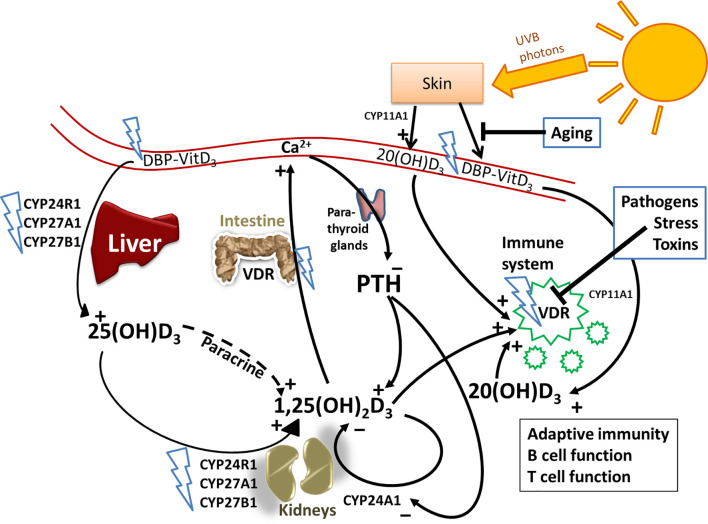
Figure 1.
Vitamin D metabolism and the sites of vitamin D resistance acquirement. Vitamin D3 is mainly produced in the skin through solar ultraviolet-B (UVB) radiation and gets transported through blood by binding to vitamin D binding protein (DBP). The liver is the systemic production site of 25(OH)D3 via the enzymes CYP2R1, CYP27A1 or CYP27B1. 25(OH)D3 then gets converted to the active hormone 1,25(OH)2D3 by a second hydroxylation which occurs mainly in the kidneys or in other tissues through paracrine production. 1,25(OH)2D3 binds to the vitamin D receptor (VDR) to promote intestinal calcium (Ca) absorption and other Ca-mobilization pathways (e.g. in bone), so that ionized Ca levels in serum rise. The paraythroid glands sense Ca2+ levels, and secrete parathyroid hormone (PTH). PTH in turn promotes the production of 1,25(OH)2D3, e.g. by inhibiting CYP24A1 which catalyzes the first degradation step of 1,25(OH)2D3. Besides 1,25(OH)2D3, there are other vitamin D3-derived hydroxy-metabolites that exert hormone-like actions. For example, skin also expresses CYP11A1, which promotes the conversion of vitamin D3 into 20(OH)D3, which has non-calcemic biological effects, for example on immune cells. The blue flashes show where polymorphisms can interfere with normal vitamin D metabolism, building the basis for the development of acquired vitamin D resistance. Additional factors that impair vitamin D signaling are highlighted in blue boxes.