Abstract
The ongoing pandemic of the novel coronavirus disease 2019 (COVID-19) originated in Wuhan, China, in December 2019. Various manifestations of coronavirus (SARS-CoV-2 [severe acute respiratory syndrome coronavirus 2]) have been reported since the pandemic began. Some articles have reported acute pancreatitis in several patients due to COVID-19 infection. In this case report, we introduce a patient in whom SARS-CoV-2 caused necrotizing pancreatitis. Acute abdomen is one of the manifestations of COVID-19. Various causes such as acute pancreatitis and necrotizing pancreatitis can be in the list of differential diagnoses.
Keywords: COVID-19, SARS-CoV-2, necrotizing pancreatitis, pandemic
Introduction
The ongoing pandemic of the novel coronavirus disease 2019 (COVID-19) originated in Wuhan, China, in December 2019. So far, more than 4 million people worldwide have been infected with the virus. Many different manifestations of this virus have been reported. In this study, we report the case of a patient with COVID-19 with gastrointestinal manifestations and mild respiratory involvement. This study introduces the involvement of necrotizing pancreatitis in a patient with COVID-19.1
Case Presentation
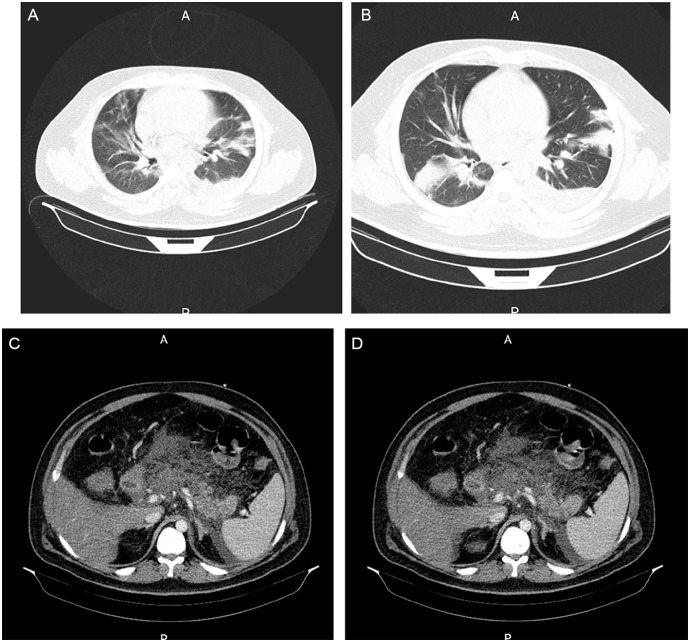
A 28-year-old man was referred to the emergency department of Mousavi Hospital (Zanjan, Iran) with a 5-day history of fever, dry cough, myalgia, and progressive dyspnea. He was hospitalized with a possible diagnosis of acute respiratory distress syndrome. The patient also complained of severe stabbing abdominal pain in the epigastric region with radiation to the back with frequent nausea and vomiting. The patient denied any travel history during the past month. He had no history of addiction, alcoholism, or medication. He was completely healthy a weak before admission. He was dehydrated with the following vital signs: heart rate 118 beats per minute, blood pressure 135/100 mm Hg, temperature 38.8 °C, and oxygen saturation 77% on room air. The abdomen was soft, mildly distended with severe epigastric tenderness and rebound tenderness. Table 1 is a summarized admission laboratory workup. Laboratory testing was repeated and achieved the same results. The patient underwent a chest and abdomen computed tomography (CT) scan. Chest CT was notable for mild left pleural effusion and multifocal bilateral ground-glass opacities on both sides (Figure 1A and B). Abdomen CT was progressed to normal gall bladder, biliary tract with severe inflammation in the fats around the pancreas and stomach. Fat stranding in perinephric fat was seen, especially on the left side. The density of the pancreas was heterogeneous, and the head and body of the pancreas were not enhanced. Mild free fluid was seen in the splenorenal space (Figure 1C and D).
Table 1.
Laboratory Findings in Our Patient.
| Laboratory test | Level | Normal range |
|---|---|---|
| WBC count | 19.3 | 4-10 × 103 cells/µL |
| Neutrophil | 85.3 | 42% to 77% |
| Lymphocyte | 10.2 | 20% to 45% |
| Monocytes | 4.5 | 2% to 6% |
| RBC count | 6.09 | 4.6-6.2 × 106 cells/µL |
| Hemoglobin | 18.3 | 12-16 g/dL |
| Platelet count | 265 | 130-450 × 103 cells/µL |
| Hematocrit | 53.4 | 36% to 52% |
| AST | 87 | <38 U/L |
| ALT | 66 | <40 U/L |
| Alkaline phosphatase | 227 | 98-279 U/L |
| Total bilirubin | 0.9 | 0.1-1.2 mg/dL |
| Direct bilirubin | 0.2 | <0.25 mg/dL |
| Albumin | 3.9 | 3.5-5.5 g/L |
| Amylase | 1273 | <90 U/L |
| Lipase | 758 | <60 U/L |
| Blood sodium level | 136 | 135-145 mEq/L |
| Blood potassium level | 4.2 | 3.5-5.1 mEq/L |
| Blood calcium level | 6.9 | 8.5-10 mg/dL |
| Triglyceride | 122 | 40-160 mg/dL |
| Blood urea nitrogen | 47 | 7-21 mg/dL |
| Creatinine | 1.7 | 0.7-1.4 mg/dL |
| C-reactive protein | 2 | <10 mg/dL |
Abbreviations: WBC, white blood cell; RBC, red blood cell; AST, aspartate transaminase; ALT, alanine aminotransferase.
Figure 1.
(A, B) Chest computed tomography (CT) revealed bilateral subpleural patchy consolidation and ground glass opacities. (C, D) Abdominal CT scan showing the presence of fluid in the splenorenal space and severe inflammation and heterogeneous density of the pancreas.
He was admitted to the intensive care unit with diagnosed severe acute necrotizing pancreatitis with acute respiratory distress syndrome as per the modified Atlanta criteria. The patient received supportive care (the nasogastric tube was fixed, resuscitation with intravenous crystalloid fluid, empiric antibiotic [vancomycin, cefepime], high-flow oxygen therapy, analgesia, and pantoprazole). Later nasal swab for SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2) reverse transcriptase-polymerase chain reaction tested positive. Then oral treatment with oseltamivir, hydroxychloroquine, and ribavirin was started for the patient. The patient was discharged with improved health conditions after a 15-day hospitalization. No adverse reactions happened in this period.
Discussion
Coronaviruses are a large family of viruses with single-stranded RNA. In humans, the virus often causes respiratory manifestations and myalgia. Gastrointestinal manifestations are also seen in some types of the virus.1,2 The association of viral pancreatitis with measles, mumps, and coxsackie viruses has already been well established. In our patient, there was no evidence in favor of viral pancreatitis. The lack of association with known causes of pancreatitis and necrotizing pancreatitis in our patient suggests that the coronavirus is the cause of necrotizing pancreatitis in this patient. Various manifestations of coronavirus (SARS-CoV-2) have been reported since the pandemic began. Some articles have been reported acute pancreatitis in many patients due to COVID-19 infection. This is the first time that the virus has been reported to cause necrotic pancreatitis in a patient. Involvement via angiotensin receptor-converting enzyme-2 and using TMPRSS2 for “priming” has been identified as possible pathogenesis of COVID-19.1-5 Both of these proteins are highly expressed in pancreatic ductal, acinar, and islet cells. SARS-CoV-2 can also cause diffuse severe endotheliitis of the submucosal vessels in several anatomical sites, and these changes, in turn, cause diffuse microischemic disease. Similar ischemic damage could occur in the pancreas.6 With this explanation, the involvement of the pancreas due to this virus can be justified. Our knowledge of this virus and its manifestations is still being completed, and this case report can provide us with background knowledge of the next possible cases.
Conclusion
According to the present findings, it can be said that acute abdomen is one of the manifestations of COVID-19 disease, and various causes such as acute pancreatitis and necrotizing pancreatitis can be causes in the list of differential diagnoses. Proper and timely diagnosis can have a significant impact on the patient’s treatment.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics Approval: Our institution does not require ethical approval for reporting individual cases or case series.
Informed Consent: Verbal informed consent was obtained from the patient to publish anonymized information in this article.
ORCID iD: Mohammad Hadi Molseghi  https://orcid.org/0000-0001-6471-7324
https://orcid.org/0000-0001-6471-7324
References
- 1. Aloysius MM, Thatti A, Gupta A, Sharma N, Bansal P, Goyal H. COVID-19 presenting as acute pancreatitis. Pancreatology. 2020;2:45-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Karimzadeh S, Manzuri A, Ebrahimi M, et al. COVID-19 presenting as acute pancreatitis: lessons from a patient in Iran. Pancreatology. 2020;20:1024-1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Anand E, Major C, Pickering O, Nelson M. Acute pancreatitis in a COVID-19 patient. Br J Surg. 2020;107:e182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hadi A, Werge MP, Kristiansen KT, et al. Coronavirus disease-19 (COVID-19) associated with severe acute pancreatitis: case report on three family members. Pancreatology. 2020;20:665-667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wang F, Wang H, Fan J, Zhang Y, Wang H, Zhao Q. Pancreatic injury patterns in patients with COVID-19 pneumonia. Gastroenterology. 2020;159:367-370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. de-Madaria E, Capurso G. COVID-19, and acute pancreatitis: examining the causality. Nat Rev Gastroenterol Hepatol. 2021;18:3-4. [DOI] [PMC free article] [PubMed] [Google Scholar]