Abstract
Introduction
Medical tourism is expanding on a global basis, with patients seeking cosmetic surgery in countries abroad. Little information is known regarding the risks and outcomes of cosmetic tourism, in particular, for aesthetic breast surgery. The majority of the literature involves retrospective case series with no defined comparator. We aimed to amalgamate the published data to date to ascertain the risks involved and the outcomes of cosmetic tourism for aesthetic breast surgery on a global basis.
Methods
A systematic review of PubMed, Google Scholar, EMBASE, the Cochrane library and OVID Medline was conducted using the PRISMA (Preferred Reporting Items for Systematic reviews and Meta-analyses) guidelines. Keywords such as “medical tourism”, “cosmetic tourism”, “tourism”, “tourist”, “surgery”, “breast” and “outcomes” were used. Seven hundred and seventy-one titles were screened, and 86 abstracts were reviewed leaving 35 full texts. Twenty-four of these met the inclusion criteria and were used to extract data for this systematic review.
Results
One hundred and seventy-one patients partook in cosmetic tourism for aesthetic breast surgery. Forty-nine percent of patients had an implant-based procedure. Other procedures included: mastopexy (n=4), bilateral breast reduction (n=11) and silicone injections (n=2). Two-hundred and twenty-two complications were recorded, common complications included: wound infection in 39% (n=67), breast abscess/ collection in 12% (n=21), wound dehiscence in 12% (n= 20) and ruptured implant in 8% (n=13). Clavien–Dindo classification of the complications includes 88 (51%) IIIb complications with 103 returns to theatre, 2 class IV complications (ICU stay) and one class V death of a patient. Explantation occurred in 39% (n=32) of implant-based augmentation patients.
Conclusions
Aesthetic breast surgery tourism is popular within the cosmetic tourism industry. However, with infective complications (39%) and return to theatre rates (51%) significantly higher than expected, it is clear that having these procedures abroad significantly increases the risks involved. The high complication rate not only impacts individual patients, but also the home country healthcare systems. Professional bodies for cosmetic surgery in each country must highlight and educate patients how to lower this risk if they do choose to have cosmetic surgery abroad. In this current era of an intra-pandemic world where health care is already stretched, the burden from cosmetic tourism complications must be minimised.
Level of Evidence III
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.
Keywords: Medical tourism, Breast surgery, Aesthetic surgery
Introduction
Medical tourism is defined as a patient seeking medical treatment out with their local practitioner. Medical tourism can be classified within the plastic surgery field as “macrotourism”, where patients go abroad for plastic surgery, “microtourism”, which involves going to a distant surgeon for plastic surgery or “speciality tourism”, which involves going to a surgeon from a different specialty for a cosmetic surgery procedure. All of these definitions include the need for follow-up or fixation of complications by the local plastic surgery team. Although some patients may seek surgery elsewhere by a surgeon with a particular area of expertise, more commonly, patients travel for cosmetic procedures to seek out lower cost surgery [1, 3].
Cosmetic tourism is increasing in popularity for numerous reasons including: lower perceived cost, confidentiality, availability of procedures in a timely fashion, including multiple procedures for a lower price, personal recommendations and social media influencers and advertisements [2, 3]. Within the UK, there are strict guidelines for access to breast surgery within the National Health Service, with funding decisions made by local clinical commissioning groups [4]. Aesthetic breast procedures are not funded on the NHS.
To date, the literature has indicated higher complication rates amongst patients undergoing cosmetic procedures abroad. The majority of publications are retrospective in nature with low numbers of patients. Due to the nature of these reports, there is no comparison group to determine the equivalent surgical outcomes and complications in the native country for the same procedures. The home healthcare systems are left to deal with the resultant complications, which are usually costly. Thacoor et al have reported an average treatment cost of over $16,000 per patient following cosmetic tourism complications. They also conclude this is likely an underestimate as cosmetic tourists’ complications are under reported [5].
We have performed a systematic review to amalgamate the published data on cosmetic tourism, particularly, aesthetic breast surgery, to ascertain the specific risks involved and the outcomes on a global basis. Complications are graded I–V according to the Clavien–Dindo classification of surgical complications.
Methods
A systematic review of PubMed, Google Scholar, EMBASE, the Cochrane library and OVID Medline was conducted, using PRISMA (Preferred Reporting Items for Systematic reviews and Meta-analyses) guidelines, in November 2020. The question we aimed to answer was “What are the outcomes for patients who seek aesthetic breast surgery abroad?”. Keywords used for the search included “ medical tourism”, “cosmetic tourism”, “surgery”, “surgical”, “tourism”, “tourist”, “travel”, “abroad”, “global”, “breast”, “outcomes”, “complications”, “postoperative” and “postsurgical”.
Two separate authors (SMc and SM) screened titles and abstracts independently using the “Covidence” application for systematic reviews. Duplicates were removed from the search process.
Inclusion criteria included: those studies relating to aesthetic breast surgery performed abroad. All study types encompassing case reports, case series, retrospective and prospective studies were included. Studies reporting on aesthetic breast surgery involving any type of breast implant, silicone injections, fat grafting, reduction, augmentation, mastopexy to either unilateral or bilateral breasts with or without any additional procedures, performed abroad were included.
Data extracted included home country, country where surgery was undertaken, demographics of patient, type of surgery undertaken, post-operative outcome, return trips to theatre, complications, and management plan in local institution.
Exclusion criteria included: conference abstracts, patients <18 years of age, cosmetic surgery other than aesthetic breast surgery. Papers were also excluded if there was insufficient information provided to give adequate outcomes specifically related to aesthetic breast surgery.
Once independently selected, the corresponding full texts were reviewed and those papers which contained salient information relating to risk factors and outcomes in aesthetic breast surgery performed abroad were analysed. Using the ‘COVIDENCE’ application for systematic reviews allowed for any disagreements to be resolved between the two authors with senior author making the final decision (see Fig. 1).
Fig. 1 .
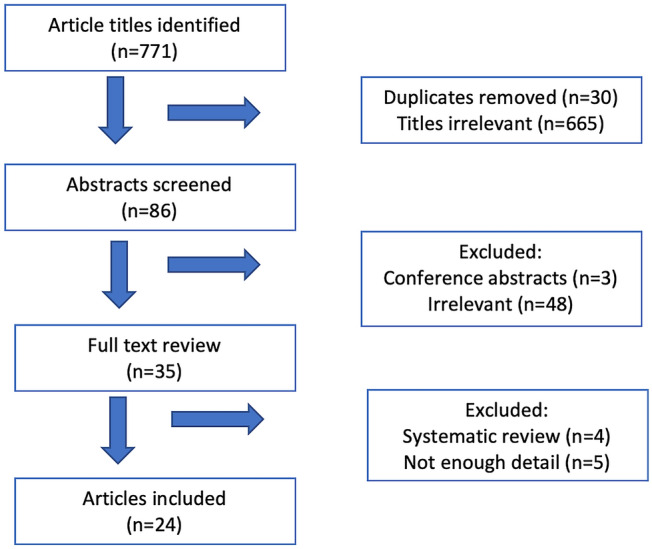
Flowchart showing methodology as per PRISMA guidelines
Results
Seven hundred and seventy-one article titles were identified, 30 duplicates were removed, 86 titles were included, and their abstracts were screened. Thirty-five full texts met criteria and were reviewed by two authors. Nine full texts were subsequently excluded (see above flow chart for reasons), and 24 papers were deemed appropriate for inclusion and data extraction.
One hundred and seventy-one patients underwent aesthetic breast surgery abroad which included 167 females, 1 male and 3 male-to-female transgender patients. The average age (those whose age was recorded explicitly) was 38.7 years old (range 24–66 years).
The most common countries where aesthetic breast complications were specifically recorded following the primary procedures included: the Dominican Republic (n=14), Thailand (n=10) and Mexico (n=6). However, Eastern Europe, India, other South American and Middle Eastern countries also had documented cases of aesthetic breast surgery tourism with complications within the texts.
The most frequent aesthetic breast procedure performed was breast augmentation in 83 patients (49%). There were 61 cases of bilateral breast augmentation alone, 7 cases of bilateral breast augmentation in conjunction with other multiple procedures (including abdominoplasty, liposuction, labiaplasty, etc.), 8 cases of augmentation mastopexy, 5 cases of augmentation mastopexy in conjunction with multiple other body site cosmetic procedures, one case of implant exchange and one case of bilateral breast augmentation utilising both implants and silicone injections. Out of the 103 patients that had specific procedures documented, 18 patients (17%) had multiple procedures, with at least one other cosmetic procedure being performed at the same time as their breast procedure (see Table 1).
Table 1.
Number of patients per procedure described
| Procedures | Patients |
|---|---|
| BBA | 61 |
| BBA + Mastopexy | 8 |
| BBA + Mastopexy + Multiple | 5 |
| BBA + Multiple | 7 |
| BBA + Silicone Injections | 1 |
| BBR | 9 |
| BBR + Multiple | 2 |
| Mastopexy + Multiple | 4 |
| Implant exchange | 1 |
| Fat grafting | 1 |
| Scar revision + fat grafting | 1 |
| Gynaecomastia excision | 1 |
| Silicone breast injections | 2 |
| "Breast Surgery" | 68 |
BBA bilateral breast augmentation, BBR bilateral breast reduction, “Breast surgery”—paper did not describe specifically what initial aesthetic breast procedure was performed
Bilateral breast reduction was performed in 11 cases, two of which had other body site cosmetic procedures at the same time. Four mastopexies in conjunction with other body site procedures were performed; there were no cases of mastopexy as a single procedure. Other procedures recorded included: one oncoplastic scar contracture revision and fat grafting, one case of fat grafting as a single procedure, one case of gynaecomastia excision, two cases of silicone breast injections.
Sixty-eight cases were documented only as aesthetic “breast surgery” without specific procedures being listed; however, the authors felt sufficient information was available in these articles to include their complications and information in the analysis.
Overall, there were 222 complications recorded in relation to aesthetic breast surgery. The most common complications included: wound infection in 39% (n=67), breast abscess/collection in 12% (n=21), wound dehiscence in 12% (n= 20) and implant rupture in 8% (n=13) of patients (see Table 2).
Infection was the commonest occurring complication, unusual but serious bacterial and fungal species were also recorded. There were 23 cases of Mycobacterium abscesses recorded (13%), including: one case each of Mycobacterium chelonae, Mycobacterium fortuitum and Saksenaea erythrospora infections.
Complications were classified using the Clavien–Dindo classification of surgical complications. This was chosen as a method of standardising complications across the included studies for more accurate comparison. (Table 3)
Table 2.
Types of complications found in aesthetic breast surgery tourism patients
| Complications | Cases |
|---|---|
| Wound infection (11 due to mycobacterium abscessus) | 67 |
| Abscess/ Collection (12 due to mycobacterium abscessus) | 21 |
| Wound dehiscence | 20 |
| Mycobacterium Abscessus bacterium isolated- total | 23 |
| Implant rupture | 13 |
| Capsular contracture | 10 |
| Seroma | 8 |
| Chronic infection | 5 |
| Implant exposure | 5 |
| Fat necrosis | 5 |
| Breast asymmetry | 4 |
| NAC necrosis | 3 |
| Sinus/fistula | 3 |
| Silicone granuloma | 3 |
| Ulcerative lesions | 3 |
| Sepsis | 2 |
| Skin necrosis | 2 |
| Haematoma | 2 |
| Giant cell reaction + fibrosis | 2 |
| DVT | 2 |
| PE | 1 |
| Cardiac arrest | 1 |
| Pyelonephritis | 1 |
| Gossypiboma | 1 |
| PIP implant | 1 |
| Keloid | 1 |
| Lung granuloma | 1 |
| Hypercalcaemia + nephrolithiasis | 1 |
| Persistent ptosis | 1 |
| Total | 222 |
NAC nipple–areolar complex
Grade V: one patient died due to hypoxic brain injury immediately post-operatively, grade IVa and IVb; two patients required ICU admission with either single or multiple organ failure secondary to sepsis from wound infections.
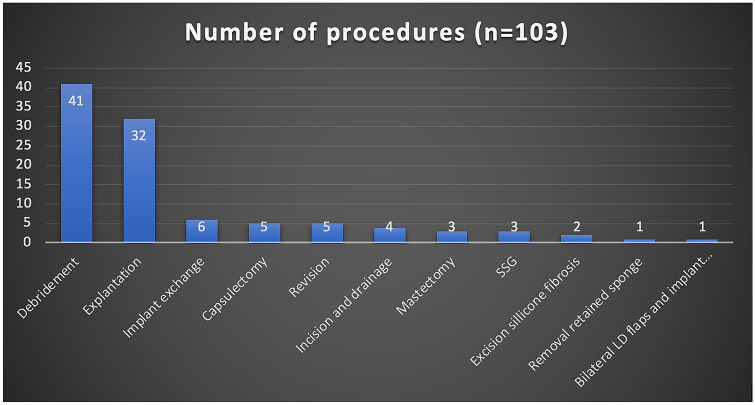
Grade IIIb: complications that required a return to theatre under general anaesthetic occurred 106 times in 88 patients (51%), with 15 patients requiring multiple general anaesthetics amongst that group (9% of overall patients, 17% of return to theatre group) [6], (see Table 3 and Graph 1).
Three patients required emergency mastectomies, three patients had split-thickness skin graft reconstruction, and one patient needed bilateral latissimus dorsi and implant-based delayed reconstruction post-débridement. In total, 39% (n=32) of implant-based augmentation procedures (n=83) required either a unilateral or bilateral explantation procedure on return to their local provider (Table 4).
Table 4.
Results table of all papers reviewed
| Paper | Paper type | Year | Author country | Tourism country | Number of patients | Patient age and sex | Procedure | Outcome | Post-operative procedures | Bed days | M&M |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Birch et al [2] | Case series | 2007 | England |
Brazil Brussels |
2 | 30 female | BBA |
1.Skin dehiscence 2.Skin necrosis 3.Wound infection |
1. Wound debridement and bilateral explantation | 10 days | |
| 25 female | BBA | 1.Wound infection | 1. Wound debridement and implant replacement | 2 days | |||||||
| Handschin et al [7] | Case report | 2007 | Switzerland | Dominican Republic | 1 | 31 female | BBA |
1. Wound infection 2. Chest pain and SOB 3. PE 4. Wound dehiscence 5. Infected seroma |
1. Wound debridement and Unilateral explantation | 4 days | PE- on warfarin |
| Niechajey et al [8] | Case report | 2011 | Sweden | Poland | 1 | 31 female | BBA | 1. Post-operative cardiac arrest secondary to hypoxia caused by anaesthetic drugs | Vegetative state, ICU | ||
| Miyagi et al [9] | Retrospective review | 2012 | England | Europe, India, southeast Asia, middle east | 14 | All female | x11 BBA |
1. x2 ruptured implants 2. x5 wound infection 3. x4 asymmetry 4. x2 capsular contracture 5. persistent ptosis |
1. x2 explantantions 2. x4 implant exchanges 3. x1 capsule biopsy 4. x1 salvage operation |
||
| BBR |
1. Wound infection 2. Wound dehiscence |
1. Debridement and SSG 2. Revision BBR |
|||||||||
| BBA and mastopexy, abdominoplasty. |
1. Wound infection 2. Wound dehiscence |
1. x3 trips to theatre for multiple revision mastopexies | |||||||||
| BBA and mastopexy, abdominoplasty, liposuction, vaginal tightening, axillary sympathectomy |
1. Wound infection 2. Wound dehiscence 3. Fat necrosis |
||||||||||
| Maurer et al [10] | Case Series | 2014 | Switzerland | Dominican Republic, Mexico, Ecuador | 5 | Female | BBA x 2 |
1. Wound infection 2. Breast abscess (mycobacterium abscessus) |
1. Bilateral explantation and washout of pus x2 | ||
| BBR x 3 +− abdominoplasty |
1. Wound infection 2. Breast abscess (mycobacterium abscessus) |
1. Wound debridement x3 operations | |||||||||
| Kantak et al [11] | Case report | 2014 | USA | 1 | 64 female | BBA |
1. Firm swelling 2. Gossypiboma |
1. Removal of retained sponge | |||
| Rüegg et al [12] | Case report | 2015 | Switzerland | Mexico | 1 | 39 female | BBA and mastopexy, BBL |
1. Swollen breast 2. Wound dehiscence 3. Peri-prosthetic fluid (mycobacterium abscessus) |
1. Bilateral implant explantation and capsulectomy | ||
| Livingston et al [13] | Retrospective review | 2015 | Australia | Thailand | 10 |
BBA x 7, BBA and mastopexy x3 |
1. Wound infection x4. 2. NAC necrosis x1 3. Ruptured implant x1 4. Implant extrusion x1. 5. Seroma 6. Wound dehiscence |
||||
| Cai et al [14] | Case report | 2015 | USA | Dominican Republic | 1 | 43 female | BBR, abdominoplasty and liposuction |
1. Wound infection by mycobacterium abscessus 2. Wound dehiscence 3. Fluid collection |
1. Wound debridement x3 operations and NPWT | Poor aesthetic outcome | |
| Green et al [15] | Case report | 2015 | USA | Dominican Republic | 1 | 55 female | BBR |
1. Palpable breast collection 2. Draining sinus 3. Ultrasound guided FNA 4. Fat necrosis 5. Chronic infection and induration |
1. Excision of abscess cavity and biopsy 2. Second biopsy |
Poor aesthetic outcome | |
| Rodríguez et al [16] | Case report | 2016 | Columbia | Venezuela | 1 | 29 female | Dermolipectomy and BBA |
1. Sepsis 2. Skin necrosis secondary to saksenaea erythrospora infection 3. ICU stay 4. Hyperbaric oxygen |
1. Removal of implants 2. Unilateral radical mastectomy 3. Unilateral radical mastectomy |
2 months | ICU, major reconstruction of entire chest wall awaited |
| Singh et al [17] | Case series | 2016 | USA | Dominican Republic | 3 | 36 female | BBA + BBL | 1. Bilateral breast abscess (mycobacterium abscessus) | 1. Bilateral explantation and washout of pus | ||
| Mexico | 29 female | BBA | 1. Unilateral breast abscess (mycobacterium abscessus) | 1. Bilateral explantation and washout of pus | |||||||
| Dominican Republic | 44 female | Bilateral mastopexy and abdominoplasty | 1. Bilateral breast abscess (mycobacterium abscessus) | 1. Incision and drainage of abscess | |||||||
| Klein et al [18] | Retrospective review | 2016 | Switzerland | Global | 68 | Female | "Breast surgery" |
1. x7 capsular contractures 2. x8 implant rupture 3. Wound infection 4. Wound dehiscence 5.Haematoma/seroma |
24 re-operations | ||
| Adabi et al [19] | Retrospective review | 2017 | USA | 8 | BBA x3 |
1. Pyelonephritis 2. Wound infection |
|||||
| BBA and abdominoplasty x2 | 1. Wound dehiscence | ||||||||||
| BBA and lipo-abdominoplasty x2 | 1. DVT x1 | DVT- anticoagulation | |||||||||
| Mastopexy and abdominoplasty | 1. DVT x1 | DVT- anticoagulation | |||||||||
| Farid et al [20] | Retrospective review | 2018 | England | Global | 7 | Female | Implant exchange | 1. PIP implant | 1. Bilateral implant explantation | 4 days | |
| Female | BBA | 1. Wound dehiscence | |||||||||
| Female | Mastopexy and brachioplasty | 1. Wound dehiscence | |||||||||
| Female | Mastopexy and abdominoplasty | 1. Keloid scar | |||||||||
| Male | Gynaecomastia and abdominoplasty | 1. Wound infection | |||||||||
| Female | BBA, thigh lifts and liposuction | 1. Wound infection | 12 days | ||||||||
| Female | Mastopexy and abdominoplasty |
1. Wound infection 2. Infected Seroma |
1 day | ||||||||
| Thacoor et al [5] | Retrospective review | 2018 | England | 8 | BBA x5 |
1. Wound infection 2. Wound dehiscence |
|||||
| 31 female | BBA and Mastopexy | 1. NAC necrosis |
1. Wound debridement x 2. 2. Wound debridement and skin graft 3.Bilateral implant explantation |
||||||||
| BBR x2 |
1. Wound infection 2. Wound dehiscence |
||||||||||
| Ovadja et al [21] | Case series | 2018 | Netherlands | Dominican Republic | 2 | 34 female | BBA and abdominoplasty |
1. Breast abscess (mycobacterium abscessus) 2. Wound dehiscence 3. Sinus formation 4. Long term antibiotics |
1. Bilateral implant explantation | 2 months | Ongoing sinuses, refusing treatment |
| Brazil | 24 female | Revision BBA and mastopexy |
1. Unilateral breast abscess (mycobacterium fortuitum) 2. 4months antibiotics |
1. Unilateral implant explantation 2. Unilateral explantation |
|||||||
| Lee et al [22] | Case series | 2018 | USA | Dominican Republic | 4 | Female | BBA and abdominoplasty |
1. Wound infection by mycobacterium abscessus 2.Wound dehiscence 3. Fluid collection in breast |
1. Bilateral explantation and washout of pus | ||
| Dominican Republic | BBA and mastopexy |
1. Wound infection by mycobacterium abscessus 2. Wound dehiscence 3. Fluid collection in breast |
1. Bilateral explantation and washout of pus | ||||||||
| Dominican Republic | BBA |
1. Wound infection by mycobacterium abscessus 2. Wound dehiscence 3. Fluid collection in breast 4. x2 admissions |
1. Bilateral explantation and washout of pus | ||||||||
| Dominican Republic | BBA and lipo-abdominoplasty |
1. Wound infection by mycobacterium abscessus 2. Wound dehiscence 3. Fluid collection in breast 4. x2 admissions |
1.Bilateral explantation and washout of pus 2. Second procedure- not documented what occurred |
||||||||
| Jensen et al [23] | Case report | 2018 | Denmark | India | 1 | 36 female | BBR |
1.Mycobacterium abscessus 2. Ulcers 3. Wound infection |
1. Washout and débridement 2. Long term antibiotics |
||
| Parel-Amini et al [24] | Retrospective review | 2019 | France |
North Africa (Tunisia) Latin America Europe USA |
18 | X18 BBA |
1.Wound infection x18 2.Mycobacterium abscessusx4 3. Seroma x4 |
1.Washout and débridement (n=26) 2.Multiple washouts n=5 3.Explantation n=7 4. Long term antibiotics |
|||
| Zheng et al [25] | Retrospective review | 2019 | USA | Guatemala | 7 | 55 female | BBA |
1. Implant rupture 2. Lung granuloma and silicone embolisation 3. Breast abscess |
1. Unilateral implant explanation and washout abscess | ||
| Puerto Rico | 47 female | Silicon breast injections |
1. Fat necrosis 2. Giant cell reaction and fibrosis |
1. Excision of silicone fibrosis and fat grafting 2. Breast revision |
|||||||
| Venezuela | 44 female | BBA |
1. Fat necrosis 2. Giant cell reaction and fibrosis |
||||||||
| Dominican Republic | 28 female | BBA |
1. Ruptured implant 2. Seroma 3. Chronic inflammation |
1. Incision and drainage of seroma 2. Bilateral implant explantation |
|||||||
| Mexico | 36 male to female | Silicone injections to breast, buttocks, thigh, hips |
1. ulceration 2. wound infection 3. granulomas 4. hypercalcaemia and obstructive nephrolithiasis |
1. Incision and removal of silicone - every two weeks | |||||||
| Mexico | 46 male to female | BBA | 1. Capsular contracture | 1. Bilateral capsulectomy and exchange of implants | |||||||
| Mexico | 40 male to female | BBA and silicone breast injections |
1. wound infection 2. extrusion 3. migration 4. scarring 5. fat necrosis 6. granuloma 7. loss of nipple |
1. Bilateral implant explantation 2. Debridement of silicone and subcutaneous nodules 3. Bilateral LD flaps with implant reconstruction and NAC reconstruction |
|||||||
| Martin et al [26] | Case Series | 2019 | Northern Ireland | Belgium | 4 | 24 y female | Left breast reduction, right mastopexy |
1. Breast reduction wound infection and necrosis. 2. NPWT 3. x2 admissions |
1. Debridement and skin grafting | 5 days | Poor aesthetic outcome |
| Poland | 25 female | BBA and labiaplasty |
1. Chest pain and SOB 2. Pus around implant |
1. Bilateral explantation and washout of pus | 3 days | ||||||
| Turkey | 30 female | BBA |
1. Wound dehiscence and infection 2. Implant exposure |
1. Removal of unilateral implant | 5 days | Asymmetrical breast- one implant in situ | |||||
| Estonia | 46 female | BBA and mastopexy | 1. Wound infection | nil | 2 days | ||||||
| Miguel et al [27] | Case series | 2020 | Spain | Peru | 2 | 66 female | Oncoplastic scar contracture revision with fat grafting |
1. Breast ulcerative lesions (mycobacterium abscessus) 2. long term IV antibiotics |
1. Simple mastectomy | 2 months | Mastectomy |
| Peru | 29 female | Breast augmentation with fat grafting |
1. Multiple subacute breast abscesses (Mycobacterium abscessus) 2. Fistulas 3. Long term antibiotics 4. Recurrent aspirations |
||||||||
| Jhaveri et al [28] | Case report | 2020 | Israel | Dominican Republic | 1 | 36 female | BBA |
1. Breast haematoma 2. Aspiration 3. Erythema and pain 4. Bilateral abscess- mycobacterium chelonae 5. Sepsis |
1. Bilateral implant explantation |
Table 3.
Clavien–Dindo classification of aesthetic breast surgery tourist complications
| Grade | Description | Complications in patient cohort |
|---|---|---|
| I | Deviation from normal, i.e. minor wound infection or collection. | |
| II | Normal course altered. Pharmacological, radiological or endoscopic intervention required. |
3-Anticoagulation (2 DVT, 1 PE) 67-Wound infection requiring antibiotics 2-Negative pressure wound therapy 4-Long term antibiotic for chronic infection 3-Haematoma/seroma needing U/S drainage 1-pyelonephritis needing IV antibiotics 1-Hyperbaric oxygen |
| III |
Intervention required 3a. Local anaesthetic 3b. General anaesthetic |
88 patients returned to theatre under general anaesthetic a total of 103 times |
| IV |
Life-threatening complication, requiring ICU. 4a. single organ failure 4b. multiorgan failure |
2-ICU admissions |
| V | Death of a patient | 1-Hypoxic brain injury and cardiac arrest immediately post-operative |
Two patients suffered from a deep vein thrombosis (DVT) and one from a pulmonary embolism (PE) requiring anticoagulation (see Fig. 2).
Fig.2 .
Operative procedures recorded by local surgeons to treat aesthetic breast surgery tourist complications (not including 24 “re-operations” that did not specifically explain the operative procedure) (SSG=split-thickness skin graft)
Discussion
With the increasing popularity of cosmetic tourism for aesthetic breast surgery, it is surprising that governments that fund healthcare systems within their country have not developed a database to record all cosmetic tourism complications given the significant financial cost it incurs. Our systematic review amalgamates the published evidence to date, describing the risks and outcomes of aesthetic breast surgery abroad in 171 patients. The majority of these patients suffered life altering consequences, and in some cases, unfortunately, patients required lifesaving treatment for these complications, with one death reported.
The difficulty with interpreting outcome data for cosmetic tourism involves the lack of a comparison cohort of patients undergoing surgery at home. All papers published to date are retrospective case series. In addition, it is impossible to determine the “denominator”, i.e. the true number of patients that travel abroad for cosmetic surgery. The patients that come to the attention of clinicians are unfortunately only those that suffer complications necessitating treatment at home; therefore, the true complication rate is difficult to determine. Despite this, complication rates for aesthetic breast surgery are well published in the literature and despite minor inter-surgeon differences, the overall complication rates of aesthetic surgery remain low.
Despite the limitations discussed, this systematic review has found that patients suffer from higher rates of infective complications and wound dehiscence, as well as skin, nipple and/or fat necrosis, when undergoing aesthetic breast surgery abroad.
These procedures are commonly undertaken in countries with less regulated healthcare systems, which lure patients with the promise of lower costs and special rates for multiple procedures, further increasing the associated risks. Complications were reported from several countries across the globe within this systematic review, including: the Dominican Republic, Thailand and Mexico. Additionally, India and countries in the Middle East, South America and Eastern Europe were also included.
These countries are less likely to have a rigorously regulated healthcare systems. Indeed, some of these nations will not have any regulatory body, with some surgeons performing aesthetic breast procedures without any training in plastic surgery. Kantak describes the case of a retained sponge found in a patient who presented with a firm swelling months after a bilateral breast augmentation abroad. This demonstrates the consequences of a lack of standard operating procedures and safety regulations, such as the WHO checklist [11].
In the UK, patients undergoing breast surgery for a breast malignancy receive prophylactic antibiotics at induction due to higher rates of surgical site infection [29, 30]. Aesthetic breast surgery is classified as a clean procedure with wound infection rates expected to be less than <5%. A systematic review by Harwicke et al concluded that aesthetic breast surgery should be classed as “clean–contaminated” due to bacteria harboured in the lactiferous ducts. All patients should be given prophylactic antibiotics at induction to lower the risk of surgical site infection [30, 31].
The high rate of infective complications across all types of aesthetic breast surgery performed abroad (39%) in this systematic review suggests a lack of antibiotic prophylaxis or a lack of sterile aseptic surgical techniques, further supported by the high explantation rate (39%) in patients undergoing augmentation procedures due to purulent peri-prosthetic infections.
In addition, travelling to foreign countries exposes patients to a wider variety of pathogenic microorganisms, particularly rarer pathogens which are harder to culture, diagnose and treat. An important example of this was the identification of various Mycobacterium species following aesthetic surgery in the Dominican Republic [10, 12, 14, 17, 21, 22, 27]. Mycobacterium infection led to abscess formation, skin necrosis and the need for complex debridement and reconstruction in these patients after difficulty with diagnosis. These rarer pathogens are not commonly seen, and delayed culture techniques required for diagnosis are not performed routinely. An awareness of such infections is needed to ensure appropriate cultures are performed to enable targeted treatment of the offending organism [32].
Wound infection rates reported across the studies in this systematic review were significantly higher than the expected rate of less than 5%, with 39% of patients requiring treatment with antibiotics, 12% developing a breast abscess and at least 13% of the total group of patients culturing rare Mycobacterium infections (26% of all infections) [29, 31] It is important to note that infective complications included in this review are only patients that required admission to hospital for intravenous antibiotics. The true wound infection rate is likely to be significantly higher, with patients requiring oral antibiotics for minor wound infections not included in these studies.
Class II complications that required treatment with simple measures such as pharmacological intervention, radiological aspiration or prolonged dressings were found in in over half the patients (n=87, 51%). More serious complications, as per Clavien-Dindo classification, led to a return to theatre in 88 patients (51%) and multiple returns to theatre in 15 patients (9%), with two patients requiring ICU and one death following a cardiac arrest in the post-operative period.
Thrombotic complications, both DVT and PE, were reported in this review (n=2 and n=1, respectively) [7, 19]. VTE is a well-known complication associated with surgery and in particular, prolonged procedures under general anaesthesia. Prophylaxis in the form of subcutaneous heparin and thromboembolic deterrent stockings (TEDs) are routine practice in many countries for all patients undergoing surgery, and these are also included on the WHO checklist in many operating departments. VTE risk is increased further for patients undergoing multiple procedures which is common amongst cosmetic tourists, availing of package deals with extra savings. Across this systematic review, one-fifth of patients (20%) had multiple procedures documented, with at least one other cosmetic procedure performed at the same time as their breast procedure. In addition, travelling and long-haul flights are an independent risk factor for VTE; thus, these risk factors become cumulative in patients travelling abroad for aesthetic procedures. This complication is potentially life-threatening but also preventable in patients undergoing surgery in a regulated practice with appropriate prophylaxis [33].
The peri-operative care received by patients travelling abroad is commonly sub-optimal and likely to factor in the high rate of post-operative complications. A range of reasons for this have been reported. Patients commonly pay for procedures in advance before travelling, and in many cases before they have a consultation with the operating surgeon. A language barrier may further compromise the patients care, with patients felling obligated to proceed with surgery on arrival, without valid informed consent. Standard practice in the UK involves a minimum two-week “cooling off” period following the initial consultation and discussion of the potential risks before proceeding with surgery [1, 34–36].
The follow-up included with these package deals tends to be minimal and when the patient travels home, any complications that develop become a problem for the home healthcare system. The cost of managing these complications ranges from £4000 per patient to $250,000 in one American paper [22, 26]. The high price is due to emergency theatre, multiple outpatient visits, dressings, unexpected hospital admissions, long-term antibiotics and for a few patients, the prolonged inpatient treatment or ICU admission [20, 22, 26, 37].
Within the UK, there is an obligation to treat patients presenting to an NHS hospital with acute complications. The need for revision procedures for cosmetic reasons, however, is not routinely covered, and patients should be directed to either their operating surgeon or a private cosmetic provider. It is important to note that the majority of patients requiring surgery for complications will be left with a sub-optimal cosmetic outcome, and in some patients, significant disfigurement. There are only scant reports in the literature reporting good outcomes following cosmetic tourism. Campbell et al. report a survey-based study of 460 cosmetic tourists who attended their Colombian clinic for a range of cosmetic procedures. They state 98% of patients said they passed the “friends and family test” and had an overall high rate of satisfaction with their surgical outcome [38].
The longer-term outcomes have not been discussed individually, but implant rupture, capsular contracture, recurrent ptosis, asymmetry and poor cosmesis were all documented within this systematic review. Further costs will be incurred by patients in a quest to correct both these short- and long-term complications which will negate the cost benefit of travelling abroad for the initial surgery.
The management of complications varies between countries, which is evident from this systematic review. Some of the papers included document reconstructive procedures including chest wall reconstruction with bilateral latissimus dorsi flaps and implants to treat the complications of silicone breast injections and implants carried out abroad. These were performed in the USA, where the healthcare system is significantly different to the UK. Trying to reconstruct or revise these cases is further complicated by the lack of access to operative notes. This is particularly relevant for BBR, with no documentation of the vascular pedicle used to preserve the NAC, further exacerbating the risks involved with any revision procedure. The need for explantation in 39% of implant cases as well as the need for emergency mastectomies in 3 patients is concerning. This is compounded with the aforementioned risk to life due to anaesthetic and thrombotic complications.
Aesthetic associations across the world, including the International Society of Aesthetic Plastic Surgery (ISAPS), the British Association of Plastic and Reconstructive Aesthetic Surgery (BAPRAS) and the American Society of Plastic Surgeons (ASPS), have produced information on their websites for people considering travelling abroad for cosmetic surgery. This includes questions to ask providers to ensure they choose a qualified plastic surgeon in a regulated hospital, educating and empowering the public to make informed choices and hopefully reduce the risks of complications and the burden on home healthcare systems. This is currently of particular importance within the constraints of a global pandemic that is pushing the health care we can offer to the limit, and we must therefore lower any potential chance of risk as a matter of necessity [39].
We highlight the COVID-19 pandemic as a final point as to why the cosmetic tourism industry should be an increasing concern. International travel increases the risk of transmission, and the resultant global travel restrictions in place will make it increasingly difficult for patients to return to the operating surgeon if required. In addition, healthcare systems are under extreme pressure and cosmetic tourists seeking treatment for complications from abroad adds increased pressure to an already stretched system. The knock-on effects of Covid-19, including the increased waiting list times, will potentially increase the demand for cosmetic tourism further in the future.
Conclusion
This systematic review highlights the high complication rates associated with travelling abroad for aesthetic breast surgery, including life-threatening complications. We describe the commonest complications encountered, including wound infection and peri-prosthetic infection requiring explantation in 38% of patients undergoing augmentation procedures. Poor long-term outcomes including implant rupture, capsular contracture, recurrent ptosis, asymmetry and poor cosmesis have been described. All of these will have a negative psychological impact and financial burden for the patients involved.
It is evident from this review that cosmetic tourism is a global phenomenon, with patients continuing to travel for these purposes even amidst a global pandemic. The regulatory bodies must highlight these risks, educate and empower the public to seek out regulated healthcare providers to reduce the associated morbidity and mortality and to reduce the burden on global healthcare systems already stretched beyond capacity.
Declaration
Conflict of interest
The authors declare that they have no conflicts of interest to disclose
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors
Informed Consent
For this type of study informed consent is not required
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Iorio ML, Verma K, Ashktorab S, Davison SP. Medical tourism in plastic surgery: ethical guidelines and practice standards for perioperative care. Aesthetic Plast Surg. 2014;38(3):602–607. doi: 10.1007/s00266-014-0322-6. [DOI] [PubMed] [Google Scholar]
- 2.Birch J, Caulfield R, Ramakrishnan V. The complications of 'cosmetic tourism' - an avoidable burden on the NHS. J Plast Reconstr Aesthet Surg. 2007;60(9):1075–1077. doi: 10.1016/j.bjps.2007.03.030. [DOI] [PubMed] [Google Scholar]
- 3.Connell J. Medical tourism: sea, sun, sand and surgery. Tour Manag. 2006;27(6):1093–1100. doi: 10.1016/j.tourman.2005.11.005. [DOI] [Google Scholar]
- 4.NHS, Breast Reduction. (2020) Available at: https://www.nhs.uk/conditions/breast-reduction-on-the-nhs/. Accessed November 9th
- 5.Thacoor A, van den Bosch P, Akhvani MA. Surgical management of cosmetic surgery tourism-related complications: current trends and cost analysis study of the financial impact on the UK national health service (NHS) Aesthet Surg J. 2019;39(7):786–791. doi: 10.1093/asj/sjy338. [DOI] [PubMed] [Google Scholar]
- 6.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240(2):205–213. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Handschin AE, Banic A, Constantinescu MA. Pulmonary embolism after plastic surgery tourism. Clin Appl Thromb Hemost. 2007;13(3):340. doi: 10.1177/1076029607302580. [DOI] [PubMed] [Google Scholar]
- 8.Niechajev I, Frame J. A plea to control medical tourism. Aesthetic Plast Surg. 2012;36(1):202–206. doi: 10.1007/s00266-011-9766-0. [DOI] [PubMed] [Google Scholar]
- 9.Miyagi K, Auberson D, Patel AJ, Malata CM. The unwritten price of cosmetic tourism: an observational study and cost analysis. J Plast Reconstr Aesthet Surg. 2012;65(1):22–28. doi: 10.1016/j.bjps.2011.07.027. [DOI] [PubMed] [Google Scholar]
- 10.Maurer Fp, Castelberg C, von Braun A, Wolfensberger A, Bloemberg Gv, Bottger Ec, Somoskovi A. Postsurgical wound infections due to rapidly growing mycobacteria in Swiss medical tourists following cosmetic surgery in Latin America between 2012 and 2014. Euro Surveill. 2014 doi: 10.2807/1560-7917.ES2014.19.37.20905. [DOI] [PubMed] [Google Scholar]
- 11.Kantak NA, Reish RG, Slavin SA, Lin SJ. Gossypiboma: an approach to diagnosis in the era of medical tourism. Plast Reconstr Surg. 2014;133(3):443e–444e. doi: 10.1097/01.prs.0000438499.85598.53. [DOI] [PubMed] [Google Scholar]
- 12.Rüegg E, Cheretakis A, Modarressi A, Harbarth S, Pittet-Cuénod B. Multisite infection with mycobacterium abscessus after replacement of breast implants and gluteal lipofilling. Case Rep Infect Dis. 2015;2015:1–6. doi: 10.1155/2015/361340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Livingston R, Berlund P, Eccles-Smith J, Sawhney R. the real cost of "cosmetic tourism" cost analysis study of "cosmetic tourism" complications presenting to a public hospital. Eplasty. 2015;28(15):e34. [PMC free article] [PubMed] [Google Scholar]
- 14.Cai SS, Chopra K, Lifchez SD. Management of mycobacterium abscessus infection after medical tourism in cosmetic surgery and a review of literature. Ann Plast Surg. 2016;77(6):678–682. doi: 10.1097/SAP.0000000000000745. [DOI] [PubMed] [Google Scholar]
- 15.Green DA, Whittier S, Greendyke W, Win C, Chen X, Hamele-Bena D. Outbreak of rapidly growing nontuberculous mycobacteria among patients undergoing cosmetic surgery in the dominican republic. Ann Plast Surg. 2017;78(1):17–21. doi: 10.1097/SAP.0000000000000746. [DOI] [PubMed] [Google Scholar]
- 16.Rodríguez JY, Rodríguez GJ, Morales-López SE, Cantillo CE, Le Pape P, Álvarez-Moreno CA. Saksenaea erythrospora infection after medical tourism for esthetic breast augmentation surgery. Int J Infect Dis. 2016;49:107–110. doi: 10.1016/j.ijid.2016.05.032. [DOI] [PubMed] [Google Scholar]
- 17.Singh M, Dugdale CM, Solomon IH, Huang A, Montgomery MW, Pomahac B, Yawetz S, Maguire JH, Talbot SG. Rapid-growing mycobacteria infections in medical tourists: our experience and literature review. Aesthet Surg J. 2016;36(8):246–253. doi: 10.1093/asj/sjw047. [DOI] [PubMed] [Google Scholar]
- 18.Klein HJ, Simic D, Fuchs N, Schweizer R, Mehra T, Giovanoli P, Plock JA. Complications after cosmetic surgery tourism. Aesthet Surg J. 2017;37(4):474–482. doi: 10.1093/asj/sjw198. [DOI] [PubMed] [Google Scholar]
- 19.Adabi K, Stern CS, Weichman KE, Garfein ES, Pothula A, Draper L, Tepper OM. Population health implications of medical tourism. Plast Reconstr Surg. 2017;140(1):66–74. doi: 10.1097/PRS.0000000000003459. [DOI] [PubMed] [Google Scholar]
- 20.Farid M, Nikkhah D, Little M, Edwards D, Needham W, Shibu M. Complications of cosmetic surgery abroad - cost analysis and patient perception. Plast Reconstr Surg Glob Open. 2019;7(6):e2281. doi: 10.1097/GOX.0000000000002281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ovadja ZN, Sluijmer H, Moerman E, van Ogtrop M, Lapid O. Rapidly growing mycobacteria infections among "cosmetic tourists" returning to the Netherlands. J Plast Reconstr Aesthet Surg. 2018;71(2):265–267. doi: 10.1016/j.bjps.2017.10.023. [DOI] [PubMed] [Google Scholar]
- 22.Lee JC, Morrison KA, Maeng MM, Ascherman JA, Rohde CH. Financial implications of atypical mycobacterial infections after cosmetic tourism: is it worth the risk? Ann Plast Surg. 2018;81(3):269–273. doi: 10.1097/SAP.0000000000001563. [DOI] [PubMed] [Google Scholar]
- 23.Jensen E, Holst-Albrechtsen S, Christensen KØ, Birk-Sørensen L, Juel J. Mycobacterium abscessus infection after cosmetic breast surgery in India. Ugeskr Laeger. 2018;180(7):V09170655. [PubMed] [Google Scholar]
- 24.Parel-Amini L, Uçkay I, Rüegg EM, Homsy A, Pittet-Cuénod B, Modarressi A. Les enjeux du tourisme chirurgical dans le domaine de la chirurgie esthétique [The challenges of surgical tourism in the field of aesthetic surgery] Ann Chir Plast Esthet. 2019;64(4):293–297. doi: 10.1016/j.anplas.2019.06.006. [DOI] [PubMed] [Google Scholar]
- 25.Zheng C, Quentzel J, Brust JCM. Complications of silicone cosmetic procedures among medical tourists from the bronx, New York: a retrospective analysis. J Clin Aesthet Dermatol. 2019;12(10):24–28. [PMC free article] [PubMed] [Google Scholar]
- 26.Martin S, Long R, Hill C, Sinclair S. Cosmetic tourism in Northern Ireland. Ann Plast Surg. 2019;83(6):618–621. doi: 10.1097/SAP.0000000000002081. [DOI] [PubMed] [Google Scholar]
- 27.Miguel Escuredo I, Vicario Elorduy E, Guío Carrión L, Elvira Segura J, Iraurgui Arcarazo P, García Gutiérrez JJ. Mycobacterium abscessus infection after breast lipotransfer: a report of 2 cases. Plast Reconstr Surg Glob Open. 2020;8(8):e3063. doi: 10.1097/GOX.0000000000003063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jhaveri VV, Singhal D, Riedel S, Rowley CF, Nathavitharana RR. Surgical cure of clarithromycin resistant Mycobacterium chelonae breast implant infection: a case report and review of the literature. J Clin Tuberc Other Mycobact Dis. 2020;5(21):100183. doi: 10.1016/j.jctube.2020.100183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jones DJ, Bunn F, Bell-Syer SV. Prophylactic antibiotics to prevent surgical site infection after breast cancer surgery. Cochrane Database Syst Rev. 2014 doi: 10.1002/14651858.CD005360.pub4. [DOI] [PubMed] [Google Scholar]
- 30.National Institute for Health and Clinical Excellence (NICE). (2020) Surgical site infection: prevention and treatment. Available at: https://www.nice.org.uk/guidance/ng125/chapter/Recommendations. Accessed November 10th [PubMed]
- 31.Hardwicke JT, Bechar J, Skillman JM. Are systemic antibiotics indicated in aesthetic breast surgery? a systematic review of the literature. Plast Reconstr Surg. 2013;131(6):1395–1403. doi: 10.1097/PRS.0b013e31828bd752. [DOI] [PubMed] [Google Scholar]
- 32.Padilla P, Ly P, Dillard R, Boukovalas S, Zapata-Sirvent R, Phillips LG. Medical tourism and postoperative infections. Plast Reconstr Surg. 2018;142(6):1644–1651. doi: 10.1097/PRS.0000000000005014. [DOI] [PubMed] [Google Scholar]
- 33.Schobersberger W, Schobersberger B, Partsch H. Travel-related thromboembolism: mechanisms and avoidance. Expert Rev Cardiovasc Ther. 2009;7(12):1559–1567. doi: 10.1586/erc.09.142. [DOI] [PubMed] [Google Scholar]
- 34.Brightman L, Ng S, Ahern S, Cooter R, Hopper I. Cosmetic tourism for breast augmentation: a systematic review. ANZ J Surg. 2017 doi: 10.1111/ans.14326. [DOI] [PubMed] [Google Scholar]
- 35.Foley BM, Haglin JM, Tanzer JR, Eltorai AEM. Patient care without borders: a systematic review of medical and surgical tourism. J Travel Med. 2019 doi: 10.1093/jtm/taz049. [DOI] [PubMed] [Google Scholar]
- 36.Jeevan R, Birch J, Armstrong AP. Travelling abroad for aesthetic surgery: Informing healthcare practitioners and providers while improving patient safety. J Plast Reconstr Aesthet Surg. 2011;64(2):143–147. doi: 10.1016/j.bjps.2010.04.022. [DOI] [PubMed] [Google Scholar]
- 37.Asher CM, Fleet M, Jivraj B, Bystrzonowski N. Cosmetic tourism: a costly filler within the national health service budget or a missed financial opportunity? a local cost analysis and examination of the literature. Aesthetic Plast Surg. 2020;44(2):586–594. doi: 10.1007/s00266-019-01571-7. [DOI] [PubMed] [Google Scholar]
- 38.Campbell A, Restrepo C, Navas G. Patient satisfaction with medical tourism: a review of 460 international plastic surgery patients in Colombia. Plast Reconstr Surg Glob Open. 2020;8(12):e3230. doi: 10.1097/GOX.0000000000003230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Long R, Martin S, Hill C. Cosmetic tourism amidst the covid-19 global pandemic. J Plast Reconstr Aesthet Surg. 2020;S1748–6815(20):30430–30437. doi: 10.1016/j.bjps.2020.08.128. [DOI] [PMC free article] [PubMed] [Google Scholar]