Abstract
Background:
Youth in foster care are more likely than non-foster care youth to experience posttraumatic stress disorder (PTSD). While research has identified maltreatment as a risk factor for PTSD, this research remains limited because it tends to only (a) examine a single type or dimension of maltreatment and ignore the polyvictimization and heterogeneity in exposure, and (b) study this relation across a short period time or retrospectively at the end of care.
Objective:
The current study used survival analysis to simultaneously examine the influence of maltreatment characteristics on the risk of receiving a PTSD diagnosis at any time in care following entry into care.
Participants/Setting:
291 youth (Mean age at entry=9.71; 53% female; 49% Black) in foster care and their primary caregivers from a large, Midwestern county.
Methods:
Information on PTSD diagnosis was extracted from Medicaid records, and information on maltreatment and time in care was extracted from case files. Survival analysis was then used to determine the association between maltreatment and risk of PTSD diagnosis.
Results:
When examined independently, each dimension (frequency, severity) of the four maltreatment types was significantly associated with PTSD diagnosis risk (all hazard ratio’s [HR] > 1.00), except sexual abuse frequency. In the comprehensive model with all dimensions examined simultaneously, only neglect frequency for youth entering care in adolescence (HR: 1.13[1.03–1.23]), and neglect severity (HR: 1.27[1.05–1.52]) and emotional abuse frequency (HR: 1.24[1.00–1.53]) for youth entering care pre-adolescence, were associated with PTSD diagnosis risk. Additionally, age of entry into care was associated with PTSD diagnosis risk (HR: 2.34[1.88–2.92]), as adolescents tended to spend fewer days in care before receiving a diagnosis.
Conclusions:
Results suggest that researchers who study PTSD in youth in foster care should consider the entirety of youth’s maltreatment exposure and the context of care to more accurately determine what aspects of youth’s history contributes to receiving a PTSD diagnosis.
Keywords: posttraumatic stress disorder (PTSD), maltreatment, foster care, measurement
Youth in foster care represent a population that tends to demonstrate a disproportionate rate of emotional and behavioral problems, as compared to children in the general population. Estimates across studies suggest that more than 50% of youth in foster care meet criteria for at least one psychiatric diagnosis during childhood (Deutsch et al., 2015; McCrea, 2009; McMillen et al., 2005; Oswald et al., 2010). Among the many difficulties demonstrated by these youth, posttraumatic stress disorder (PTSD) has been of particular importance. Given that youth in foster care are by definition exposed to substantiated maltreatment (i.e., physical, sexual, and emotional/psychological abuse; and neglect), as well as other adverse experiences (U.S. Department of Health and Human Services, 2019), it is not surprising to find higher rates of PTSD in this population compared to their non-foster peers (e.g., Pecora et al., 2009). Childhood prevalence rates of PTSD for youth in foster care are approximately twice as high (approximately 15%) as youth in the general population (approximately 7%; Merikangas et al., 2010; Salazar et al., 2013).
While many children in foster care experience maltreatment and report mental health concerns, there is still a large portion of youth who do not develop PTSD. In an effort to better understand the development of PTSD in youth in foster care and identify youth who may be more likely to receive a PTSD diagnosis, research has sought to identify risk factors associated with a PTSD diagnosis. One such risk factor is the characteristics or dimensions of maltreatment experience(s), including the type, frequency, and severity of these experiences. The current study sought to add to the field of maltreatment research and PTSD by systematically examining each dimension or characteristic of maltreatment exposure prior to entry into foster care in relation to PTSD diagnosis risk while in care using a novel survival analysis approach.
Characteristics of Maltreatment Exposure
Certain characteristics of maltreatment exposure may increase one’s risk for meeting criteria for a PTSD diagnosis, or having increased posttraumatic stress symptoms (PTSS). Importantly, PTSD diagnosis refers to a diagnosis made by a licensed professional according to a specific set of criteria (e.g., Diagnostic and Statistical Manual of Mental Disorders [DSM]), whereas PTSS refer to the presence of one or more symptoms of PTSD. Among the characteristics of maltreatment previously examined in relation to PTSD, type of exposure (i.e., physical, sexual, and psychological abuse; neglect) tends to be the most studied. In comparisons of the different maltreatment types, evidence suggests that youth exposed to sexual abuse are more at-risk to be diagnosed with PTSD, as compared to those exposed to physical abuse, emotional abuse, or neglect (Rock et al., 2018). For example, several studies have found that youth exposed to sexual abuse to tend have greater prevalence rates of PTSD, as compared to youth exposed to other types of maltreatment and neglect (Dubner & Motta, 1999; Maikovich et al., 2009). This may be especially the case for youth who have experienced rape (Salazar et al., 2013).
Although much less studied than type and not widely examined among youth in foster care, maltreatment severity and frequency are two other prominent maltreatment characteristics to consider in relation to PTSD risk (Trickey et al., 2012). In general, the evidence appears to suggest a positive association for severity and frequency of maltreatment and risk of PTSD, such that there is a greater risk of developing PTSS or being diagnosed with PTSD for youth with a high number of or more severe maltreatment experiences. For example, regarding severity, Maikovich et al. (2009) found that harm or severity ratings by caseworkers of their client’s maltreatment predicted high levels of self-reported PTSS in youth referred to Child Protective Services (CPS). Hulette and colleagues (2008) found among preschool age children in foster care that more severe forms of sexual abuse were associated with higher PTSD symptoms scores, compared to those children with less severe forms of sexual abuse. With regard to frequency, Sullivan et al. (2006) found a moderate or higher strength correlation between all types of maltreatment frequency and total PTSD symptom scores in an inpatient adolescent population. Moreover, when examining the influence of maltreatment frequency in relation to PTSD among a sample of high-risk youth, Cecil and colleagues (2017) found that a greater frequency for each type of maltreatment, when each type’s frequency was examined by itself, was positively associated with a higher report of PTSS. However, in general, the characteristics of frequency and severity of maltreatment exposure among youth in foster care are rarely explored in relation to youth’s functioning (e.g., Jackson et al., 2019).
Despite some consistencies within the literature tending to demonstrate an association between maltreatment and diagnosis of PTSD, mixed findings between studies have brought into question what dimensions of maltreatment most accurately predict or influence PTSD diagnosis. For example, there are conflicting findings in the literature regarding type, with some studies indicating that other types of maltreatment (e.g., physical and emotional abuse, and neglect) may increase risk for PTSD and PTSS more than sexual abuse exposure (e.g., Hildyard & Wolfe, 2002; Jackson et al., 2011). Additionally, in contrast to Maikovich et al.’s (2009) findings on maltreatment severity in relation to PTSD symptomology, Dubner and Motta (1999) found no association between sexual abuse severity, or sexual abuse frequency scores, and PTSD diagnosis among youth in foster care. One potential explanation for these conflicting findings could be that past studies have not accounted for polyvictimization or exposure to multiple types or multiple events of maltreatment. Maltreatment rarely occurs in isolation, and it is more often the case more than not that youth experience multiple forms and reoccurring experiences of maltreatment (Collin-Vézina et al., 2011; Turner et al., 2010). However, as with the maltreatment literature at large (Jackson et al., 2014), it is often the case in research on PTSD and maltreatment among youth in foster care that researchers use methods that do not account for polyvictimization. This includes techniques such as grouping youth by “maltreatment type” based on the most recent or most severe exposure and then comparing group means (e.g., Kolko et al., 2010), or examining a single dimension or type of maltreatment in a regression analysis. These approaches bring into question whether there is an accurate representation of youth’s maltreatment history, especially when considering that polyvictimization is the norm.
Evidence from comparing studies examining the relation between maltreatment and PTSD diagnosis and PTSS suggests attention to polyvictimization and the multiple characteristics of maltreatment may explain differences in findings. For example, in contrast to studies finding a significant link between sexual abuse and PTSD when examining this single type of exposure in isolation (e.g., Maikovich et al., 2009), Van Vugt et al. (2014) found no association between sexual abuse severity scores and PTSD symptomology in youth in foster care when they accounted for youth’s polyvictimization by including the severity score for all types of abuse in the same model. In this case, the authors found instead that psychological or emotional abuse was a consistent predictor of PTSD symptoms. Similarly, Rayburn et al. (2016) and Vanderminden et al. (2019) found that after accounting for other types of maltreatment in the same model, certain forms of maltreatment, such as sexual abuse, were no longer predictive of PTSS. Overall, evidence from studies examining PTSD appear to suggest that there is a need to account for polyvictimization and the multitude of maltreatment characteristics when examining the relation between maltreatment and PTSD among youth in foster care, which may help provide a more accurate estimation of the relation between maltreatment and PTSD.
Timing of PTSD Analysis
In addition to maltreatment characteristics, another explanation for mixed findings in the maltreatment/PTSD diagnosis risk association is the time frame of the study. One approach to research on PTSD among youth in foster care is examining lifetime prevalence of PTSD, which often involves examining PTSD in youth aging out of care or among adults who were previously in foster care. For example, Keller and colleagues (2010) assessed for PTSD history in late adolescence-aged youth in foster care in relation to trauma exposure and found a higher lifetime percentage of meeting criteria for PTSD, over other depressive and substance use disorders. Alternatively, other studies will only examine the influence of maltreatment and other risk factors on PTSD or PTSS over a short period of time, such as a period of a few years while in care. For example, Yoon et al. (2018) tracked the trajectory of PTSS in system involved youth (not removed from their homes) over a three year period, finding that there was an overall decrease in PTSS over time for girls and not boys, and that sexually abused victims had slower declines in PTSS, as compared to the other maltreatment types.
While these study designs provide important information about PTSD in relation to maltreatment and other risk factors, the general nature of PTSD symptomology over time and the complexity of youth’s experiences in foster care suggest that using either a lifetime prevalence retrospective approach, or a prospective but short time frame approach, may miss important information on the nature or development of PTSD. What is less understood is the long-term trajectory of the development of PTSD. Evidence suggests that the trajectory of PTSD does not remain stable or linear over time, as studies have shown that there tends to be a typical, rapid decline in PTSD symptoms over time. For example, in a study of system involved youth as part of the National Survey for Child and Adolescent Well-Being (NSCAW), it was reported that 91% of youth who scored in the clinically significant range for PTSS at baseline referral were in the normal or borderline range at a three year follow up (McCrea, 2009). Additionally, compared to other mental health and substance use problems, Keller et al. (2010) found that PTSD has the lowest age of onset, PTSD diagnoses did not increase in adolescence, and a relatively equal number of children demonstrated PTSD symptoms before entering care compared to after entry. Taken together, these findings suggest that the timing of when PTSD diagnosis is examined matters and that only examining a small portion of youth’s life while in care with regard to PTSD may not produce an accurate indication of the full trajectory or change of PTSD symptomology over time. Moreover, given the non-linear trajectory of PTSD and PTSS, this may indicate that the entirety of youth’s time in care should be considered to obtain a better understanding of when and why some youth may receive a PTSD diagnosis. No studies to date have examined changes in risk across a long period of time for youth in foster care.
These findings are further complicated among youth in foster care given the shift in youth’s lives that occur when they enter foster care, which could influence the trajectory of PTSS and risk of being diagnosed with PTSD. Although youth who enter into care may already be experiencing symptoms or meet criteria for PTSD (Keller et al., 2010), entry into care can be a significant or even traumatic life experience for this population because of many potential personal, social and environmental challenges, which may influence symptoms (Barber et al., 2001; Mitchell & Kuczynski, 2010; Wechsler-Zimring et al., 2012). Additionally, youth who enter foster care become eligible for Medicaid services through the state, most commonly through Title IV-E eligibility, which provides them access to various medical and psychological services that may influence the potential of receiving a PTSD diagnosis. In sum, there is evidence to support the need to consider PTSD trajectory across youth’s time in care from first entry into care, as the significant changes in youth’s lives at this time may shape their risk of being diagnosed with PTSD.
Current Study
To address the identified gaps in the literature, the current study examined the trajectory of risk for PTSD diagnosis in youth in foster care using a survival analysis approach. This type of approach is useful when there is time-to-event data, or known start and stop dates about the length of time until an event happens, and this approach can manage data where an event of interest does not occur or participants are “lost” before the end of the study (Tabachnick et al., 2019). Given that information on the dates of youth’s placement into care and PTSD diagnoses are recorded in case file and Medicaid claims data information, this provides a unique opportunity to examine the timeline of youth’s mental health problems while in care. Thus, the primary goal of the current study was to comprehensively and simultaneously examine how each dimension of maltreatment (type, severity, and frequency) contributed to the risk of PTSD diagnosis across youth’s complete time in foster care from a similar starting point (i.e., entry into care) and similar set of exposure (i.e., maltreatment prior to entry into care) for each youth. This is in contrast to previous studies on PTSD diagnosis and maltreatment that only look a single type or dimension of exposure, or only examine a few years. It was hypothesized that frequency and severity of sexual abuse would be associated with risk of PTSD diagnosis. Given the minimal and mixed research on the dimensions of other types of maltreatment (physical abuse, emotional abuse, neglect), especially when examined simultaneously, no specific hypotheses were made about these dimensions for the other maltreatment types.
Methods
Participants
Participants included 291 youth enrolled in foster care in a large Midwestern city, and their foster caregivers. To be included in the study, youth had to be at least eight-years-old and living with the reporting caregiver in foster care for at least 30 days prior to study enrollment. Youth who had received a prior diagnosis of intellectual disability or autism spectrum disorder were excluded from the larger project due to the larger project’s demands of data collection procedures, necessity of youth self-report, and the use of measures in the larger project that not been validated in samples of youth with cognitive challenges. Upon entry into the larger project, youth were on average 13.30 (SD = 2.95, range: 8–18) years old. On average, youth had entered care at age 9.71 (SD = 4.37), wherein the youngest age of entrance into care was at birth and oldest age was age 17. Fifty-two percent of participants were female, with 49.48% self-identified as Black, 32.75% as White, 11.15% as Multiracial, and 6.62% as another race/ethnicity. At entry into the larger study, 53% resided in traditional foster home settings and 47% resided in congregate foster care settings (e.g., group home settings).
Measures
Demographics and Placement.
Youth and foster caregivers provided demographic information, including the youth’s age, gender, and race/ethnicity. In the current study, gender and ethnicity were examined in relation to PTSD diagnosis given previous evidence demonstrating differences in PTSD presentation and mental health service utilization among youth involved in the foster care system (e.g., Jackson et al., 2011; Villegas & Pecora, 2012). The state Department of Social Services (DSS) provided information on the date of youth’s first entry into care and the date of their last day in care. This information was then used in conjunction with the child’s date of birth to calculate the amount of time in placement before receiving a PTSD diagnosis. Additionally, age at placement into care was calculated using the child’s date of birth and date of first entry into care, which was also converted into a categorical variable to represent infancy (ages 0 to < 3), preschool (ages 3 to < 6), school-age (ages 6 to < 13), and adolescence (ages 13 to 18).
Maltreatment.
DSS provided case files for all participating youth. Maltreatment from each case file was coded using the Modified Maltreatment Classification System (MMCS; English & the LONGSCAN Investigators, 1997). The MMCS has been used in numerous studies of maltreatment and is a valid and reliable method for capturing both frequency and severity of abuse and neglect incidents experienced by youth (English et al., 2005a; Litrownik et al., 2005). All maltreatment incidents were coded by trained and reliable coders (i.e., coders obtained a kappa reliability of .80 to ensure interrater reliability and consistency with the MMCS coding) from the reporter narratives in the case file. All reports that involved maltreatment directed at the participant were coded, including those not investigated as well as those substantiated by DSS. For a complete review on the case file coding method, see Huffhines et al. (2016).
Using the MMCS, the coder first determined the maltreatment type (i.e., physical, sexual, emotional/psychological, physical neglect, or supervisory neglect) for each incident specified in the case file narratives, as well as the number of total maltreatment incidents in the youth’s case file (i.e., frequency of maltreatment). The severity of each maltreatment incident was also coded using the MMCS, which specifies severity by the quality and time period of the incident. For example, a mild severity rating (MMCS severity coding of 1) for an incident of neglect would include lack of supervision of the child while at home for a few hours, whereas a more severe rating (MMCS severity code of 4) for an incident of neglect would include a child being left alone overnight. Thus, the current study included type, frequency, and severity of maltreatment. Further, only maltreatment incidents that occurred prior to entry into foster care were included. In addition to overall maltreatment, developmental stages where maltreatment exposure occurred were also computed in line with previous research on chronicity of exposure across age (English et al., 2005b). Developmental stages were classified as follows: infancy (ages 0 to < 3), preschool (ages 3 to < 6), school-age (ages 6 to < 13), and adolescence (ages 13 to 18). Number of developmental stages in which maltreatment occurred were then summed. For instance, if a youth experienced a maltreatment incident in infancy, two incidents in preschool, and an incident in adolescence, they would have a score of three.
PTSD Diagnosis.
All youth were enrolled in Medicaid as their primary medical provider. The Medicaid claim records for each youth was provided by DSS to determine psychiatric and medical history of each participant, including diagnosis and date of diagnosis. Medicaid claims files have been widely used as a measure of mental and physical health concerns in low income and foster care populations (e.g., Lucenko et al., 2015; Huffhines & Jackson, 2019). Moreover, research has determined the reliability of information in youth’s Medicaid claims files for documenting physical and mental health concerns for research purposes (e.g., Knapp et al., 2006; Cummings et al., 2017). Diagnoses were based on DSM-IV and DSM-5 diagnostic criteria and were made by a trained healthcare provider, such as a licensed psychologist, psychiatrist, or social worker, as reported in the Medicaid claim records.1 For the current study, presence of PTSD was coded as 1 = “diagnosis” and 0 = “no diagnosis” if a diagnosis of PTSD occurred any time after entry into foster care, which was indicated in the Medicaid file by (a) an International Classification of Diseases (9th Revision [ICD-9-CM]) code for PTSD and (b) the date diagnosis of PTSD being after the date of entry into care for the child. Time to PTSD diagnosis was calculated by subtracting the date of entry into foster care from the first date of the PTSD diagnosis indicated in the Medicaid claims record.
Procedures
Participants were recruited from a large Midwestern county on behalf of a larger study, the SPARK (Studying Pathways to Adjustment and Resilience in Kids) project, which is a federally funded longitudinal research initiative on the mental, physical, and academic functioning of youth placed in foster care. The project worked with the DSS for the county, who provided the project with contact information for approximately 2700 youth who may have been eligible to participate. Using this contact information, foster caregivers and youth were recruited through multiple methods, including direct mailings and phone calls. In addition to these direct contacts, advertisements for the project were placed in newsletters and list-serves for foster families, and recruitment booth were used at community events for foster care families and congregate care centers. Referrals from prior SPARK participants were also used. The sample obtained through these recruitment strategies was demographically representative of the larger population of youth in foster care in the county. DSS provided formal consent for all youth to participate in the SPARK project and granted access to youths’ case files, Medicaid claims records, and placement records. Youth and their foster caregivers were fully informed about the purpose and nature of the study, as well as limits to confidentiality (i.e., suicidality, homicidality, current child abuse or neglect). Consent was obtained from foster caregivers and assent obtained from youth.
In addition to youth’s case file information, youth and caregivers completed demographics and additional study questionnaires through an audio-computer assisted self-interview (ACASI) program on project laptops. Additional study questionnaires not included in the current paper included items related to youth coping, appraisal, social support, and internalizing and externalizing symptoms. The ACASI program presents items on a computer screen and reads questions aloud via headphones, thus improving privacy and confidentiality and allowing those who need additional reading support to better understand the material. Both youth and their caregivers were compensated for their time and participation. For more information on the SPARK project, including details on recruitment strategy, informed consent, data collection procedures, and maintenance of participant confidentiality and safety, see Jackson et al. (2012). The SPARK Project was approved by both the university Institutional Review Board and DSS.
Data Analysis
All statistical analyses were conducted in R (R Core Team, 2014). To examine the trajectory of PTSD diagnosis in youth in foster care, each model used the time from the day the youth first entered care to the date of diagnosis of PTSD, representing a right censored dataset. First, the current study used a Kaplan–Meier survival analysis to examine group differences in survival rate among youth in foster care according to gender (male vs. female), ethnicity (Black, White, and another race/ethnicity), age of placement into foster care (infancy vs. preschool vs. school age vs. adolescence), maltreatment status (maltreated vs. non-maltreated), and developmental periods experiencing maltreatment (none vs. one vs. two vs. three periods). These distinctions between groups are similar to other studies examining demographics variables in relation to maltreatment or mental health functioning among youth in foster care (e.g, English et al., 2005a; 2005b), as well as for the purpose of closely examining the covariates included in the models later on with the maltreatment dimensions. Differences between the trajectories of each curve were examined using a log-rank test following a chi-squared distribution. Second, Cox proportional hazard regression was utilized to estimate the influence of maltreatment variables on days until diagnosis. This was first completed with the whole sample looking at each dimension individually, as a means of comparing this study to previous research that does not account for all of youth’s maltreatment history. In the second part, all dimensions were examined simultaneously into a model with the entire sample, as well as separated by pre-adolescent and adolescent youth. The influence of the variables of interest in the Cox proportional hazard regression analyses were examined using the significance and 95% confidence intervals of the hazard ratios [HR] estimates. In the full models with all maltreatment dimensions, gender, ethnicity, age of entry into care, and maltreatment across developmental periods were includes as covariates.
Results
The means, standard deviations, and ranges for the continuous variables in the analyses are presented in Table 1. The sample included 77.66% diagnosed with PTSD while in foster care during the duration of their time in care. On average, youth received a PTSD diagnosis 1,301 days (3.56 years) after entering care, with one day being the minimum number of days and 6584 (18.04 years) days being the maximum number of days after entering care to receive a PTSD diagnosis. Based on the youth’s case file, neglect was the most prevalent or most frequent type of abuse (i.e., highest reported mean number of events), followed by physical abuse, and then emotional abuse and sexual abuse. Overall, 65.03% of youth had experienced at least one event of maltreatment prior to entry into care according to their case file records. The remaining proportion of youth (34.97%) had reports in their care file of abuse of another child in the same home or living situation, or a non-maltreated related threat to their well-being prior to entry, which may have been associated with their placement into foster care. Among those who experienced maltreatment prior to entry into care, 39.86% of youth experienced physical abuse, 51.89% experienced neglect, 35.05% experienced emotional abuse, and 14.77% experienced sexual abuse. Polyvictimization was common in the sample. The most common form of polyvictimization was for both physical abuse-neglect and emotional abuse-neglect (30.24%), followed by physical abuse-emotional abuse (23.02%), sexual abuse-neglect (9.62%), physical abuse-sexual abuse (8.25%), and then sexual abuse-emotional abuse (5.84%). Moreover, among those who experienced maltreatment, 21.43% experienced maltreatment during only one developmental period, 35.20% experienced maltreatment in two different developmental periods, and 43.37% experienced maltreatment in three different developmental periods.
Table 1.
Sample Descriptive Statistics
| Total Sample (N=291) | Infant EC (n=19) | Preschool EC (n=33) | School-age EC (n=148) | Adolescent EC (n=93) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean(SD) or % | Min-Max | Mean(SD) or % | Min-Max | Mean(SD) or % | Min-Max | Mean(SD) or % | Min-Max | Mean(SD) or % | Min-Max | |
| Demographics | ||||||||||
| % Female | 52.96% | 58.82% | 51.52% | 56.25% | 47.31% | |||||
| Ethnicity | ||||||||||
| Black | 49.48% | 64.71% | 39.39. | 59.72% | 34.41% | |||||
| White | 32.75% | 17.64% | 48.48% | 26.39% | 39.78% | |||||
| Other | 17.77% | 17.64% | 12.12% | 13.89% | 25.80% | |||||
| Maltreatment Dimensions | ||||||||||
| Physical Abuse Frequency | 1.5 (2.79) | 0–22 | . 11 (.46) | 0–2 | .49 (1.28) | 0–6 | 1.65 (2.94) | 0–22 | 2.02 (3.07) | 0–13 |
| Physical Abuse Severity | .70 (.98) | 0–5 | .21 (.92) | 0–4 | .42 (.95) | 0–4 | .75 (1.01) | 0–5 | .82 (.91) | 0–3 |
| Sexual Abuse Frequency | .33 (1.09) | 0–10 | NR | NR | .15 (.57) | 0–3 | .30 (.98) | 0–8 | .45 (1.32) | 0–10 |
| Sexual Abuse Severity | .57 (1.44) | 0–6 | NR | NR | .44 (1.49) | 0–6 | .53(1.35) | 0–5 | .77 (1.64) | 0–6 |
| Emotional Abuse Frequency | .70 (1.26) | 0–7 | .05 (.23) | 0–1 | .55 (.79) | 0–2 | .75 (1.37) | 0–7 | .79 (1.32) | 0–7 |
| Emotional Abuse Severity | 1.00 (1.56) | 0–5 | .26 (1.14) | 0–5 | 1.23 (1.77) | 0–5 | 1.05 (1.61) | 0–5 | .97 (1.47) | 0–5 |
| Neglect Frequency | 1.95 (2.90) | 0–17 | .47 (1.12) | 0–4 | 1.21 (1.81) | 0–7 | 2.22 (3.00) | 0–13 | 2.14 (3.22) | 0–17 |
| Neglect Severity | 1.11 (1.34) | 0–5 | .29 (.59) | 0–2 | .96 (1.28) | 0–4 | 1.12 (1.26) | 0–5 | 1.33 (1.51) | 0–5 |
| % with Maltx prior to EC | 65.03% | 26.32% | 54.55% | 68.75% | 72.04% | |||||
| PTSD/Foster CareVariables | ||||||||||
| Age at EC | 9.71 (4.37) | 0–17 | 1.05 (.91) | 0–2 | 4.12 (.93) | 3–5 | 8.94 (1.85) | 6–12 | 14.66 (1.25) | 13–17 |
| % with Diagnosis | 77.66% | 78.95% | 78.78% | 86.56% | 61.47% | |||||
| Days from EC to PTSD Diagnosis (in days) | 1300.82 (14. 0.34) | 1–6584 | 3852.79 (1987.83) | 316–6584 | 2565.58 (1759.79) | 63–5591 | 1131.82 (1042.50) | 4–4338 | 582.27 (558.81) | 1–2245 |
| In years | 3.56 | 10.56 | 7.03 | 3.10 | 1.60 | |||||
Descriptive information is provided for the entire sample, as well as separated by the age at which children entered into foster care (EC). NR= No record of experience. PTSD= Posttraumatic stress disorder. Matlx= Maltreatment. EC= Entry into foster care.
Kaplan–Meier Survival Analysis
A Kaplan–Meier survival analysis was conducted to determine differences in diagnosis risk among the sample based on group differences. This included examination of demographic and control variables (gender, ethnicity, age of entry into care, maltreatment across developmental stages), as well as the grouping of maltreatment dimensions. In the first comparison, the log-rank test of the Kaplan–Meier survival analysis for gender demonstrated a non-significant difference (χ2(1, 287) = .20, p = .67), suggesting that males and females did not differ on PTSD diagnosis trajectory. The comparison in survival function between ethnicity (Black, White, and Other) demonstrated a non-significant difference (χ2(2, 287) = 1.80, p = .40). Additionally, the Kaplan–Meier survival analysis for experiencing maltreatment across developmental stages for those youth who experienced maltreatment prior to entry into care demonstrated a non-significant difference (χ2(3, 174) = 6.50, p = .09), suggesting that there was no difference in PTSD diagnosis trajectory among youth who experienced maltreatment across one or more developmental periods prior to entry into care.
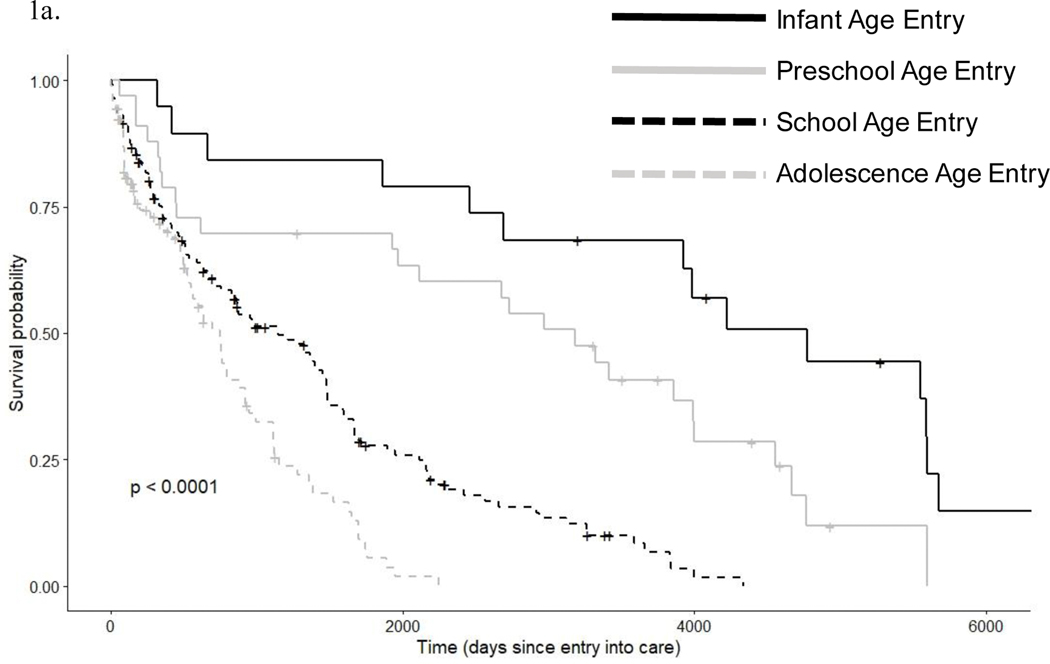
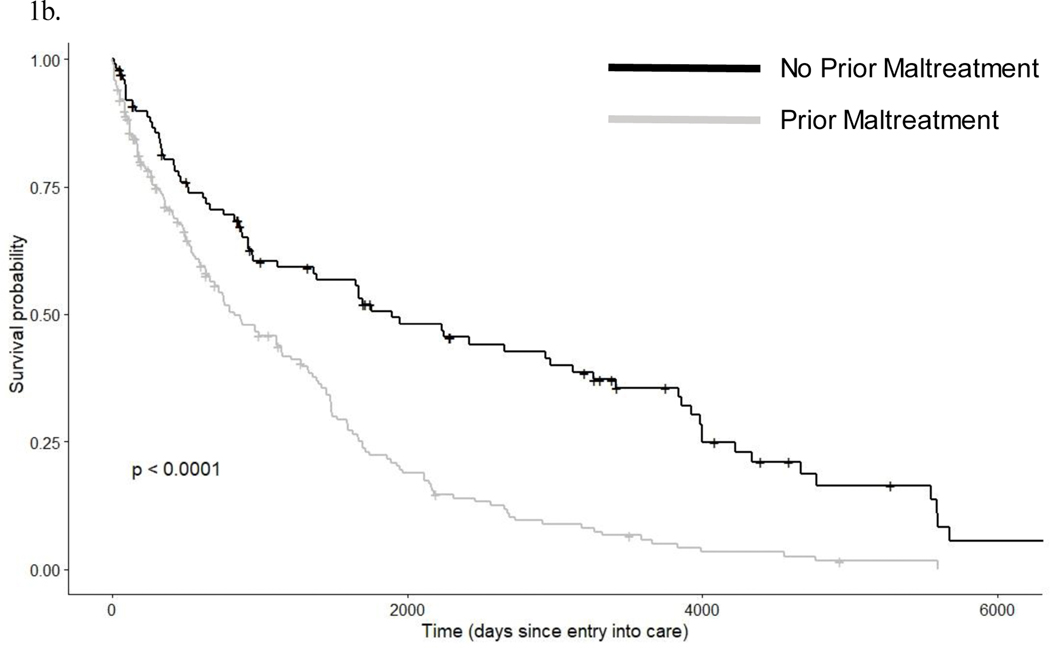
The log-rank test of the Kaplan–Meier survival analysis revealed a significant difference (χ2(3, 289) = 70.80, p < .01) in PTSD diagnosis trajectory between youth placed in foster care in infancy (ages 0 to < 3), preschool (ages 3 to < 6), school-age (ages 6 to < 13), and adolescence (ages 13 to 18), which is shown in Figure 1a. The results suggest that as age of entry into care increases from infancy to adolescence, the fewer days in between entry to care and receiving a PTSD diagnosis. In other words, upon entry into care, adolescents tend to receive a PTSD diagnosis after fewer days into care, as compared to school age and younger youth who enter foster care. Maltreatment status revealed a significant difference for PTSD diagnosis risk (χ2(1, 291) = 29.10, p < .01; Figure 1b), such that youth who entered care with previous maltreatment were more likely to receive a PTSD diagnosis fewer days into care, as compared to youth with no previously reported maltreatment.
Figure 1. Survival plots from Kaplan–Meier survival analysis for grouping based on age of entry into care and maltreatment status.
Time is measured in days since first entry into care. These figures show the change in survival probability (i.e., estimated percent chance that a youth does not have a PTSD diagnosis) across time in care for age of entry into care (Figure 1a) and maltreatment status (Figure 1b). For example in Figure 1b, there is around a 50 % chance that a child who entered care with no previous history of maltreatment exposure will have a PTSD diagnosis after spending 2000 days in care.
Cox Proportional Hazard Regression
The variables of the maltreatment dimensions and other potential risk factors associated with foster care were analyzed using Cox proportional hazard regression. A series of hierarchical Cox proportional hazard regressions were conducted to examine the variables of interest. In the first part, a model with only a single maltreatment variable was examined with the whole sample to simulate previous research not accounting for polyvictimization. In the second part, three full models with all predictors were calculated. This included using the whole sample, as well as looking separately at children who entered care pre-adolescence (i.e., children < 13 years) and those who entered into care during adolescence to take into consideration potential developmental differences. This was also based on the observed differences in diagnosis previous identified from age of entry into care from the Kaplan–Meier survival analysis above. In the adolescent model, gender and ethnicity were included in the model as covariates. In the pre-adolescent model, gender and ethnicity were included in the model as covariates, as well as the maltreatment across developmental stages variable since this group included the infancy, preschool, and school age youth. In the full model, gender, ethnicity, maltreatment across developmental stages, and age at entry into care were included as covariates. Results for the models, including hazard ratio (HR) estimates, are presented in Table 2.
Table 2.
Survival Analysis Results for Risk of PTSD Diagnosis
| Adolescent Model | Pre-Adolescent Model | Full Sample Model | ||||||
|---|---|---|---|---|---|---|---|---|
| Predictors | Hazard Ratio | 95% CI | Predictors | Hazard Ratio | 95% CI | Predictors | Hazard Ratio | 95% CI |
| PA Frequency | 1.04 | .95–1.14 | PA Frequency | 1.05 | .94 –1.17 | PA Frequency | 1.02 | .95–1.10 |
| SA Frequency | 1.14 | .85–1.53 | SA Frequency | 1.03 | .74–1.43 | SA Frequency | 1.01 | .83–1.24 |
| EA Frequency | .84 | .57–1.25 | EA Frequency | 1.24** | 1.00–1.53 | EA Frequency | 1.03 | .85–1.23 |
| NFrequency | 1.13* | 1.03–1.23 | N Frequency | 1.06 | .98–1.15 | N Frequency | 1.10* | 1.03–1.15 |
| PA Severity | .84 | .58–1.21 | PA Severity | 1.03 | .82–1.30 | PA Severity | .92 | .75–1.11 |
| SA Severity | .97 | .76–1.24 | SA Severity | 1.00 | .83–1.21 | SA Severity | 1.03 | .90–1.18 |
| EA Severity | 1.36 | .99–1.86 | EA Severity | .94 | .80–1.11 | EA Severity | 1.07 | .94–1.23 |
| N Severity | .89 | .72–1.10 | N Severity | 1.27** | 1.05–1.52 | N Severity | .98 | .85–1.12 |
| Gender | 1.17 | .69–1.98 | Gender | .86 | .57–1.31 | Gender | 1.01 | .76–1.35 |
| Ethnicity | .81 | .57–1.16 | Ethnicity | .97 | .69–1.37 | Ethnicity | .92 | .75–1.14 |
| Maltx Aross Dev | 1.27 | .98–1.63 | Maltx Aross Dev | 1.00 | .88–1.15 | |||
| Age of EC | 2.34* | 1.88–2.92 | ||||||
p < .05.
In the independent models, only the one maltreatment dimension was included in the model. PA= Physical Abuse, SA= Sexual Abuse, EA= Emotional Abuse, N= Neglect. Maltx Across Dev = Experiencing maltreatment across developmental periods. Age of EC= Age of first entry into foster care. N = 291
First, the separate models were created and examined with each dimension of maltreatment included independently. These models did not include covariates, including gender and ethnicity, again as a test for examining the influence of each predictor when not accounting for other maltreatment dimensions or factors. In each of their own independent models, the following variables were significantly associated with PTSD diagnosis risk: Physical abuse severity (HR = 1.19, 95% CI = 1.06–1.35, p < .01), sexual abuse severity (HR = 1.10, 95% CI = 1.01–1.20, p = .03), emotional abuse severity (HR = 1.11, 95% CI = 1.03–1.20, p < .01), neglect severity (HR = 1.21, 95% CI = 1.10–1.33, p < .01), physical abuse frequency (HR = 1.08, 95% CI = 1.03–1.13, p < .01), emotional abuse frequency (HR = 1.19, 95% CI = 1.07–1.32, p < .01), and neglect frequency (HR = 1.10, 95% CI = 1.06–1.15, p < .01). Sexual abuse frequency was marginally significant (HR = 1.11, 95% CI = .99–1.24, p = .07). For all these predictors, the hazard ratio was significantly (or marginally significant for sexual abuse frequency) greater than one, indicating that the predictors were associated with an increase in PTSD diagnosis risk over time as frequency or severity of each maltreatment type increased when the predictors were examined in their own independent model.
Next, the three full models with all predictors and covariates were examined for the pre-adolescent and adolescent subgroups. In these full model, all of the frequency and severity scores for each maltreatment type were entered and examined simultaneously, along with the covariates for each model. The global chi-square test for the model was not significant for either model (pre-adolescent model: χ2(11, 131) = 14.76, p = .19; adolescent model: χ2(10, 93) = 9.36, p = .50; full model: χ2(12, 224) = 20.36, p = .06), indicating that the assumption of proportionality was not violated. In the pre-adolescent model, there were only two maltreatment dimensions associated with PTSD diagnosis risk, which included emotional abuse frequency (HR= 1.24, 95% CI: 1.00–1.53, p < .05) and neglect severity (HR= 1.27, 95% CI: 1.05–1.52, p < .05). In the adolescent model, the only maltreatment dimension associated with PTSD diagnosis risk was neglect frequency (HR= 1.13, 95% CI: 1.03–1.23, p < .05). None of the covariates were significantly associated with PTSD diagnosis risk in either model. In the model with the entire sample, only neglect frequency (HR= 1.09, 95% CI: 1.03–1.53, p < .05) and age at placement into care (HR= 2.34 95% CI: 1.88–2.92, p < .05) were associated with PTSD diagnosis risk.
Discussion
Youth in foster care tend to experience a more maltreatment compared to youth in the general population, and it is therefore important for researchers to understand how maltreatment may contribute to the risk of mental health concerns. The current study attempted to add to the field’s understanding of one such mental health concern, PTSD, by examining how youth’s maltreatment history prior to entry in foster care may put these youth at greater risk for receiving a PTSD diagnosis while in care. This was completed by using a survival analysis approach with Medicaid and case file data to examine the this risk trajectory of PTSD diagnoses in relation to maltreatment experienced prior to entry into care across youth’s time in care from entry to time of receiving a diagnosis. These findings build upon a limited literature base exploring how the specific characteristics of maltreatment (i.e., type, frequency, and severity) exposure prior to entry into care may influence what youth receive a PTSD diagnosis after entering care. Moreover, the present study provided information on how important aspects of youth’s foster care experience (i.e., developmental stage at entry into care) was associated with the risk for later PTSD diagnosis.
Although almost every dimension of maltreatment was significantly associated with risk for diagnosis of PTSD when examined individually in separate models, the findings were notably different when the dimensions were examined simultaneously. When examined together in the same model, most of the dimensions of exposure did not significantly increase or decrease the risk of receiving a PTSD diagnosis. The most consistent type of exposure associated with a greater risk of PTSD diagnosis was neglect, as neglect frequency was associated with PTSD risk in the overall model and adolescent model, and neglect severity was associated with risk in the pre-adolescent model. Although somewhat surprising that neglect was the only type of maltreatment associated with risk of PTSD diagnosis, experiences of neglect in themselves can be perceived as traumatic for youth, which could in turn be associated with persistent anxiety and stress, poor ability to regulate these emotions, and the development of PTSD symptomology (Bellis et al., 2009; Hildyard & Wolfe, 2002). Moreover, past studies have shown that neglected children display more PTSD symptoms than non-neglected children (e.g., Milot et al., 2010), and that childhood neglect is associated with PTSD symptoms in adulthood (Koenen & Widom, 2009). However, these findings build on this past research by demonstrating neglect (including both frequent and severe neglect) may still have a unique influence on PTSD risk, even when taking into account all other experiences of maltreatment and that this may hold across childhood.
It was also found that emotional abuse frequency was associated with a greater risk for PTSD diagnosis in a fewer amount of days for children entering care younger than 13. These findings extend on similar research conducted by Cecil et al. (2017) with non-foster care high risk adolescents, and Van Vugt et al. (2014) with adolescents and young adults involved in child welfare, showing that emotional abuse may contribute to PTSD and PTSS even when accounting for other types of maltreatment the same model. These findings also provide evidence that this may be the case for younger children as well. Although emotional abuse may not serve a primary traumatic event, the negative influence of emotional abuse, in combination with its high prevalence in conjunction with other forms of maltreatment, may significantly contribute to the demonstration of PTSS and thus increase risk for receiving a PTSD diagnosis (Norman et al., 2012). For example, in a network analysis of PTSD symptoms and different types of trauma in adults who were in foster care, Glück et al. (2017) found that several forms of emotional abuse had the most centrality as compared to other forms of trauma, and were significantly associated with PTSD symptoms, suggesting that emotional abuse may be particularly important in the development of PTSD and PTSS.
In contrast to previous research and the study’s hypothesis (e.g., Maikovich et al., 2009), sexual abuse specifically (including both frequency and severity of experiences) did not appear to be more predictive of a PTSD diagnosis risk when examined simultaneously and taking into account the influence of youth’s complete maltreatment history. This finding may have been associated with the approach used in the current study to examine all maltreatment dimensions together, as the results of the current study are similar to that of studies such as Van Vugt et al. (2014) and Cecil et al. (2017), who also found no direct association between sexual abuse and PTSD when including other types of abuse in the same model. This is in contrast to other research on sexual abuse and PTSD that examined and found certain maltreatment dimensions to be associated with PTSD diagnosis when analyzing these aspects of youth’s maltreatment experience in isolation (e.g., Maikovich et al., 2009). This includes using techniques such as grouping youth into a certain maltreatment group based on the most recent or most prevalent type of maltreatment exposure, or examining the influence of each dimension in independent analyses that do not take into account youth’s complete maltreatment history.
As with other research examining the potential influence of maltreatment as a whole on youth’s functioning (e.g., McGuire & Jackson, 2018), the findings of the current study for the individual and comprehensive models illustrate that using grouping methods or single dimension approaches only in analyses and not taking in account all of youth’s maltreatment history and characteristics may lead to inaccurate findings and thus inaccurate conclusions about the role of maltreatment. When examined in a separate, independent models, almost all the maltreatment dimensions for all the four types (except sexual abuse frequency) were significantly associated with a greater PTSD diagnosis risk than those youth with lower amounts of these experiences. Further, youth with any history of maltreatment prior to entry into care, as compared to no maltreatment, demonstrated a higher risk of PTSD diagnosis. While these findings may suggest that cumulative maltreatment increases risk, this can be misleading because in the full model that took into account all other types of maltreatment, the majority of these significant associations with PTSD diagnosis risk were no longer observed. Taken together, the results point to the need to consider the complex nature of youth’s maltreatment history by examining and accounting for the many aspects of the different types of experiences when attempting to determine whether maltreatment is associated with youth’s functioning. This also suggests that it may not be accurate to make broad statements about “maltreatment” contributing to poor functioning when it may actually be unique aspects of these experiences that matter. Additionally, these findings build on related research demonstrating the importance of accounting for exposures that may not be typically considered Criterion A events according to DSM definitions when examining PTSD diagnoses, as it was neglect and emotional abuse (not physical abuse or sexual abuse) that were primarily associated with PTSD diagnosis risk (e.g., Anders et al., 2012; Lansing et al., 2017). Moreover, this may be even more important in samples of youth in foster where there is often polyvictimization and high rates of exposure to neglect and emotional abuse.
In addition to demonstrating the need to take into account the complexity of youth in foster care’s maltreatment experiences, the current study also demonstrates the importance of taking into account aspects of youth’s foster care experience specifically in relation to PTSD, as opposed to simply focusing on maltreatment. Of the various predictors of risk for PTSD diagnosis examined in the current study beyond maltreatment specifically, age of entry into care was a significant predictor. Even when taking into account maltreatment history and other factors associated with PTSD (e.g., gender, ethnicity) in the full models, age of entry into care was still significantly associated with PTSD diagnosis risk. These results suggest that the older a youth enters care, the fewer days in care the youth spends before they receive a PTSD diagnosis on average. The number of days did decrease as children entered care at an older age, moving from 3853 days or 10.56 years for children entering care in infancy to 582 days or 1.60 years for youth entering during adolescence. There are a few potential explanations for this finding. Follow up analyses indicated that while there was evidence of a small increasing trend in age of entry into care and maltreatment exposure (r = .20), the school-age group had the most youth with maltreatment exposure. Taken together with the findings that maltreatment exposure may put youth at more risk of a PTSD diagnosis, age and exposure may explain part but not the entirety of these findings. Another possibility is that adolescents may be diagnosed with PTSD more than younger youth because of symptom presentation. For example, adolescents tend to demonstrate more externalizing concerns, such as aggression and anger associated with PTSD (Contractor et al., 2013), than younger youth with PTSD. Externalizing symptoms such as these may be more disruptive or noticeable than internalizing symptoms, which in turn could lead to more referrals for assessment or treatment services. Further, school age children examined for PTSD symptomology may not have met criteria given that evidence suggests certain PTSD criteria are underreported in school age children as compared to adolescents, and that school age reports often rely on caregiver report which may not be as reliable in foster care youth (Scheeringa et al., 2006).
When considering longitudinal studies of youth in foster care’s functioning, it may be necessary to examine development from the time youth enter care and across their entire time in care, as the current study did. This is in contrast to previous studies examining PTSD symptomology/diagnosis, which only examined a short period of youth’s lives or looked at lifetime diagnosis, including adulthood. Only examining a short period in time may be problematic as the current study demonstrates. For the overall sample, the number of days in care from entry into care to PTSD diagnosis was on average 1301 days or 3.59 years, and ranged from approximately one day to 18 years. Further, with regard to the pattern of risk, there was a tendency for risk of PTSD diagnosis to drop after the first year and a half across all ages of entry. Most studies looking at change in PTSD diagnosis or symptomology over time tend to look at periods of one to three years (e.g., McCrea, 2009; Yoon et al., 2018). If researchers are only looking at a single part of youth’s time in care, they may find significantly different results depending on the part they are examining. For example, it may be the case that one would observe significant decrease in PTSD risk if looking at the first year in care, whereas one might assume risk for PTSD diagnosis is fairly stable across time if looking at trajectories after the first two years in care. Furthermore, entry into care for youth can be a significant life experience, and for some youth this can be considered a traumatic event (Wechsler-Zimring et al., 2012), in addition to the multitude of environmental factors in a child’s life that change at this time. Thus, all of these factors together may influence the trajectory of PTSD diagnosis, suggesting that researchers should consider entry into care as an important point in youth’s life when considering how functioning may change over time.
Limitations
The results should be interpreted in light of the study’s limitations. One limitation was that the study could not account for unreported maltreatment or non-maltreatment potentially traumatic experiences (PTEs) that may be associated with PTSD (e.g., Cho & Jackson, 2016). However, given that dates and details of youth’s maltreatment history was needed for the survival analysis, case file data was the most viable option as it would be difficult to determine how recall bias might interfere with youth’s ability to report on dates and details of these other past experiences (Hulme, 2004). Further, given the approach used in the current study, possible maltreatment and other PTE exposure occurring after entry into care was not included. Although rates may be lower after entry compared to before entry into foster care, previous research has shown these youth may continue to experience maltreatment and PTEs after entry into care, and that more maltreatment exposure prior to entry into care may increase the risk of experiencing more maltreatment while in care (e.g., Font, 2015; Katz et al., 2017). These experiences could influence the potential risk of receiving a PTSD diagnosis. If appropriate data is available on this type of information (e.g., dates of maltreatment or PTE exposure), future studies should consider examining how post-entry maltreatment or PTE exposure, as well as comparing how pre- or post-entry exposure, may contribute to PTSD diagnosis risk.
Additionally, this study was not able to account for placement related factors, such as placement instability (e.g., moving homes while in care) or placement type (e.g., foster care families, congregate care, specialized treatment care settings), which have been found in some studies to be associated with differences in PTSD, PTS symptoms, and overall mental health among youth in foster care (Gutterswijk et al., 2020; Keller et al., 2010; Okpych & Courtney, 2018; Villodas et al., 2016). Further, placement related factors have also been shown in previous literature to influence mental health service usage, such as which youth in foster care may be more likely to seek or receive services (e.g., Leslie et al., 2000). While total length of time spent in care was accounted for in the current study to provide a picture of youth who had short- or long-term stays, information was not available to determine what type of placements or how many placement changes occurred prior to receiving a PTSD diagnosis. Overall, future studies should consider examining these placement related factors and using time varying survival models to account for placement characteristics. Lastly, one should consider the robustness of the study’s findings across different populations of foster care youth as the sample in the current study was recruited from a single Midwestern county. This includes, for example, youth in foster care with known intellectual or developmental disabilities, who may be at a greater risk for maltreatment and mental health concerns (e.g., Perrigo et al., 2018). Additionally, at an administrative or systemic level, it may be the case that certain procedures of the foster care system in the county, such as access to various services or funding for the providers, could influence the rate and trajectory of PTSD diagnosis.
Conclusions
Despite these limitations, the current study provides an important step forward in understanding what specific aspects of maltreatment exposure may contribute to PTSD for youth in foster care. Findings demonstrate that when the entirety of youth’s maltreatment exposure prior to entry into foster care is examined, there does not appear to be one aspect of maltreatment exposure (i.e., type, severity, or frequency) that is most influential in determining which youth in foster care may be at most risk for receiving a PTSD diagnosis. The findings also further illustrate the need to account for the entirety of youth’s maltreatment exposure in this field of research. Moreover, in contrast to much of the previous literature, neglect and emotional abuse were more often associated with PTSD risk, as opposed to sexual or physical abuse. These findings may suggest that researchers and clinicians working with youth in foster care who experience maltreatment and trauma should not exclude these events in research questions and potentially case conceptualization, even though they may be less likely to be considered traumatic or meet “Criterion A” standards. This may be especially necessary in research given emotional abuse is not as widely studied as other types of maltreatment (e.g., Stoltenborgh, et al., 2015). Lastly, researchers studying youth in foster care should consider potential risk and protective factors associated with the foster care experience (e.g., age at entry into care) to provide a more accurate understanding of how maltreatment and risk factors more generally contribute to PTSD.
Acknowledgments
Funding: This work was supported in part by the National Institutes of Mental Health [R01 Grant MH079252-03, 2011] awarded to YJ, and the National Institutes of Mental Health [T32 Grant T32MH019927, 2019] awarded to LH.
Footnotes
Information on what event was used specifically for Criterion A to diagnosis PTSD (based on either DSM-IV or DSM-5 criteria) was not provided in the Medicaid files. Thus, maltreatment experiences in the current study were not specifically connected with a certain PTSD diagnosis. The current study is not making the claim that all forms of maltreatment or experiences of maltreatment examined in the current study (particularly forms of neglect and emotional abuse) can be classified as Criterion A events or directly used to determine a PTSD diagnosis. Rather, maltreatment histories based on frequency and severity of each type are considered as a set of risk factors for receiving a PTSD diagnosis using the current data analysis approach.
Conflict of Interest: The authors declare that they have no conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Anders SL, Shallcross SL, & Frazier PA (2012). Beyond criterion A1: The effects of relational and non-relational traumatic events. Journal of Trauma & Dissociation, 13, 134–151. [DOI] [PubMed] [Google Scholar]
- Barber JG, Delfabbro PH, & Cooper L. (2001). The predictors of unsuccessful transition to foster care. The Journal of Child Psychology and Psychiatry and Allied Disciplines, 42, 785–790. [PubMed] [Google Scholar]
- Bellis MD, Hooper SR, Spratt EG, & Woolley DP (2009). Neuropsychological findings in childhood neglect and their relationships to pediatric PTSD. Journal of the International Neuropsychological Society, 15, 868–878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cecil CA, Viding E, Fearon P, Glaser D, & McCrory EJ (2017). Disentangling the mental health impact of childhood abuse and neglect. Child Abuse & Neglect, 63, 106–119. [DOI] [PubMed] [Google Scholar]
- Cho B, & Jackson Y. (2016). Self-reported and case file maltreatment: Relations to psychosocial outcomes for youth in foster care. Children and Youth Services Review, 69, 241–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collin-Vézina D, Coleman K, Milne L, Sell J, & Daigneault I. (2011). Trauma experiences, maltreatment-related impairments, and resilience among child welfare youth in residential care. International Journal of Mental Health and Addiction, 9, 577–589. [Google Scholar]
- Contractor AA, Layne CM, Steinberg AM, Ostrowski SA, Ford JD, & Elhai JD (2013). Do gender and age moderate the symptom structure of PTSD? Findings from a national clinical sample of children and adolescents. Psychiatry Research, 210, 1056–1064. [DOI] [PubMed] [Google Scholar]
- Cummings JR, Ji X, Allen L, Lally C, & Druss BG (2017). Racial and ethnic differences in ADHD treatment quality among Medicaid-enrolled youth. Pediatrics, 139, e20162444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deutsch SA, Lynch A, Zlotnik S, Matone M, Kreider A, & Noonan K. (2015). Mental health, behavioral and developmental issues for youth in foster care. Current Problems in Pediatric and Adolescent Health Care, 45, 292–297. [DOI] [PubMed] [Google Scholar]
- Dubner AE, & Motta RW (1999). Sexually and physically abused foster care children and posttraumatic stress disorder. Journal of Consulting and Clinical Psychology, 67, 367. [DOI] [PubMed] [Google Scholar]
- English DJ, Graham JC, Litrownik AJ, Everson M, & Bangdiwala SI (2005b). Defining maltreatment chronicity: Are there differences in child outcomes?. Child Abuse & Neglect, 29, 575–595. [DOI] [PubMed] [Google Scholar]
- English D, Upadhyaya M, Litrownik A, Marshall J, Runyan D, Graham C, & Dubowitz H. (2005a). Maltreatment’s wake: The relationship of maltreatment dimensions to child outcomes. Child Abuse & Neglect, 29, 597–619. [DOI] [PubMed] [Google Scholar]
- Finkelhor D, Turner HA, Shattuck A, & Hamby SL (2013). Violence, crime, and abuse exposure in a national sample of children and youth: An update. JAMA Pediatrics, 167, 614–621. [DOI] [PubMed] [Google Scholar]
- Font SA (2015). Are children safer with kin? A comparison of maltreatment risk in out-of-home care. Children and Youth Services Review, 54, 20–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glück TM, Knefel M, & Lueger-Schuster B. (2017). A network analysis of anger, shame, proposed ICD-11 post-traumatic stress disorder, and different types of childhood trauma in foster care settings in a sample of adult survivors. European Journal of Psychotraumatology, 8, 1372543. doi: 10.1080/20008198.2017.1372543 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gutterswijk RV, Kuiper CH, Lautan N, Kunst EG, van der Horst FC, Stams GJJ, & Prinzie P. (2020). The outcome of non-residential youth care compared to residential youth care: A multilevel meta-analysis. Children and Youth Services Review, 104950. doi: 10.1016/j.childyouth.2020.104950 [DOI] [Google Scholar]
- Hildyard KL, & Wolfe DA (2002). Child neglect: Developmental issues and outcomes. Child Abuse & Neglect, 26, 679–695. [DOI] [PubMed] [Google Scholar]
- Huffhines L, & Jackson Y. (2019). Child maltreatment, chronic pain, and other chronic health conditions in youth in foster care. Journal of Child & Adolescent Trauma, 12, 437–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hulette AC, Fisher PA, Kim HK, Ganger W, & Landsverk JL (2008). Dissociation in foster preschoolers: A replication and assessment study. Journal of Trauma & Dissociation, 9, 173–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hulme PA (2004). Retrospective measurement of childhood sexual abuse: A review of instruments. Child Maltreatment, 9, 201–217. [DOI] [PubMed] [Google Scholar]
- Hussey JM, Chang JJ, & Kotch JB (2006). Child maltreatment in the United States: Prevalence, risk factors, and adolescent health consequences. Pediatrics, 118, 933–942. [DOI] [PubMed] [Google Scholar]
- Jackson LJ, O’Brien K, & Pecora PJ (2011). Posttraumatic stress disorder among foster care alumni: The role of race, gender, and foster care context. Child Welfare, 90, 71–93. [PubMed] [Google Scholar]
- Jackson Y, Gabrielli J, Fleming K, Tunno AM, & Makanui PK (2014). Untangling the relative contribution of maltreatment severity and frequency to type of behavioral outcome in foster youth. Child Abuse & Neglect, 38, 1147–1159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katz CC, Courtney ME, & Novotny E. (2017). Pre-foster care maltreatment class as a predictor of maltreatment in foster care. Child and Adolescent Social Work Journal, 34, 35–49. [Google Scholar]
- Keller TE, Salazar AM, & Courtney ME (2010). Prevalence and timing of diagnosable mental health, alcohol, and substance use problems among older adolescents in the child welfare system. Children and Youth Services Review, 32, 626–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knapp PK, Hurlburt MS, Kostello EC, Ladd H, Tang L, & Zima BT (2006). Child sociodemographic characteristics and common psychiatric diagnoses in medicaid encounter data: Are they valid? The Journal of Behavioral Health Services & Research, 33, 444–452. [DOI] [PubMed] [Google Scholar]
- Koenen KC, & Widom CS (2009). A prospective study of sex differences in the lifetime risk of posttraumatic stress disorder among abused and neglected children grown up. Journal of Traumatic Stress, 22, 566–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lansing AE, Plante WY, & Beck AN (2017). Assessing stress-related treatment needs among girls at risk for poor functional outcomes: The impact of cumulative adversity, criterion traumas, and non-criterion events. Journal of Anxiety Disorders, 48, 36–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leslie LK, Landsverk J, Ezzet-Lofstrom R, Tschann JM, Slymen DJ, & Garland AF (2000). Children in foster care: Factors influencing outpatient mental health service use. Child Abuse & Neglect, 24, 465–476. [DOI] [PubMed] [Google Scholar]
- Litrownik AJ, Lau A, English DJ, Briggs E, Newton RR, Romney S, & Dubowitz H. (2005). Measuring the severity of child maltreatment. Child Abuse & Neglect, 29, 553–573. [DOI] [PubMed] [Google Scholar]
- Lucenko BA, Sharkova IV, Huber A, Jemelka R, & Mancuso D. (2015). Childhood adversity and behavioral health outcomes for youth: An investigation using state administrative data. Child Abuse & Neglect, 47, 48–58. [DOI] [PubMed] [Google Scholar]
- Maikovich AK, Koenen KC, & Jaffee SR (2009). Posttraumatic stress symptoms and trajectories in child sexual abuse victims: An analysis of sex differences using the National Survey of Child and Adolescent Well-Being. Journal of Abnormal Child Psychology, 37, 727–737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCrae JS (2009). Emotional and behavioral problems reported in child welfare over 3 years. Journal of Emotional and Behavioral Disorders, 17, 17–28. [Google Scholar]
- McGuire A, & Jackson Y. (2018). Dimensions of maltreatment and academic outcomes for youth in foster care. Child Abuse & Neglect, 84, 82–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMillen JC, Zima BT, Scott LD Jr., Auslander WF, Munson MR, Ollie MT, & Spitznagel EL (2005). Prevalence of psychiatric disorders among older youths in the foster care system. Journal of the American Academy of Child & Adolescent Psychiatry, 44, 88–95. [DOI] [PubMed] [Google Scholar]
- Merikangas KR, He JP, Burstein M, Swanson SA, Avenevoli S, Cui L, … & Swendsen J. (2010). Lifetime prevalence of mental disorders in US adolescents: results from the National Comorbidity Survey Replication–Adolescent Supplement (NCS-A). Journal of the American Academy of Child & Adolescent Psychiatry, 49, 980–989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milot T, St-Laurent D, Ethier LS, & Provost MA (2010). Trauma-related symptoms in neglected preschoolers and affective quality of mother-child communication. Child Maltreatment, 15, 293–304. [DOI] [PubMed] [Google Scholar]
- Mitchell MB, & Kuczynski L. (2010). Does anyone know what is going on? Examining children’s lived experience of the transition into foster care. Children and Youth Services Review, 32, 437–444. [Google Scholar]
- Moore E, Gaskin C, & Indig D. (2013). Childhood maltreatment and post-traumatic stress disorder among incarcerated young offenders. Child Abuse & Neglect, 37, 861–870. [DOI] [PubMed] [Google Scholar]
- Norman RE, Byambaa M, De R, Butchart A, Scott J, & Vos T. (2012). The long-term health consequences of child physical abuse, emotional abuse, and neglect: a systematic review and meta-analysis. PLoS Med, 9(11), e1001349. doi: 10.1371/journal.pmed.1001349 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okpych NJ, & Courtney ME (2018). Characteristics of foster care history as risk factors for psychiatric disorders among youth in care. American Journal of Orthopsychiatry, 88, 269. [DOI] [PubMed] [Google Scholar]
- Oswald SH, Heil K, & Goldbeck L. (2009). History of maltreatment and mental health problems in foster children: A review of the literature. Journal of Pediatric Psychology, 35, 462–472. [DOI] [PubMed] [Google Scholar]
- Pecora PJ, White CR, Jackson LJ, & Wiggins T. (2009). Mental health of current and former recipients of foster care: A review of recent studies in the USA. Child & Family Social Work, 14, 132–146. [Google Scholar]
- Perrigo JL, Berkovits LD, Cederbaum JA, Williams ME, & Hurlburt MS (2018). Child abuse and neglect re-report rates for young children with developmental delays. Child Abuse & Neglect, 83, 1–9. [DOI] [PubMed] [Google Scholar]
- Rayburn AD, McWey LM, & Cui M. (2016). The interrelationships between trauma and internalizing symptom trajectories among adolescents in foster care. Children and Youth Services Review, 61, 332–336. [Google Scholar]
- R Core Team. (2014). R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing. [Google Scholar]
- Rock J, Geier CF, Noll JG, De Bellis MD (2018). Developmental traumatology: Brain development in maltreated children with and without PTSD. In Noll J, & Shalev I. (Eds.), The biology of early life stress (pp. 45–56). Cham, Switzerland: Springer. [Google Scholar]
- Salazar AM, Keller TE, Gowen LK, & Courtney ME (2013). Trauma exposure and PTSD among older adolescents in foster care. Social Psychiatry and Psychiatric Epidemiology, 48, 545–551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheeringa MS, Wright MJ, Hunt JP, & Zeanah CH (2006). Factors affecting the diagnosis and prediction of PTSD symptomatology in children and adolescents. American Journal of Psychiatry, 163, 644–651. [DOI] [PubMed] [Google Scholar]
- Stoltenborgh M, Bakermans- Kranenburg MJ, Alink LR, & van IJzendoorn MH (2015). The prevalence of child maltreatment across the globe: Review of a series of meta-analyses. Child Abuse Review, 24, 37–50. [Google Scholar]
- Sullivan TP, Fehon DC, Andres Hyman RC, Lipschitz DS, & Grilo CM (2006). Differential relationships of childhood abuse and neglect subtypes to PTSD symptom clusters among adolescent inpatients. Journal of Traumatic Stress, 19, 229–239. [DOI] [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS, & Ullman JB (2019). Using multivariate statistics (7th Ed.). Boston, MA: Pearson. [Google Scholar]
- Trickey D, Siddaway AP, Meiser-Stedman R, Serpell L, & Field AP (2012). A meta-analysis of risk factors for post-traumatic stress disorder in children and adolescents. Clinical Psychology Review, 32, 122–138. [DOI] [PubMed] [Google Scholar]
- Turner HA, Finkelhor D, & Ormrod R. (2010). Poly-victimization in a national sample of children and youth. American Journal of Preventive Medicine, 38, 323–330. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services, Administration on Children, Youth and Families. (2019). The AFCARS Report #26. Washington, D.C.: U.S. Government Printing Office. [Google Scholar]
- Van Vugt E, Lanctôt N, Paquette G, Collin-Vézina D, & Lemieux A. (2014). Girls in residential care: From child maltreatment to trauma-related symptoms in emerging adulthood. Child Abuse & Neglect, 38, 114–122. [DOI] [PubMed] [Google Scholar]
- Vanderminden J, Hamby S, David-Ferdon C, Kacha-Ochana A, Merrick M, Simon TR, … & Turner H. (2019). Rates of neglect in a national sample: child and family characteristics and psychological impact. Child Abuse & Neglect, 88, 256–265. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villegas S, & Pecora PJ (2012). Mental health outcomes for adults in family foster care as children: An analysis by ethnicity. Children and Youth Services Review, 34, 1448–1458. [Google Scholar]
- Villodas MT, Cromer KD, Moses JO, Litrownik AJ, Newton RR, & Davis IP (2016). Unstable child welfare permanent placements and early adolescent physical and mental health: The roles of adverse childhood experiences and post-traumatic stress. Child Abuse & Neglect, 62, 76–88. [DOI] [PubMed] [Google Scholar]
- Wechsler-Zimring A, Kearney CA, Kaur H, & Day T. (2012). Posttraumatic stress disorder and removal from home as a primary, secondary, or disclaimed trauma in maltreated adolescents. Journal of Family Violence, 27, 813–818. [Google Scholar]
- Yoon S, Cage J, Pei F, & Barnhart S. (2018). Risk and resilience factors for psychobehavioral symptom trajectories among child welfare–involved youth. Journal of Interpersonal Violence, 0886260518799485. doi: 10.1177/0886260518799485 [DOI] [PubMed] [Google Scholar]