FIGURE 1.
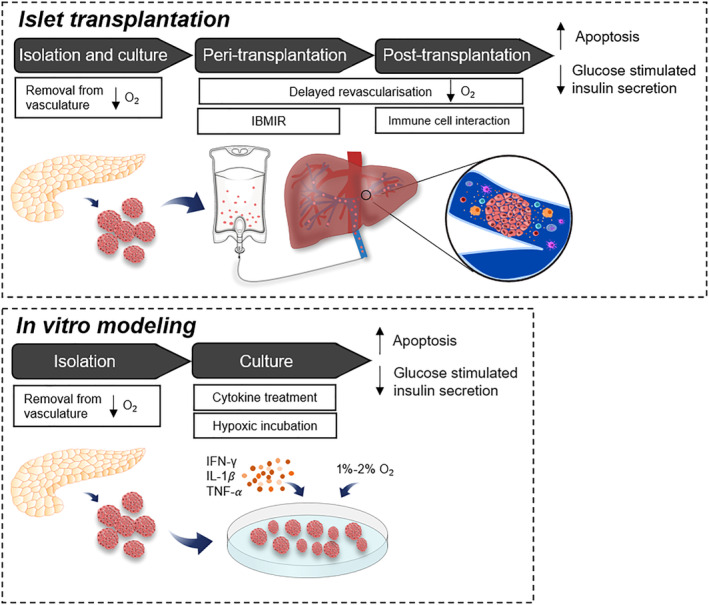
Islets are subjected to hypoxic and inflammatory stressors throughout the isolation and transplantation process. Islets are removed from their dense vasculature during the isolation process and maintained at a lower oxygen environment in the subsequent culture period. Following transplantation, islet graft revascularization begins within a week but islets must rely on a limited oxygen supply from portal venous blood flow prior to this. Infusion of islets into the hepatic portal vein triggers the nonspecific inflammatory and thrombotic reaction called the immediate blood‐mediated inflammatory reaction (IBMIR). Activated innate immune cells continue to interact with islets post‐transplantation, releasing free radicals and pro‐inflammatory cytokines. The sum of these prolonged stressors leads to an increase in islet cell apoptosis and a decrease in glucose stimulated insulin secretion, which reduces the long‐term efficacy of the graft. Peri‐ and post‐transplantation conditions can be modeled in vitro by treatment with pro‐inflammatory cytokines (IFN‐γ, IL‐1β, and TNF‐α) and incubation in 1% to 2% O2, with similar effects on cell death and function
