaccination in Japan. Vaccines. 2021;9(1):48. doi: 10.3390/vaccines9010048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sun S, Lin D, Operario D. Interest in COVID-19 vaccine trials participation among young adults in China: Willingness, reasons for hesitancy, and demographic and psychosocial determinants. Preventive Medicine Reports 2021 2021-01-01;22:101350. [DOI] [PMC free article] [PubMed]
- 22.Brown C.S., Ravallion M. Inequality and the Coronavirus: Socioeconomic Covariates of Behavioral Responses and Viral Outcomes Across US Counties. National Bureau of Economic Research Working Paper Series 2020, 27549.
- 23.Han B., Zhao T., Liu B., Liu H., Cui F. Public awareness, individual prevention practice, and psychological effect at the beginning of the COVID-19 outbreak in China. J Epidemiol. 2020;30(10):474–482. doi: 10.2188/jea.JE20200148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Medical Wheat Observation. Is the newly developed COVID-19 vaccine safe within one year? 2021. Available from: https://www.163.com/dy/article/G1JG7R0E05448CTD.html.
- 25.Thunstrom L., Ashworth M., Finnoff D., Newbold S. Hesitancy towards a COVID-19 vaccine and prospects for herd immunity. Covid Econ. 2020;35(7):1–50. [Google Scholar]
- 26.Tu S., Sun F.Y., Chantler T., Zhang X., Jit M., Han K., et al. Caregiver and service provider vaccine confidence following the Changchun Changsheng vaccine incident in China: A cross-sectional mixed methods study. Vaccine. 2020;38(44):6882–6888. doi: 10.1016/j.vaccine.2020.08.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lorini C., Collini F., Gasparini F., Paolini D., Grazzini M., Ierardi F., et al. Health Literacy, vaccine confidence and influenza vaccination uptake among nursing home staff: A cross-sectional study conducted in Tuscany. Vaccines. 2020;8(2):154. doi: 10.3390/vaccines8020154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Linda Cecilia, Karlsson Stephan, Lewandowsky Jan, et al. The association between vaccination confidence, vaccination behavior, and willingness to recommend vaccines among Finnish healthcare workers. PLOS One. 2019;14(10):e224330. doi: 10.1371/journal.pone.0224330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Edwards K.M., Hackell J.M. Countering vaccine hesitancy. Pediatrics. 2016;138(3):e20162146. doi: 10.1542/peds.2016-2146. [DOI] [PubMed] [Google Scholar]
- 30.Edwards B., Biddle N., Gray M. Sollis K (2021) COVID-19 vaccine hesitancy and resistance: Correlates in a nationally representative longitudinal survey of the Australian population. PLoS ONE. 2021;16(3):e0248892. doi: 10.1371/journal.pone.0248892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Haiyan Z., Ping S. Research on deliberation and public rationality in online public opinion events. J Northeastern Uni (Social Sci) 2019;21(2):165–172. [Google Scholar]
- 32.Bin X. [Prevention and Control of Outbreak] Experts Interpretation of COVID-19 Vaccine (Phase 4). 2021. Available from: https://www.thepaper.cn/newsDetail_forward_10963660.
- 33.Junping W. The number of COVID-19 vaccination in China exceeds 15 million person-times (State Council Joint Prevention and Control Mechanism Press Conference). People's Daily. 2021 2021-01-21. Available from: http://paper.people.com.cn/rmrb/html/2021-01/21/nw.D110000renmrb_20210121_1-13.htm.
- 34.Zhonghua Y. Ministry of Industry and Information Technology: Till now, 18 domestic companies have successively carried out production capacity construction of COVID-19 vaccine. China City News. 2021 2021-01-11. Available from: http://paper.people.com.cn/zgcsb/html/2021-01/11/content_2028449.htm.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Original data are available on request. These were stored on password protected computers at Department of Laboratorial Science and Technology & Vaccine Research Center, School of Public Health, Peking University. Readers who wish to gain access to the data can write to the corresponding author.