Abstract
Work contributes to health and health inequity in complex ways. The traditional exposure-disease framework used in occupational health research is not equipped to address societal contexts in which work is embedded. The political economy approach to public health directly examines macro-level societal contexts, but the attention to work in this literature is mostly on unemployment. As a result, we have limited understanding of work as a social determinant of health and health inequity. To fill this gap, we propose a conceptual framework that facilitates research on work, health, and health equity in institutional contexts. As an illustration of different social institutions creating different work-related health, we present characteristics of work and health in the United States and the European Union using the 2015 Working Conditions Surveys data. The results also highlight limitations of the traditional exposure-disease approach used in occupational health research. Applying the proposed framework, we discuss how work and health could be investigated from a broader perspective that involves multiple social institutions and the sociopolitical values that underpin them. Such investigations would inform policy interventions that are congruent with existing social institutions and thus have the potential for being adopted and effective. Further, we clarify the role of research in generating knowledge that would contribute to institutional change in support of population health and health equity.
Keywords: United States, European union, Occupational safety and health, Social determinants of health, Political economy, Welfare regime
Highlights
-
•
Occupational health research decontextualizes work from other social institutions.
-
•
The political economy approach can help contextualize work and health in society.
-
•
Studying work and health in institutional contexts offers new perspectives.
-
•
Researchers play an important role in institutional change toward health equity.
Introduction
Clare Bambra opens her 2011 book on work, worklessness, and health by stating, “Work is the most important determinant of population health and health inequalities” (Bambra, 2011b, p. ix). Most of our knowledge about work and health has been accumulated within a framework of exposure and disease, in which researchers compare the health of workers with varying degrees of exposure and then explore physiological pathways that link the exposure to disease (Kant & van Amelsvoort, 2017; Rosenstock & Landrigan, 1986). Originally applied to physical, chemical, and biological hazards in the workplace, this exposure-disease framework has guided investigations of other types of hazards as well, such as job stress and shiftwork. It has been useful in examining specific hazards and their specific health impacts (Cullen, 1999; Rosenstock & Landrigan, 1986); however, it does not offer systematic ways to investigate societal factors that determine the level or distribution of exposure (Rose, 1985). In a separate literature, work has been examined as a marker of social class; however, health differences across social class tend to be attributed to differences either in income and education (Wilkinson, 2002) or in job control (Bosma et al., 1997). Because these differences are studied mostly in an exposure-disease framework, they provide relatively little understanding of how society creates these differences, or how we reduce the overrepresentation of marginalized groups in unfavorable work situations. These are crucial questions in redressing health inequity, and to answer them we must incorporate societal factors in the research on work and health.
Societal forces at a macro-level that create health and health inequity are most explicitly examined in the literature of political economy and public health, which argues that “the behavioral and social determinants of health are themselves shaped by macro-level structural determinants […] the structures, values, and priorities of political and economic systems” (Bambra, 2019, p. 833). Motivated to understand international variations in health and health inequity, researchers have compared political systems that have different arrangements for distributing services such as medical care, education, and unemployment protection. There have been calls for investigating health impacts of work in the context of political economy (Bambra, 2011a; Burgard & Lin, 2013; McLeod et al., 2012), but studies in this field have focused mostly on unemployment (McLeod et al., 2012) and insecure employment (Kim et al., 2012).
This limited attention to work has resulted in a missed opportunity for mitigating health inequity. The wealth of knowledge in occupational safety and health research suggests concrete policy interventions that would make work safer and health-enhancing for everyone. Because improvements in work would benefit those in the worst work situations the most, occupational safety and health policy interventions could be powerful tools to reduce health inequity. However, recommendations developed within an exposure-disease framework may not be adopted or effective if they are incongruent with existing values and institutions. To develop useful policy recommendations, we must examine work as a social determinant of health and health inequity with an explicit focus on how it is embedded in social institutions. The political economy approach to public health could bring this perspective.
In this paper, we propose a conceptual framework that guides health inequity research from an integrated perspective of political economy and occupational health. It is informed by Muntaner and colleagues' macro-level model (2010), which highlights the social origins of employment conditions and health inequity; and by Diderichsen, Evans, & Whitehead (2009), which clarifies the multiple roles society can play in both contributing to health inequity and potentially preventing it. Following the introduction of the framework, we compare characteristics of work and health in the European Union and the United States as an illustration of different work-related health in different social contexts. This exercise also highlights the limitations of the traditional exposure-disease approach. Based on the observations, we discuss how our framework may guide new types of research questions embedded in societal contexts. We conclude by pointing out possibilities for institutional change and the role of research in the process.
The work-health relationship in social contexts: A conceptual framework
Sociopolitical values as common roots of social institutions
This framework distinguishes historical, cultural, economic, and political values and priorities in society (sociopolitical values hereafter) from more tangible social structures, policies, and practices (social institutions hereafter) which embody sociopolitical values. Social institutions are developed, accepted, and maintained only if they correspond with prevailing sociopolitical values (Hall & Taylor, 1996). The distinction between values and institutions becomes useful in considering institutional change. If existing institutions are harmful to the health of some members of society and thus create health inequity, they need to be changed. The theory of discursive institutionalism (Schmidt, 2008, 2011) recognizes the power of discourse, or the ability to discuss values that would require new types of social institutions, as an impetus for institutional change. We will turn to discursive institutionalism and institutional change in a later section.
Institutions that create health-damaging and health-enhancing conditions
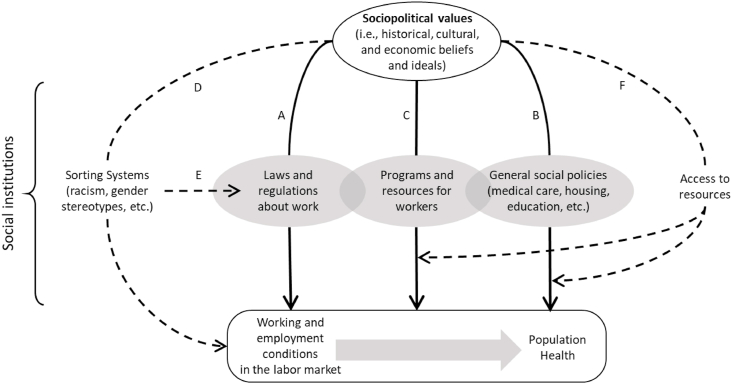
With a specific emphasis on work, we identify three types of social institutions that create variations in health-relevant conditions: work and employment (Arrow A in Fig. 1), general social policies (Arrow B), and resources for working people (Arrow C). The first type, work-related laws and regulations, determines what kinds of working and employment conditions exist in the labor market (Arrow A), characterized by minimum wage, work hours, employment protection, safety regulations, workplace inspections, and so on. Sociopolitical values, which include economic ideologies and priorities, are reflected in this type of social institution. While it is well documented that the variation in working and employment conditions contributes to the variation in health (Cullen, 1999; Peckham et al., 2019; Rosenstock & Landrigan, 1986; Van Aerden et al., 2016), only a few studies have investigated sociopolitical values and working conditions (e.g., Bambra et al., 2014; Bartoll et al., 2014; Dragano et al., 2011), and the findings are not entirely consistent.
Fig. 1.
A framework for adressing population health from the perspective of work. Solid lines indicacte mechanisms that create health-damaging and health-enhancing conditions. Dotted lines indicate mechanisms that place people in health-damaging and health-enhancing conditions.
A second type of social institution is what we call general social policies (Arrow B), which do not directly address work but have consequences for working people as members of society (Krieger, 2010). These policies pertain to, for example, education, taxation, medical care, housing, urban planning, transportation, and environmental protection. Because these are social determinants of health, the range of health in society would correspond to the range of conditions these social institutions create. Arrow B is generally supported by the literature on political economy and public health (Bergqvist et al., 2013; McCartney et al., 2019).
A third type of social institution pertains to services and resources for people experiencing certain circumstances such as health problems, job loss, temporary or long-term disability, and caregiving responsibilities (Arrow C). Some resources are specifically for working people in need: for example, sick leave, parental leave, wage replacement and medical benefits in case of occupational injury or illness, and unemployment benefits. Some of these resources may be available through employment and thus overlap with Arrow A. Others are for all members of society and therefore overlap with general social institutions on Arrow B; examples are affordable childcare, reasonable housing options, and reliable public transportation. The overlap among the three types of social institutions—that is, who provides what resources to whom and how—vary by society, reflecting its particular sociopolitical values.
Support for Arrow C can be found in comparative studies on health consequences of unemployment. The association between unemployment and poor health differs across societies, and the differences are explained by the generosity of the benefits (Cylus et al., 2015; Ferrarini et al., 2014; Shahidi et al., 2016). The generosity varies because, we argue, societies find different levels of support appropriate within their sociopolitical values. In fact, public attitudes toward social assistance have been shown to modify the unemployment-health relationship (Shahidi et al., 2016).
Mechanisms that place people in health-damaging and health-enhancing conditions
In any society, certain population subgroups—defined by age, gender, race/ethnicity, religion, tribe, or other social demarcations relevant to the society—are systematically placed into health-damaging conditions and therefore are likely to experience poor health. First, sorting systems determine who works in what kinds of jobs (Hudson, 2007) (Arrow D). For example, gender stereotypes and job segregation in self-fulfilling ways affect which jobs men and women have. The different working conditions men and women experience as a result can impact their health status. In addition, sorting systems and resulting segregation may tacitly influence the effectiveness of occupational safety and health regulations (Arrow E). Immigrants are more likely to be self-employed or employed in small establishments (Hazans, 2011). If small businesses are exempt from certain labor laws, immigrant workers would be less protected. A vast majority of care workers—e.g., kindergarten teachers, nurses’ aides, hotel room cleaners—are women. Campos-Serna, Ronda-Pérez, Artazcoz, Moen, and Benavides (2013) argue that the traditional view of women as caregivers not only sorts women into this type of work but also makes society tolerate poor working and employment conditions that women endure in these jobs.
A third way for social institutions to create health inequity is through differential access to resources (Arrow F). Generous programs and services may exist both for workers and for the general public, but access to such resources may not be universal. For example, reliable public transportation may be available only to workers in large cities. Resources in case of occupational injury and illness (e.g. first aid, on-site medical services, income replacement, and medical benefits) may not be available for self-employed workers. Responsibilities for providing these resources vary by society (as shown in overlap among Arrows A, B, and C), and so do the mechanisms to manage access to them (e.g., universal access, social insurance, and means-tested access).
Seeing the COVID-19 pandemic using the framework
The COVID-19 pandemic provides a vivid example of work being intertwined with various social institutions. During the pandemic's early stage, the essential business designation (Arrow A) created vastly different work situations: while some workers continued working in the safety of their homes, others took on heavier workloads, longer work hours, and/or higher risks of the infection, and many others lost hours or their jobs entirely because the need for the work or service diminished. Women, ethnic minorities, and people with limited education were overrepresented in jobs that were intensified, involved high risk, or were lost (Arrow D) (Blau et al., 2020; Montenovo et al., 2020). The operations of schools, childcare facilities, and public transportation were limited, and peoples' movements restricted (Arrow B), all of which could impact workers' ability to work. Many societies provided emergency relief funds to individuals and businesses, expanded paid leave and unemployment benefits, and banned evictions and utility shutoffs (Arrow C). The scope of these relief efforts and the access to them, however, varied widely by locale, citizenship or documentation status, pre-pandemic employment conditions and many other factors (Arrows F).
Because these extensive policy responses simultaneously impact people's work, health, and well-being, the effect of any policy response cannot be understood in isolation by controlling for all other factors, as the exposure-disease approach would suggest. Policy responses are devised and implemented because, we argue, they correspond with existing institutions and sociopolitical values in each society. Income replacement, for example, could be provided as unemployment benefits or payroll subsidies. The level of resources allocated to these different implementations reflects existing employment protection: if it is easy to dismiss employees, more unemployment benefits are needed; if it is difficult, more payroll subsidies are needed. Employment protection, in turn, reflects economic ideologies and history of labor movements in a society. If some societies weather the COVID crisis better than others, researchers need to examine not only societies' policy responses across various domains but also the sociopolitical values that enabled particular combinations of policy responses. Such investigations could then inform strategies for institutional change that would allow societies to better withstand future crises.
While this is an application of the framework to an extraordinary situation, work in ordinary situations can also be better understood with particular attention to social institutions. In the next section, we compare the United States and the European Union on work-related health as an illustration of differences that can be produced under different sociopolitical values and social institutions. This illustration also highlights limitations of the traditional exposure-disease approach.
Illustration: health and working conditions in the United States and the European Union
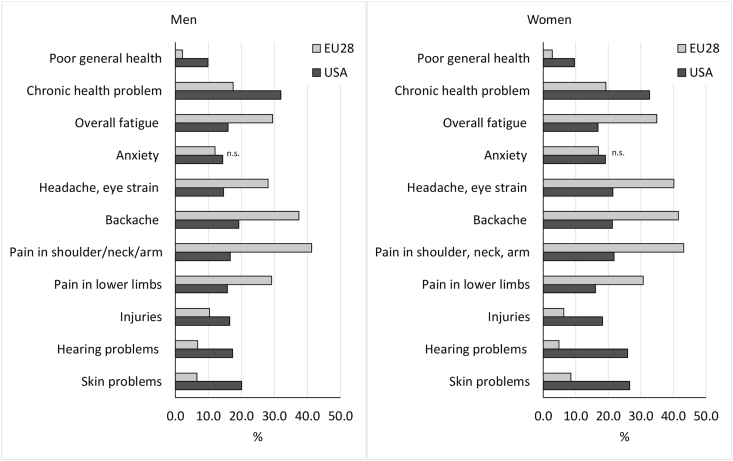
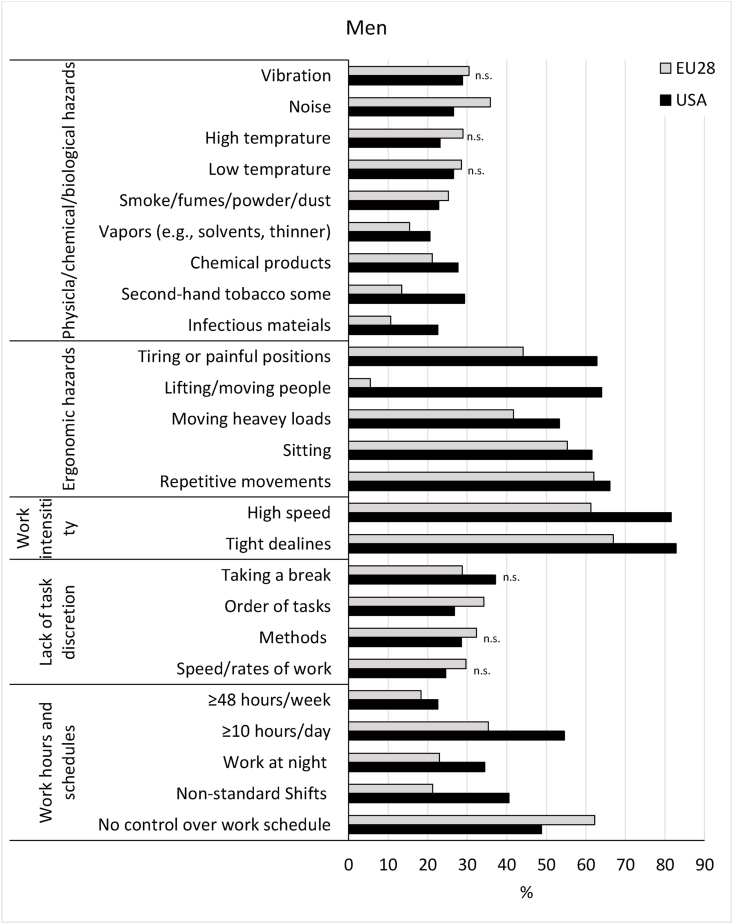
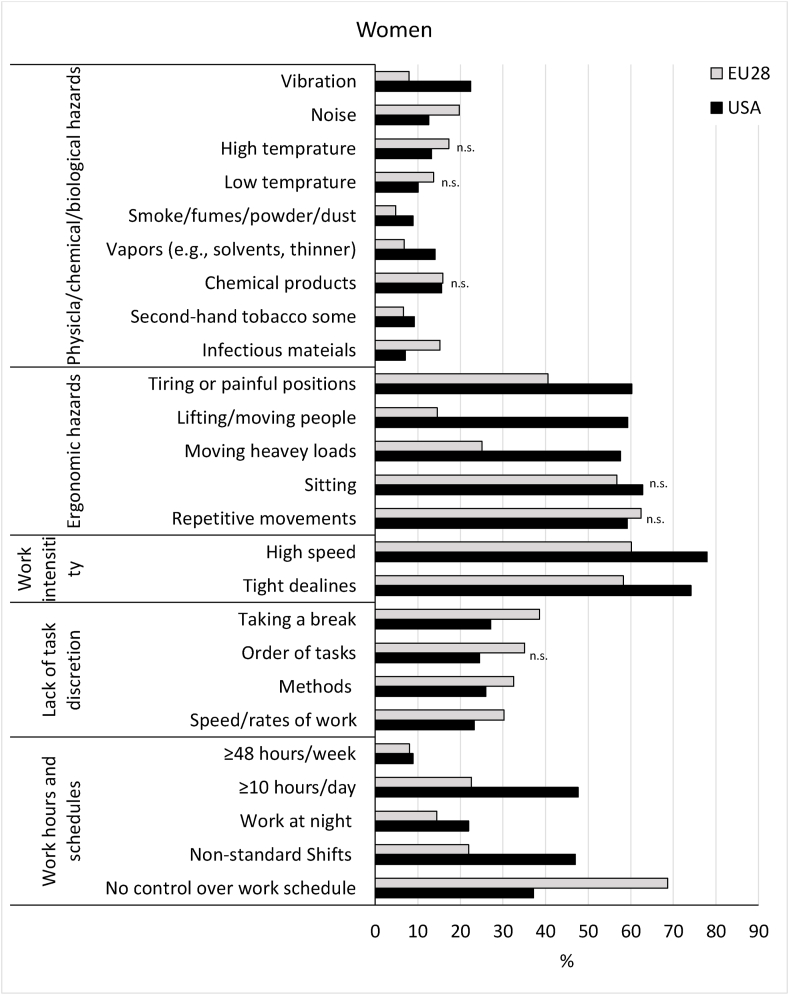
If health and working conditions are products of multiple social institutions supported by common sociopolitical values, we would see different levels of hazard exposure and related health in societies with different sociopolitical values. Assuming “significant political and institutional arrangements that differentiate the United States from other rich democracies” (Bambra, 2019, p. 834), we compare the United States and the 28 member states of the European Union (EU28) using data from the 2015 European and American Working Conditions Surveys, which are coordinated international surveys conducted with representative samples of working populations in participating countries (Eurofound & International Labour Organization, 2019). The full description of the data, sample, measures, and statistical approach is presented in Appendix. Fig. 2 shows age-adjusted proportions of workers in each region who reported poor health, and Fig. 3, Fig. 4 show comparisons of occupational hazard exposure between regions by gender. All results in table format are also available in Appendix.
Fig. 2.
Age-adjusted prevalence of poor health indicators among working men and women in the US and EU28, 2015. All differences between the two regions are statistically significant at the 0.05 level unless noted as “n.s.”
Fig. 3.
Age-adjusted prevalence of selected occupational hazard exposure among working men in the US and EU28, 2015. All differences between the two regions are statistically significant at the 0.05 level unless noted as “n.s.”
Fig. 4.
Age-adjusted prevalence of selected occupational hazard exposure among working women in the US and EU28, 2015. All differences between the two regions are statistically significant at the 0.05 level unless noted as “n.s.”
Limitations of the exposure-disease framework
The side-by-side description of US and EU28 workers’ health and working conditions showed considerable differences but no consistent advantages in either region. Nor did it show clear patterns in observed regional differences in working conditions and their presumed associations with health. For example, a higher proportion of EU workers reported muscular pains, yet ergonomic hazard exposure was more often reported by US workers. Similarly, hearing problems were more common among US workers, but a higher proportion of EU workers reported noise exposure. In a traditional exposure-disease framework, these incongruencies would be attributed to technical problems such as measurement error (e.g., self-reported data are unreliable), cross-sectional data (i.e., causality cannot be determined), sample representativeness (e.g., recruitment processes are different), and the crude nature of the comparison (e.g., only age and gender were controlled in the prevalence estimates and no multivariate analyses were done). All these are legitimate concerns if the investigation were meant to establish a causal association between, for example, ergonomic hazard exposure and muscular pains. In fact, for that purpose, international surveys would not be the most suitable data sources. However, these seemingly incongruent patterns that we observed can prompt further exploration of social institutions.
Understanding work and health through multiple social institutions
One of the stark differences we see is in the proportion of workers reporting poor general health: <3% in the EU28 and >9% in the US (Fig. 2). Because the proportion in the general population is about 9% in both regions (Eurostat, 2020; National Health Interview Survey, 2018), the difference among workers indicates that EU28 may have a stronger healthy worker effect (i.e., only people who are healthy enough to work are in the workforce). Consistent with this finding, we see a higher proportion of US workers reporting chronic health conditions than EU28 workers. These differences could be better understood if we consider multiple social institutions together. The return-to-work literature identifies social institutions with different functions as important determinants for people with health problems to engage in paid labor (Islam et al., 2014). They include the employer's responsibility for providing accommodation and medical insurance (Arrow A), the cost of medical care to the individual and post-retirement financial provisions (Arrow B), financial assistance during illness, and disability benefits (Arrow C). Additionally, subgroup differences (inequity) can become apparent by considering the characteristics of the people who have a job with medical insurance, paid sick leave, and other benefits (Arrow D), as well as those who have access to medical care and financial assistance (Arrow F). Because most studies focus on one factor at a time, they do not make clear if returning to work after health problems is beneficial. Our framework would help researchers discover specific combinations of cooccurring institutional characteristics under which workers can benefit from, or harmed by, returning to work.
Considering multiple working conditions together rather than in isolation could also suggest broader intervention approaches that involve multiple social institutions. Compared to EU workers, higher proportions of US workers report ergonomic risks, high work intensity, long workdays, and night and shift work (Fig. 3, Fig. 4). Injury rates are higher among US workers (Fig. 2), which may be explained by US workers having these more demanding working conditions in addition to having poorer general health. If workers are physically vulnerable because of poor health and demanding working conditions, injury prevention programs that focus only on workplace safety (Arrow A) may have limited effect. Our framework suggests a wider range of social institutions to be engaged for injury prevention, such as providing resources that allow people with health problems to stay home or work with appropriate accommodations (Arrows B and C), as well as making sure these resources reach all workers who need them (Arrows D and F).
Significant differences in occupational hazard exposure in the side-by-side comparisons indicate that the rates could be reduced at least to the level of the region with the lower rate. However, this lower rate does not necessarily mean that the level is acceptable. For example, a sizable proportion of workers in both regions reported lack of task discretion. Low levels of job control have been well-documented as a predictor of poor health, ranging from cardiovascular disease (Bosma et al., 1997) to all-cause mortality (Amick et al., 2002). Also, high work intensity was reported by a vast majority of workers in both regions. If the scientific consensus has not been used in creating laws and regulations (i.e., Arrow A is blocked), our framework suggests that sociopolitical values need to change so that social institutions related to labor practice may change.
We have illustrated our framework using data from two high-income multi-state regions, but the general relationships among the factors hold in lower-income countries as well. Costa Rica, a middle-income country, achieves remarkably good population health status despite modest national economic resources. Campbell Barr and Michael (2020) attribute Costa Rica's success to “the decision to cease investment in national defense” (p. e2), which is a sociopolitical value that “free[s] up money to invest in health, education, and the welfare of the population” (p. e2). The specific ways these institutions were shaped embody the country's sociopolitical values (Arrow B). Nonetheless, health inequities still exist in Costa Rica for lower-income, indigenous, and Afro-descendant populations (Campbell Barr & Michael, 2020). These social demarcations suggest that sorting mechanisms are likely to influence who does what kind of work (Arrow D), and whose work is regulated and protected (Arrow E). Supportive programs for workers may exist (Arrow C), but the proportion of informal labor in the country (i.e., 35–40%) (Pasquali, 2020) suggests potentially uneven access (Arrow F) if programs are designed under the assumption of formal employment. The complexity of all these factors emphasizes the importance of considering work and health in societal contexts.
How social institutions can change to support population health and health equity
Existing social institutions have the power to maintain current sociopolitical values and thus resist changes, as earlier institutional theories describe (Hall & Taylor, 1996). For example, environmental health and occupational health in the United States are institutionally distinct under the separate laws and governmental agencies. As a result, people are divided into workers and residents, and their common demand for safe environment—both inside and outside the workplace—is weakened (Zoller, 2009). However, discursive institutionalism (Schmidt, 2008) recognizes that people can discuss ideas outside existing social institutions while their lives are still shaped by them. The difference between these outside ideas and current practices of social institutions can prompt action. Here, the possibility of change lies.
It is a long-term project to change an entire society's sociopolitical values and institutions; however, small-scale local efforts may be a promising starting point. Hagedorn and colleagues (2016) provide an example for workers changing local labor practices through union negotiations. Reviewing union contracts in a wide range of industries in the US Pacific Northwest, they found that union contracts achieved more than safer working conditions and higher wages: the workers gained a more balanced relationship with employers so that they did not have to sacrifice personal and family needs in order to keep their jobs. Sociopolitical values may have shifted as a result of these union activities, and the social institutions related to work in the Pacific Northwest may now conform to these new values.
Researchers have a crucial role to play in institutional change: how they do research has consequences in either maintaining or changing existing social institutions. To highlight this point, we contrast two surveillance reports on COVID-19 among workers published in a same journal. Kambhampati and colleagues (2020) described characteristics of healthcare workers who had COVID-19. With detailed clinical information (e.g., underlying chronic medical conditions, exam findings, treatments, and the outcome), the authors concluded that obesity prevention and healthy lifestyles were important to reduce healthcare workers' risk for poor COVID-related outcomes. Decontextualizing healthcare workers' COVID-19 experiences, this study maintained the discourse of biomedical risk factors and personal responsibility for health. In contrast, Rubenstein and colleagues (2020) distinguished structural factors (e.g., job tasks, housing arrangements, transportation options) from behavioral factors (e.g., social gathering, use of masks), both relevant to COVID transmission. In their sample of poultry processing workers, foreign-born workers were less likely to engage in high-risk behaviors but more likely to experience high-risk structural factors both inside and outside of the workplace (e.g., physical proximity with coworkers, crowded housing, and shared rides to work). This study not only proposed immediately actionable workplace interventions but also presented a concrete way to discuss workers’ health embedded in a larger social context. Through this type of research, we can generate knowledge about work and health that would prompt institutional change toward a more equitable society.
Conclusions and future directions
Understanding working people's health with a clear awareness of its institutional contexts is imperative for developing policy interventions that make a difference. Our framework promotes “theory-driven data-informed” (Haardörfer, 2019) studies of work and health that incorporate the simultaneous influences of societal forces. Such investigations require high quality data that are comparable across time and place, and collecting these data requires long-term national and international collaboration and commitment. We need data at multiple levels—workers’ experiences and institutional structures at various levels of society. Some sociopolitical values may be captured in the general social opinion surveys that many countries conduct or can be inferred from existing institutional practices. Linking different sources of information takes not only technical savvy but also innovative thinking, which we hope our framework inspires. In addition to using existing data in unorthodox ways, researchers should take advantage of the power of qualitative research, whose major strengths include the discovery of meanings and mechanisms that are currently unknown and thus cannot be captured with close-ended survey questions. Collaborations with colleagues in social sciences and humanities will advance and enrich our thinking. Working with unions, employers, policy makers, and civic organizations will offer effective means for putting new ideas into institutional practices. It is our hope that the framework presented here opens avenues for productive interdisciplinary collaboration and research-practice integration.
Work, an essential part of society, is intertwined with various social institutions. Because it is a social determinant of health, improving the quality of work contributes to overall population health and reduces health inequity at the same time. Health inequity could be further reduced by ensuring access to resources for everyone and by dismantling sorting systems that systematically place certain subgroups in less healthy work. To contribute to this process, population health researchers must embrace the complexity of work and address it in its societal contexts.
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily reflect the official position of the National Institute for Occupational Safety and Health, Centers for Disease Control and Prevention.
Acknowledgement
Dr. Gimeno Ruiz de Porras is partially funded by the Southwest Center for Occupational and Environmental Health (SWCOEH), a NIOSH Education and Research Center at The University of Texas Health Science Center at Houston School of Public Health, and awardee of Grant No. T42OH008421 from the NIOSH/CDC.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ssmph.2021.100787.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Amick B.C., III, McDonough P., Chang H., Rogers W.H., Pieper C.F., Duncan G. Relationship between all-cause mortality and cumulative working life course psychosocial and physical exposures in the United States labor market from 1968 to 1992. Psychosomatic Medicine. 2002;64:370–381. doi: 10.1097/00006842-200205000-00002. [DOI] [PubMed] [Google Scholar]
- Bambra C. Work, worklessness and the political economy of health inequalities. Journal of Epidemiology & Community Health. 2011;65:746–750. doi: 10.1136/jech.2009.102103. [DOI] [PubMed] [Google Scholar]
- Bambra C. Oxford University Press; New York: 2011. Work, worklessness, and the political economy of health. [DOI] [PubMed] [Google Scholar]
- Bambra C. The political economy of the United States and the people's health. American Journal of Public Health. 2019;109:833–834. doi: 10.2105/AJPH.2019.305064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bambra C., Lunau T., Van Der Wel K., Eikemo T., Dragano N. Work, health, and welfare: The association between working conditions, welfare states, and self-reported general health in Europe. International Journal of Health Services. 2014;44:113–136. doi: 10.2190/HS.44.1.g. [DOI] [PubMed] [Google Scholar]
- Bartoll X., Cortès I., Artazcoz L. Full-and part-time work: Gender and welfare-type differences in European working conditions, job satisfaction, health status, and psychosocial issues. Scandinavian Journal of Work, Environment & Health. 2014:370–379. doi: 10.5271/sjweh.3429. [DOI] [PubMed] [Google Scholar]
- Bergqvist K., Yngwe M.Å., Lundberg O. Understanding the role of welfare state characteristics for health and inequalities–an analytical review. BMC Public Health. 2013;13:1234. doi: 10.1186/1471-2458-13-1234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blau F.D., Koebe J., Meyerhofer P.A. National Bureau of Economic Research; 2020. Who are the essential and frontline workers? (No. w27791) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bosma H., Marmot M.G., Hemingway H., Nicholson A.C., Brunner E., Stansfeld S.A. Low job control and risk of coronary heart disease in Whitehall II (prospective cohort) study. BMJ. 1997;314:558. doi: 10.1136/bmj.314.7080.558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgard S.A., Lin K.Y. Bad jobs, bad health? How work and working conditions contribute to health disparities. American Behavioral Scientist. 2013;57:1105–1127. doi: 10.1177/0002764213487347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell Barr E., Michael M. Vol. 44. Revista Panamericana de Salud Pública; 2020. Leadership, social determinants of health and health equity: The case of Costa Rica. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campos-Serna J., Ronda-Pérez E., Artazcoz L., Moen B.E., Benavides F.G. Gender inequalities in occupational health related to the unequal distribution of working and employment conditions: A systematic review. International Journal for Equity in Health. 2013;12:57. doi: 10.1186/1475-9276-12-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cullen M.R. Annual review of public health. Vol. 20. 1999. Personal reflections on occupational health in the twentieth century: Spiraling to the future; pp. 1–13. [DOI] [PubMed] [Google Scholar]
- Cylus J., Glymour M.M., Avendano M. Health effects of unemployment benefit program generosity. American Journal of Public Health. 2015;105:317–323. doi: 10.2105/AJPH.2014.302253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diderichsen F., Evans T., Whitehead M. Challenging inequities in health: From ethics to action. Oxford Scholarship Online; 2009. The social basis of disparities in health.https://oxford.universitypressscholarship.com/view/10.1093/acprof:oso/9780195137408.001.0001/acprof-9780195137408-chapter-2 [Google Scholar]
- Dragano N., Siegrist J., Wahrendorf M. Welfare regimes, labour policies and unhealthy psychosocial working conditions: A comparative study with 9917 older employees from 12 European countries. Journal of Epidemiology & Community Health. 2011;65:793–799. doi: 10.1136/jech.2009.098541. [DOI] [PubMed] [Google Scholar]
- Eurofound, International Labour Organization . Publications Office of the European Union, Luxembourg, and ILO; Geneva: 2019. Working conditions in a global perspective. [Google Scholar]
- Eurostat . European Commission; 2020. Self-perceived health statistics.https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Self-perceived_health_statistics#Self-perceived_health [Google Scholar]
- Ferrarini T., Nelson K., Sjöberg O. Decomposing the effect of social policies on population health and inequalities: An empirical example of unemployment benefits. Scandinavian Journal of Public Health. 2014;42:635–642. doi: 10.1177/1403494814546349. [DOI] [PubMed] [Google Scholar]
- Haardörfer R. Taking quantitative data analysis out of the positivist era: Calling for theory-driven data-informed analysis. Health Education & Behavior. 2019;46:537–540. doi: 10.1177/1090198119853536. [DOI] [PubMed] [Google Scholar]
- Hagedorn J., Paras C.A., Greenwich H., Hagopian A. The role of labor unions in creating working conditions that promote public health. American Journal of Public Health. 2016;106:989–995. doi: 10.2105/AJPH.2016.303138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall P.A., Taylor R.C. Political science and the three new institutionalisms. Political Studies. 1996;44:936–957. [Google Scholar]
- Hazans M. World Bank Policy Research Working Paper; 2011. Informal workers across europe: Evidence from 30 European countries.https://elibrary.worldbank.org/doi/abs/10.1596/1813-9450-5912 [Google Scholar]
- Hudson K. The new labor market segmentation: Labor market dualism in the new economy. Social Science Research. 2007;36:286–312. [Google Scholar]
- Islam T., Dahlui M., Majid H.A., Nahar A.M., Taib N.A.M., Su T.T. BMC public health. Springer; 2014. Factors associated with return to work of breast cancer survivors: A systematic review; p. S8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kambhampati A.K., O'Halloran A.C., Whitaker M., Magill S.S., Chea N., Chai S.J. COVID-19–Associated hospitalizations among health care personnel—COVID-NET, 13 states, march 1–may 31, 2020. Morbidity and Mortality Weekly Report. 2020;69:1576–1583. doi: 10.15585/mmwr.mm6943e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kant I., van Amelsvoort L.G. Applying a biopsychosocial perspective in occupational health: Easier said than done! Work. 2017;57:149–151. doi: 10.3233/WOR-172550. [DOI] [PubMed] [Google Scholar]
- Kim I.H., Muntaner C., Vahid Shahidi F., Vives A., Vanroelen C., Benach J. Welfare states, flexible employment, and health: A critical review. Health Policy. 2012;104:99–127. doi: 10.1016/j.healthpol.2011.11.002. [DOI] [PubMed] [Google Scholar]
- Krieger N. Workers are people too: Societal aspects of occupational health disparities—an ecosocial perspective. American Journal of Industrial Medicine. 2010;53:104–115. doi: 10.1002/ajim.20759. [DOI] [PubMed] [Google Scholar]
- McCartney G., Hearty W., Arnot J., Popham F., Cumbers A., McMaster R. Impact of political economy on population health: A systematic review of reviews. American Journal of Public Health. 2019;109:E1–E12. doi: 10.2105/AJPH.2019.305001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLeod C.B., Hall P.A., Siddiqi A., Hertzman C. How society shapes the health gradient: Work-related health inequalities in a comparative perspective. Annual Review of Public Health. 2012;33:59–73. doi: 10.1146/annurev-publhealth-031811-124603. [DOI] [PubMed] [Google Scholar]
- Montenovo L., Jiang X., Rojas F.L., Schmutte I.M., Simon K.I., Weinberg B.A. National Bureau of Economic Research; 2020. Determinants of disparities in COVID-19 job losses (No. w27132) [Google Scholar]
- Muntaner C., Chung H., Solar O., Santana V., Castedo A., Benach J. A macro-level model of employment relations and health inequalities. International Journal of Health Services. 2010;40:215–221. doi: 10.2190/HS.40.2.d. [DOI] [PubMed] [Google Scholar]
- National Health Interview Survey . 2018. Table P-1a: Age-adjusted percent distribution of respondet-assessed health status, by selected characteristics. United States. [Google Scholar]
- Pasquali M. 2020. Informal employment as percentage of total employment in Costa Rica from 2011 to 2019.https://www.statista.com/statistics/1039933/informal-employment-share-costa-rica/ (Statista) [Google Scholar]
- Peckham T., Fujishiro K., Hajat A., Flaherty B.P., Seixas N. Evaluating employment quality as a determinant of health in a changing labor market. RSF: The Russell Sage Foundation Journal of the Social Sciences. 2019;5:258–281. doi: 10.7758/RSF.2019.5.4.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rose G. Sick individuals and sick populations. International Journal of Epidemiology. 1985;14:32–38. doi: 10.1093/ije/14.1.32. [DOI] [PubMed] [Google Scholar]
- Rosenstock L., Landrigan P.J. Occupational health: The intersection between clinical medicine and public health. Annual Review of Public Health. 1986;7:337–356. doi: 10.1146/annurev.pu.07.050186.002005. [DOI] [PubMed] [Google Scholar]
- Rubenstein B.L., Campbell S., Meyers A.R., Crum D.A., Mitchell C.S., Hutson J. Factors that might affect SARS-CoV-2 transmission among foreign-born and US-born poultry facility workers—Maryland. Morbidity and Mortality Weekly Report. 2020;69:1906–1910. doi: 10.15585/mmwr.mm6950a5. May 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt V.A. Discursive institutionalism: The explanatory power of ideas and discourse. Annual Review of Political Science. 2008;11:303–326. [Google Scholar]
- Schmidt V.A. Reconciling ideas and institutions through discursive institutionalism. In: Béland D., Cox R.H., editors. Ideas and politics in social science research. Oxford University Press; 2011. pp. 76–95. [Google Scholar]
- Shahidi F.V., Siddiqi A., Muntaner C. Does social policy moderate the impact of unemployment on health? A multilevel analysis of 23 welfare states. The European Journal of Public Health. 2016;26:1017–1022. doi: 10.1093/eurpub/ckw050. [DOI] [PubMed] [Google Scholar]
- Van Aerden K., Puig-Barrachina V., Bosmans K., Vanroelen C. How does employment quality relate to health and job satisfaction in europe? A typological approach. Social Science & Medicine. 2016;158:132–140. doi: 10.1016/j.socscimed.2016.04.017. [DOI] [PubMed] [Google Scholar]
- Wilkinson R.G. Routledge; 2002. Unhealthy societies: The afflictions of inequality. [Google Scholar]
- Zoller H.M. The social construction of occupational health and safety: Barriers to environmental-labor health coalitions. New Solutions. 2009;19:289–314. doi: 10.2190/NS.19.3.b. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.