Abstract
A 48-year-old female presented to the emergency department with chest pain and collapsed at the front desk. She was reanimated with mechanical chest compression, and after coronary angiography, a left anterior descending/diagonal bifurcation mini-crush stenting was performed. Few hours after the procedure, the patient showed severe hypotension. Abdominal ultrasound and computed tomography (CT) scan evidenced a massive subcapsular liver hematoma (Grade IV, American association for the surgery of trauma (AAST) liver injury scale) of the right lobe with extrahepatic blushing. Transhepatic embolization was attempted but without benefit, so the patient underwent emergency laparotomy for damage control surgery with perihepatic packing. After hemodynamic stabilization, right hepatectomy was performed with a favorable outcome and full recovery. The patient CT scan was retrospectively processed to obtain a virtual model visualizable through a head-mounted display. The virtual reconstruction could improve the comprehension of the injury and the liver surgical anatomy for educational purpose, and it could represent a new tool for preoperative planning.
Keywords: Case report, emergency setting, liver trauma, mechanical cardiopulmonary resuscitation, virtual reality
INTRODUCTION
Survival rates for out-of-hospital cardiac arrest range from 3% to 16% in North America.[1] Some guidelines consider as essential the effectiveness of chest compression during cardiopulmonary resuscitation (CPR) and propose the use of automatic mechanical chest compression for prolonged or prehospital CPR.[2] Automatic compression devices for CPR have been developed as an alternative to standard manual CPR to improve blood circulation and oxygen supply of unresponsive victims to the heart and brain, generating systemic pressures, and flow superior to those obtained with manual chest compression in human models.[3]
A limited number of studies has been reported in the medical literature describing the different injuries caused by the automated CPR devices.[4,5] We report a case of liver injury in a patient with refractory ventricular fibrillation following myocardial infarction who received CPR by a mechanical cardiopulmonary device. Moreover, a postoperative three-dimensional (3D) reconstruction of the scenario was performed to evaluate the applicability of this technology to the emergency setting.
CASE REPORT
A self-admitted 48-year-old femaleaccusing chest pain collapsed at the desk of the emergency department. CPR was immediately started, but the woman was in ventricular fibrillation refractory to electrical and pharmacological cardioversion. After 10 min of resuscitation, a mechanical chest compression device “Lund University Cardiac Assist System” was applied, and a return of spontaneous circulation was obtained after 25 min. Electrocardiogram showed an anterior ST elevation with a severely impaired left ventricular ejection fraction observed with heart ultrasound. After intravenous administration of aspirin and crushed ticagrelor, the patient underwent coronary angiography with evidence of an occluded left anterior descending/diagonal bifurcation. After thrombus aspiration and intravenous tirofiban, a bifurcation mini-crush stenting technique was performed.
The patient showed a full recover with good hemodynamic parameters. After 4 h from the end of angioplasty, severe hypotension was observed. An abdominal ultrasound showed intraperitoneal bleeding, and a computed tomography (CT) scan evidenced a massive subcapsular liver hematoma (Grade IV, AAST liver injury scale) of the right lobe with extrahepatic blushing [Figure 1].
Figure 1.
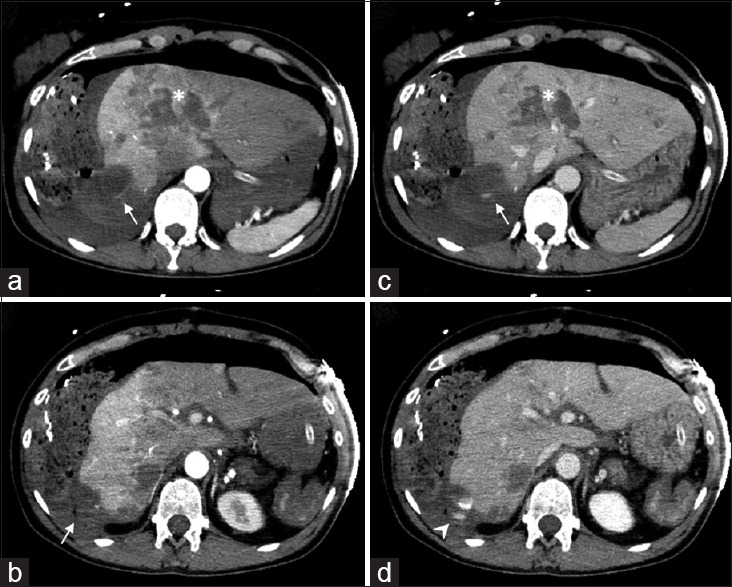
Computed tomography scan of severe liver trauma (Grade IV, AAST Liver Injury Scale) after damage control surgery with perihepatic packing. Two different levels of the arterial (a and b) and venous phases (c and d) are shown. It can be noticed the large subcapsular hematoma in Segment VI and Segment VII (arrow) with extrahepatic blushing (arrowhead), as well as the extensive involvement of Segment IV (asterisk)
A first attempt of transhepatic embolization to stop the source of bleeding failed, so the patient underwent emergency laparotomy for damage control surgery with perihepatic packing. After hemodynamic stabilization, a second multi-detector row CT scan with a slice thickness of 3 mm was performed 24 h later. In consideration of the tendency of the liver hematoma to enlarge, the patient was submitted to right hepatectomy with a favorable outcome and full recovery. She was discharged home on hospital day 12.
Soon after the surgery, the Digital Imaging and Communications in Medicine images of the arterial and portal venous phase were retrieved from the Picture Archiving and Communication System and uploaded into 3D Slicer v. 4.10.0 (www.slicer.org). As a part of the ongoing clinical trial to evaluate the potential benefit of the 3D liver visualization in the emergency setting, the anatomical structures of surgical interest were segmented using semiautomatic algorithms with manual refinements of the boundary [Figure 2].
Figure 2.
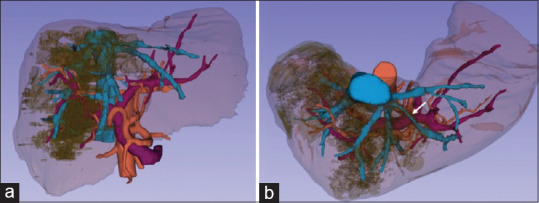
(a) Whole liver vascularization in relationship with the lesion; (b) the left hepatic vein appears to be stretched (white arrow). BLUE: Hepatic venous drainage, PURPLE: Portal vascularization, RED: Arterial vascularization
The obtained 3D scene was finally uploaded in a virtual reality environment developed in Unity (Unity Technologies, San Francisco, CA, USA) to be visualized by a mobile head-mounted display.[6] As better showed by the immersive virtual 3D visualization, Segment IV was lacerated from the subdiaphragmatic capsule nearly to Rex recessus. The 3D virtual liver visualization also allowed appreciating how the lacerations and contusion involved Segment VIII and continued downward sagittally crossing Segment V. The virtual model was developed in our emergency department to better quantify the extension liver injuries. In this patient, the visualization of the large subcapsular hematoma occupying the posterior part of Segment VII as well as the relationships between the images of the liver lesion and the intrahepatic vessels were compared with those of the standard CT scan. In the 3D liver reconstruction, it was particularly evident how the right hepatic vein and the two hepatic veins originating from the common trunk were compressed and divaricated by the lesion. In correspondence of Segment IVa, no arterial or venous vessels were visible because they were stretched or truncated by the large hematoma. The right vascular pedicle was crossed by the parenchymal laceration that reached Segment V and VI [Figures 3-5].
Figure 3.
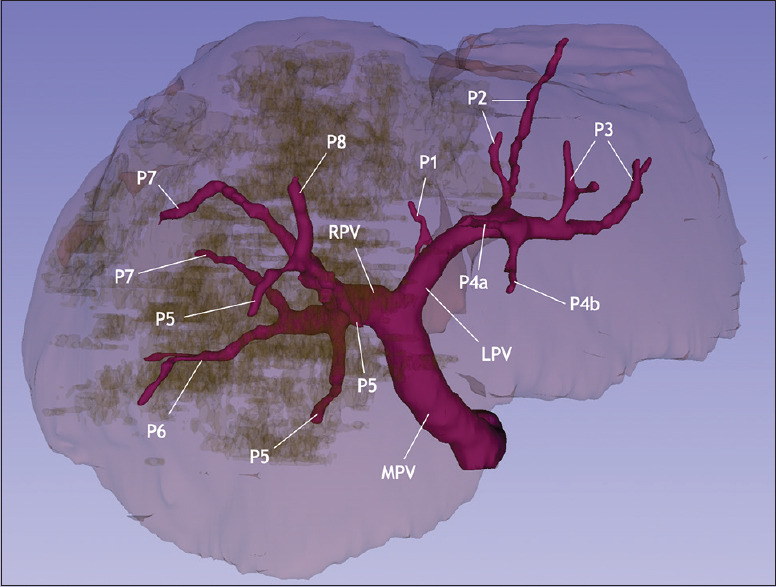
Portal vascularization. P1-P8 defines the corresponding portal branch supplying the corresponding liver segment. MPV: Main portal vein, RPV: Right portal vein, LPV: Left portal vein
Figure 5.
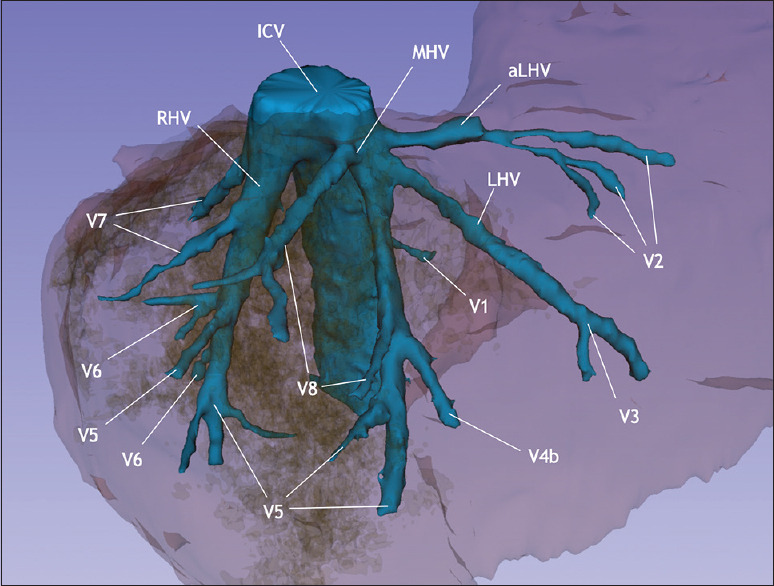
Hepatic venous drainage. V1-V8 defines the corresponding venous branch for each liver segment draining into the inferior cava. IVC: Inferior vena cava, MHV: Medial hepatic vein, RHV: Right hepatic vein, LHV: Left hepatic vein
Figure 4.
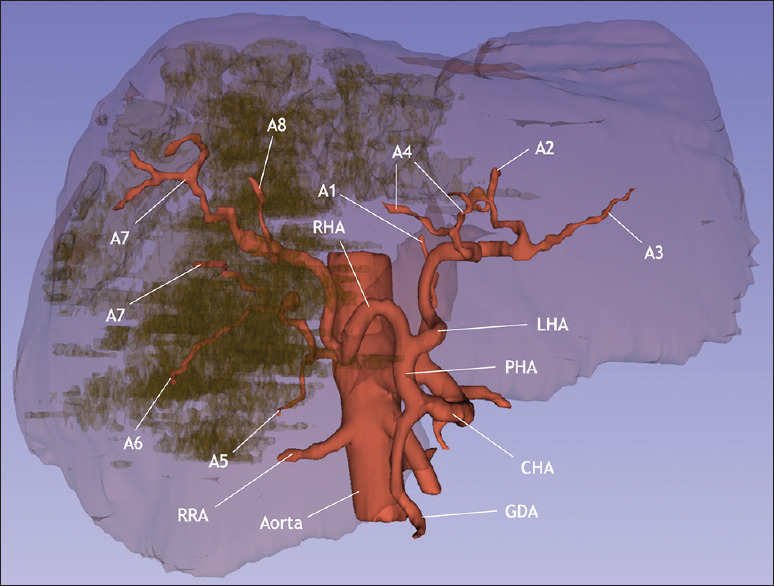
Arterial vascularization. A1-A8 defines the corresponding arterial branch supplying the corresponding liver Segment. GDA: Gastroduodenal artery, CHA: Common hepatic artery, PHA: Proper hepatic artery, RHA: Right hepatic artery, LHA: Left hepatic artery, RRA: Right renal artery
DISCUSSION
CPR is a procedure applied to increase the survival of patients in cardiovascular arrest. However, during manual or mechanical CPR, several complications may occur because of chest compressions that may result in fatal complications. The most frequent injuries are sternum and rib fractures, which can harm internal organs and reduce the patient’s chance of survival. Rarer complications include tracheal injury, gastric rupture, or injury to solid organs (liver and spleen). Especially, liver damage during CPR is seen at an incidence of 0.6% and seems the most frequent intraabdominal complication related to CPR.[7] However, it should be noted that in the case here described there was a concomitant drug-associated risk factor, i.e., the concomitant antiplatelet therapy administered to the patient which although rarely has been associated to a spontaneous liver injury.[8]
In addition, in this case report, we have illustrated the use of a 3D liver model which can be realized from the patient’s CT scan in about 2 h from the image acquisition. This novel application of 3D virtual reconstruction is part of an ongoing clinical study in our emergency department whose purpose is to visualize in a dedicated virtual reality environment all surgically relevant anatomical structures and to provide a better comprehension of the patient’s liver anatomy with a detailed extension of the lesion. At present, the possible real advantages of this technology applied in the emergency setting are unclear, but hopefully it could provide trauma surgeons with a useful integration of the information from the routine CT scan.
CONCLUSION
Mechanical CPR in patients with antiplatelet therapy should be considered a relevant risk factor for liver and other parenchymal injuries. A safer preoperative spatial knowledge of the liver anatomy in the emergency scenario using 3D reconstruction may help trauma surgeons to plan the most suitable therapeutic strategy in trauma patients.
The authors of this manuscript declare that this scientific work complies with reporting quality, formatting, and reproducibility guidelines set forth by the EQUATOR Network. The authors also attest that this clinical investigation was determined to not require the Institutional Review Board/Ethics Committee review. We also certify that we have not plagiarized the contents in this submission and have done a Plagiarism Check.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Rea TD, Pearce RM, Raghunathan TE, Lemaitre RN, Sotoodehnia N, Jouven X, Siscovick DS. Incidence of out-ofhospital cardiac arrest. Am J Cardiol. 2004;93:1455–60. doi: 10.1016/j.amjcard.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 2.Formalized expert recommendations. Management of cardiac arrest. Ann Fr Anesth Rénim. 2007;26:1008–19. [Google Scholar]
- 3.Timerman S, Cardoso LF, Ramires JA, Halperin H. Improved hemodynamic performance with a novel chest compression device during treatment of in-hospital cardiac arrest. Resuscitation. 2004;61:273–80. doi: 10.1016/j.resuscitation.2004.01.025. [DOI] [PubMed] [Google Scholar]
- 4.Pinto DC, Haden-Pinneri K, Love JC. Manual and automated cardiopulmonary resuscitation (CPR): A comparison of associated injury patterns. J Forensic Sci. 2013;58:904–9. doi: 10.1111/1556-4029.12146. [DOI] [PubMed] [Google Scholar]
- 5.Manzanera J, Millet I, Charbit J, Capdevila X. Fatal pancreatic injury due to trauma after successful cardiopulmonary resuscitation with automatic mechanical chest compression. Anesthesiology. 2014;120:1038–41. doi: 10.1097/ALN.0000000000000147. [DOI] [PubMed] [Google Scholar]
- 6.Vertemati M, Cassin S, Rizzetto F, Vanzulli A, Elli M, Sampogna G, et al. A virtual reality environment to visualize three-dimensional patient-specific models by a mobile head-mounted display. Surg Innov. 2019;26:359–70. doi: 10.1177/1553350618822860. [DOI] [PubMed] [Google Scholar]
- 7.Beydilli H, Balci Y, Erbas M, Acar E, Isik S, Savran B. Liver laceration related to cardiopulmonary resuscitation. Turk J Emerg Med. 2016;16:77–9. doi: 10.1016/j.tjem.2015.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kastalli S, El Aïdli S, Zaïem A, ben Abdallah H, Daghfous R. Fatal liver injury associated with clopidogrel. Fundam Clin Pharmacol. 2010;24:433–5. doi: 10.1111/j.1472-8206.2009.00791.x. [DOI] [PubMed] [Google Scholar]


