Abstract
Aims
Suicide attempt is an important indicator of suicide and potential future mortality. However, the prevalence of suicide attempts has been inconsistent across studies. This meta-analysis aimed to examine the prevalence of suicide attempts in individuals with schizophrenia and associated correlates.
Methods
Relevant publications in Embase, PsycINFO, PubMed, Web of science and Cochrane were systematically searched. Data on the prevalence of suicide attempts in individuals with schizophrenia were pooled using a random-effects model.
Results
Thirty-five studies with 16 747 individuals with schizophrenia were included. The pooled lifetime prevalence of suicide attempts was 26.8% (95% CI 22.1–31.9%; I2 = 97.0%), while the 1-year prevalence, 1-month prevalence and the prevalence of suicide attempts from illness onset were 3.0% (95% CI 2.3–3.7%; I2 = 95.6%), 2.7% (95% CI 2.1–3.4%; I2 = 78.5%) and 45.9% (95% CI 42.1–49.9%; I2 = 0), respectively. Earlier age of onset (Q = 4.38, p = 0.04), high-income countries (Q = 53.29, p < 0.001), North America and Europe and Central Asia (Q = 32.83, p < 0.001) were significantly associated with a higher prevalence of suicide attempts.
Conclusions
Suicide attempts are common in individuals with schizophrenia, especially those with an early age of onset and living in high-income countries and regions. Regular screening and effective preventive measures should be implemented as part of the clinical care.
Key words: Meta-analysis, schizophrenia, suicide attempt
Introduction
Schizophrenia is a chronic and severe psychiatric disorder with a massive global health burden, accounting for 7.4% (5.0–9.8) of disability-adjusted life years caused by mental and substance use disorders (Bhugra, 2005; Whiteford et al., 2013). Compared with the general population, persons with schizophrenia have 3.7 times higher risk of premature death (Olfson et al., 2015); men and women with schizophrenia have a reduced life-expectancy of around 19 and 16 years, respectively (Laursen, 2011). Among those with schizophrenia, the lifetime suicide rate is about 5% (Palmer et al., 2005; Hor and Taylor, 2010), and suicide is a major cause of premature death (Caldwell and Gottesman, 1992; Brown, 1997; Olfson et al., 2015). Prior suicide attempt is a major risk factor of suicide death (Hor and Taylor, 2010) and the lifetime prevalence of suicide attempts in individuals with schizophrenia ranged from 1.93% in Taiwan (Lee et al., 2012) to 55.1% in the USA (Roy et al., 1984).
Several demographic and clinical factors are associated with the risk of suicide attempts in persons with schizophrenia. For example, patients with comorbid depressive symptoms, a family history of suicide and multiple hospitalisations (Roy et al., 1984; Lee et al., 2012; Zhang et al., 2013) are at a higher risk of suicide attempts (Roy, 1983; Roy et al., 1984; Tremeau et al., 2005). Comorbid substance use (Togay et al., 2015; Fuller-Thomson and Hollister, 2016; Duko and Ayano, 2018) and more severe psychotic symptoms (Kao et al., 2012; Shrivastava et al., 2016) could also increase the risk of suicide attempts.
In order to develop effective preventive measures against suicide death, it is important to examine the epidemiology of suicide attempts in individuals with schizophrenia. However, the reported prevalence rates have been inconsistent across studies, probably due to discrepancy in study sampling, duration and regions with different economic levels. A meta-analysis of suicide-related behaviours in China found that the lifetime prevalence of suicide attempts was 14.6% in individuals with schizophrenia (Dong et al., 2017). To date there is no meta-analysis on the epidemiology of suicide attempts in person with schizophrenia worldwide. We thus conducted a meta-analysis of observational studies to examine the prevalence of suicide attempts in individuals with schizophrenia and associated factors.
Methods
Search strategy
This meta-analysis was performed in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines, and the protocol was registered in the International Prospective Register of Systematic Reviews (PROSPERO) with the registration number of CRD42018112863.
Two investigators (LL and MD) independently searched the databases of Embase, PsycINFO, PubMed, Web of science and Cochrane from their respective commencement date until 12 June 2018 using the following search terms: ((attempted suicide) OR (suicide attempt*)) AND (schizophrenia OR (schizophrenic disorder) OR (schizoaffective disorder) OR (Dementia Praecox)) AND (epidemiology OR (cross-sectional study) OR (cohort study) OR prevalence OR incidence OR rate).
Study selection
Inclusion criteria were: (a) studies of individuals with a diagnosis of schizophrenia; (b) cross-sectional or cohort studies (only the baseline data of cohort studies were analysed); (c) studies reporting prevalence of suicide attempts or providing relevant data which enabled the calculation of prevalence of suicide attempts; (d) studies published in English. Secondary analyses of medical records alone or studies with very small sample size, no timeframe or special populations (such as twins and samples in veteran/military hospitals) were excluded. Studies with mixed samples were included if data on schizophrenia and related diagnoses (e.g. schizoaffective or schizophrenia spectrum disorders) were reported separately. In order to increase homogeneity, only data of schizophrenia were extracted for analyses.
In the initial search, the titles and abstracts of publications were independently screened, and then the full texts were read by two investigators (LL and MD) to identify eligible studies. If there were multiple publications based on the identical study sample, only the one with the most complete information was analysed. Any discrepancies in study search and selection were resolved by a discussion or a consultation with a senior investigator (YTX).
Data extraction and quality assessment
Relevant data were independently extracted by the same two investigators (LL and MD), including country, study design, sample size and events of suicide attempts, mean age, gender proportion, source of patients (such as inpatients, outpatients, community or mixed), diagnostic criteria of schizophrenia, assessment tools and timeframe of suicide attempts. Study quality was also independently evaluated by the same two investigators using an eight-item instrument for quality assessment of epidemiological studies (Loney et al., 1998). The items are shown in online Supplementary Table S1. The total score ranged from 0 to 8.
Statistical analysis
The prevalence and its 95% confidence intervals (CI) of suicide attempts were calculated using a random-effects model and Freeman Tukey double arcsine transformation (Freeman and Tukey, 1950). Heterogeneity between studies was measured by τ2 and I2 statistic, with I2> 50% indicating high heterogeneity (Higgins et al., 2003).
In order to explore the sources of heterogeneity, subgroup analyses and meta-regression analyses (at least ten studies are needed) were performed. Subgroup analyses were conducted for categorical variables, such as gender (female/male); source of patients (inpatients/outpatients/community/mixed); economic group (low income/lower middle income/upper middle income and high income) and region (sub-Saharan Africa/East Asia and Pacific/South Asia/Europe and Central Asia/North America) according to the classification of the World Bank; assessment tools of suicide attempt (interview or and records/others). As recommended previously (Higgins and Green, 2011), at least ten studies are needed to perform meta-regression analyses. The potential moderating effects of continuous variables on lifetime prevalence of suicide attempts, such as sample size, mean age, the proportion of female patients, publication year and assessment score were also examined in this meta-analysis.
Funnel plots and Egger's regression model (Egger et al., 1997) were used to test publication bias. Sensitivity analysis was implemented by removing each study sequentially to assess the consistency of the primary results. Comprehensive Meta-Analysis software version 2 (Biostat Inc., Englewood, New Jersey, USA) and STATA version 12.0 (Stata Corporation, College Station, Texas, USA) were used for analyses with the significance level as a p < 0.05 (two-tailed).
Results
Search results
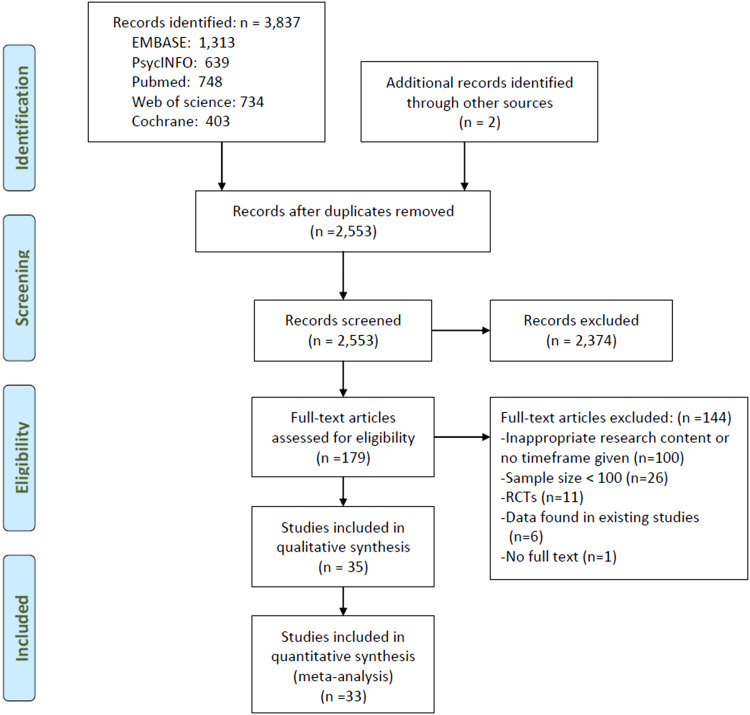
From a total of 3837 potential studies identified, 35 studies with 16 747 individuals with schizophrenia were included in the meta-analyses (Fig. 1). The full text of one study (Marcinko et al., 2008) could not be found and therefore was not included.
Fig. 1.
Flowchart of the selection of studies.
Study characteristics and quality assessment
Study characteristics are shown in Table 1. The mean age was 40.1 years and women accounted for 37.1% of the whole sample. Twenty-eight studies (11 756 patients) reported the lifetime prevalence, one study reported both the lifetime and 1-month prevalence (Radomsky et al., 1999), two studies reported the 1-year prevalence (Tang et al., 2007; Lee et al., 2012) and one study reported the 1-month prevalence of suicide attempts (Malandain et al., 2018), and two studies reported the prevalence of suicide attempts since illness onset (Prasad and Kellner, 1988; Assefa et al., 2012). One study from India (Shrivastava et al., 2016) and another from Greece (Andriopoulos et al., 2011) reported the 6-month prevalence and the prevalence of suicide attempts during the prodromal period, respectively.
Table 1.
Characteristics of the studies included in the meta-analysis
| No. | First author (year) | References | Countrya | Study design | Sample size | Age (years) M/R | Female (%) | Diagnostic criteria (SCH)b | Assessment tools (SA)c | Period experienced |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Malandain 2018 | (Malandain et al., 2018) | France | Cohort | 1859 | 38.1 | 31.4 | DSM-IV | Question | 1 month |
| 2 | Duko 2018 | (Duko and Ayano 2018) | Ethiopia | Cross-sectional | 272 | 33.7 | 30.9 | DSM-IV | CIDI | Lifetime |
| 3 | Jakhar 2017 | (Jakhar et al., 2017) | India | Cross-sectional | 270 | NR | NR | DSM-IV | DIGS and records | Lifetime |
| 4 | Shrivastava 2016 | (Shrivastava et al., 2016) | India | Cross-sectional | 200 | 36.5 | 40.5 | DSM-IV | Interview | 6 months |
| 5 | Fuller-Thomson 2016 | (Fuller-Thomson and Hollister, 2016) | Canada | Cross-sectional | 101 | NR | NR | Clinical diagnosis | Question | Lifetime |
| 6 | Fulginiti 2016 | (Fulginiti and Brekke 2016) | USA | Cohort | 166 | 33.6 | 24.1 | SADS | SADS | Lifetime |
| 7 | Togay 2015 | (Togay et al., 2015) | Turkey | Cohort | 172 | 15–45 | 40.1 | DSM-IV | Interview and records | Lifetime |
| 8 | Ran 2015 | (Ran et al., 2015) | China | Cohort | 510 | ⩾15 | 53.5 | ICD-10 | Interview | Lifetime |
| 9 | Finseth 2014 | (Finseth et al., 2014) | Norway | Cross-sectional | 338 | NR | NR | DSM-IV | Interview | Lifetime |
| 10 | Zhang 2013 | (Zhang et al., 2013) | China | Cross-sectional | 520 | 49.4 | 33.5 | DSM-IV | Interview and records | Lifetime |
| 11 | Tamminga 2013 | (Tamminga et al., 2013) | USA | Case–control | 361 | NR | NR | DSM-IV | Interview | Lifetime |
| 12 | Polsinelli 2013 | (Polsinelli et al., 2013) | Canada | Cross-sectional | 234 | 37.0 | 29.5 | DSM-IV | Interview | Lifetime |
| 13 | Ndetei 2013 | (Ndetei et al., 2013) | Kenya | Cross-sectional | 170 | 33.5 | 37.1 | DSM-IV | Interview and records | Lifetime |
| 14 | Lee 2012 | (Lee et al., 2012) | Taiwan, China | Cross-sectional | 1655 | 43.9 | 40.9 | Clinical diagnosis | Interview and records | 1 year |
| 15 | Kao 2012 | (Kao et al., 2012) | Taiwan, China | Cross-sectional | 102 | 39.5 | 51.0 | DSM-IV | Question | Lifetime |
| 16 | Assefa 2012 | (Assefa et al., 2012) | Ethiopia | Cross-sectional | 212 | 33.3 | 34.9 | DSM-IV | Question | From on-set |
| 17 | Okusaga 2011 | (Okusaga et al., 2011) | Germany | Cross-sectional | 950 | 38.0 | 36.8 | DSM-IV | Interview | Lifetime |
| 18 | Hung 2011 | (Hung et al., 2011) | Taiwan, China | Cross-sectional | 168 | 38.3 | 37.5 | DSM-IV | Interview | Lifetime |
| 19 | Andriopoulos 2011 | (Andriopoulos et al., 2011) | Greece | Case–control | 106 | 29.6 | 30.2 | DSM-IV | Interview | Prodromal phase |
| 20 | Uzun 2009 | (Uzun et al., 2009) | Turkey | Cross-sectional | 300 | 36.7 | 35.0 | DSM-IV | Interview and records | Lifetime |
| 21 | Xiang 2008 | (Xiang et al., 2008) | China | Cross-sectional | 505 | 43.0 | 51.9 | DSM-IV | Interview and records | Lifetime |
| 22 | Tang 2007 | (Tang et al., 2007) | China | Cross-sectional | 542 | 41.6 | 45.0 | DSM-IV | Interview | 1 year |
| 23 | Limosin 2007 | (Limosin et al., 2007) | France | Cohort | 3425 | 18–64 | 36.2 | ICD-10 | Interview | Lifetime |
| 24 | Tremeau 2005 | (Tremeau et al., 2005) | France | Cross-sectional | 160 | 34.2 | 27.5 | SADS | Interview | Lifetime |
| 25 | De Luca 2005 | (De Luca et al., 2005) | Canada | Cross-sectional | 253 | 41.0 | 33.0 | DSM | SCID-I | Lifetime |
| 26 | Ran 2004 | (Ran et al., 2004) | China | Cross-sectional | 145 | 32.2 | 49.0 | DSM-IV | SAIS | Lifetime |
| 27 | Niehaus 2004 | (Niehaus et al., 2004) | South Africa | Cross-sectional | 454 | NR | 27.8 | DIGS | DIGS | Lifetime |
| 28 | Kebede 2003 | (Kebede et al., 2003) | Ethiopia | Cohort | 312 | NR | 16.0 | ICD-10/DSM-IV | Interview | Lifetime |
| 29 | Chong 2000 | (Chong et al., 2000) | Singapore | Cross-sectional | 338 | 47.1 | 36.1 | DSM-IV | Interview | Lifetime |
| 30 | Radomsky 1999 | (Radomsky et al., 1999) | USA | Cross-sectional | 454 | 15–55 | 35.7 | DSM-III | Interview and records | Lifetime and 1 month |
| 31 | Harkavy-Friedman 1999 | (Harkavy-Friedman et al., 1999) | USA | Cross-sectional | 112 | NR | NR | DSM-III | DIGS | Lifetime |
| 32 | Dixon 1999 | (Dixon et al., 1999) | USA | Cross-sectional | 719 | 43.2 | 36.9 | Clinical diagnosis | Question | Lifetime |
| 33 | Prasad 1988 | (Prasad and Kellner, 1988) | UK | Cross-sectional | 417 | 38.4 | 45.8 | RDC | Interview | From on-set |
| 34 | Landmark 1987 | (Landmark et al., 1987) | UK | Cross-sectional | 118 | 38.4 | 61.0 | 12 systems | Interview | Lifetime |
| 35 | Roy 1984 | (Roy et al., 1984) | USA | Cross-sectional | 127 | NR | 42.5 | RDC and DSM | Interview | Lifetime |
M, mean; NR, not reported; R, range; SA, suicide attempt; SCH, schizophrenia.
Country: UK, United Kingdom; USA, United States.
Diagnostic criteria (SCH): DIGS, The Diagnostic Interview for Genetic Studies; DSM-III, Diagnostic and Statistical Manual of Mental Disorders, 3rd Edition; DSM-IV, Diagnostic and Statistical Manual of Mental Disorders, 4th edition; ICD-10, the 10th Revision of the International Statistical Classification of Diseases and Related Health. Problems; RDC, The Research Diagnostic Criteria; SADS, Schedule for Affective Disorders and Schizophrenia;12 systems, 12 systems for diagnosing schizophrenia.
Assessment tools (SA): CIDI, The composite international diagnostic interview; DIGS, The Diagnostic Interview for Genetic Studies; SADS, Schedule for Affective. Disorders and Schizophrenia; SAIS, Suicide Attempts Investigation Schedule; SCID-I, The Structured Interview for Psychiatric Diagnosis.
Quality assessment of all the 35 studies ranged from 4 to 7; the details of quality assessment are shown in online Supplementary Table S1.
Prevalence of suicide attempts
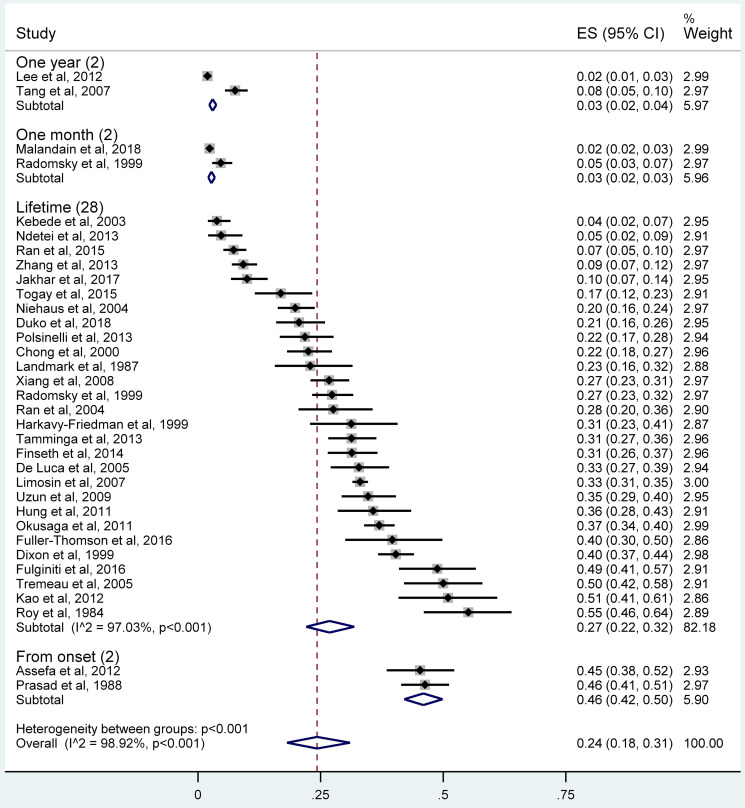
The pooled lifetime prevalence of suicide attempts was 26.8% (95% CI 22.1–31.9%; τ2 = 0.019, I2 = 97.0%, p < 0.001), while the 1-year prevalence, 1-month prevalence and the prevalence of suicide attempts from illness onset in individuals with schizophrenia were 3.0% (95% CI 2.3–3.7%; τ2 = 0.002, I2 = 95.6%), 2.7% (95% CI 2.1–3.4%; τ2 = 0.0002, I2 = 78.5%) and 45.9% (95% CI 42.1–49.9%; τ2 = 0, I2 = 0), respectively (Fig. 2). The 6-month prevalence was 38% and the prevalence during the prodromal period was 7.5%.
Fig. 2.
Forest plot of the prevalence of suicide attempts among individuals with schizophrenia.
Subgroup and meta-regression analyses
The subgroup analyses of lifetime prevalence of suicide attempts are shown in Table 2. The prevalence in high-income countries (35.3%, 95% CI 31.7–38.9%) was significantly higher than those in lower economic level countries (Q = 53.29, p < 0.001). Patients from North America (35.9%, 95% CI 29.8–42.2%) and Europe and Central Asia (32.2%, 95% CI 27.4–37.2%) were more likely to have suicide attempts than those from East Asia and Pacific (23.9%, 95% CI 14.3–35.2%), sub-Saharan Africa (11.0%, 95% CI 3.6–21.8%) and South Asia (10.0%, 95% CI 6.7–14.2%; Q = 32.83, p < 0.001). Early onset of illness group (41.8%, 95% CI 30.7–53.5%) had more frequent suicide attempts than late-onset patients (23.6%, 95% CI 12.1–37.6%; Q = 4.38, p = 0.04).
Table 2.
Subgroup analyses of the lifetime prevalence of suicide attempts in individuals with schizophrenia
| Subgroups | Categories (number of studies) | Prevalence (%) | 95% CI (%) | Events | Sample size | τ2 (P) | I2 (%, P) | Q (p value between subgroups) | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Gender | Female (15) | 28.2 | 21.0 | 36.1 | 928 | 3049 | 0.48 (0.489) | 94.4 | <0.001 | 1.03 (0.31) |
| Male (15) | 24.6 | 17.7 | 32.2 | 1400 | 5324 | 96.9 | <0.001 | |||
| Mean age (years) | Age ⩽ 38.15 (8) | 29.3 | 20.0 | 39.5 | 771 | 2397 | 0 (0.985) | 96.1 | <0.001 | 0.001 (0.97) |
| Age > 38.15 (8) | 29.1 | 19.9 | 39.4 | 771 | 2723 | 96.7 | <0.001 | |||
| Source of patients | Inpatients (7) | 25.9 | 14.2 | 39.6 | 446 | 1914 | 97.5 | <0.001 | 1.85 (0.60) | |
| Outpatients (3) | 27.3 | 10.5 | 48.4 | 214 | 877 | 97.5 | <0.001 | |||
| Community (4) | 21.2 | 4.6 | 45.4 | 170 | 1089 | 98.5 | <0.001 | |||
| Mixed (4) | 31.0 | 24.1 | 38.3 | 1618 | 4936 | 94.8 | <0.001 | |||
| Duration of illness (years) | ⩽15.8 (5) | 33.7 | 26.4 | 41.4 | 627 | 1795 | 0.99 (0.804) | 89.5 | <0.001 | 0.69 (0.41) |
| >15.8 (4) | 27.8 | 12.5 | 46.5 | 236 | 1128 | 97.4 | <0.001 | |||
| Age of onset (years) | ⩽24.38 (4) | 41.8 | 30.7 | 53.5 | 318 | 843 | 4.03 (0.045) | 90.6 | <0.001 | 4.38 (0.04) |
| >24.38 (4) | 23.6 | 12.1 | 37.6 | 327 | 1470 | 97.0 | <0.001 | |||
| Assessment tools (SA)a | Interview or and records (21) | 27.0 | 21.4 | 33.0 | 2945 | 10 084 | 0.015 (0.904) | 97.5 | <0.001 | 0.002 (0.97) |
| Others (7) | 26.3 | 17.8 | 35.8 | 412 | 1672 | 94.2 | <0.001 | |||
| Economic group | Low income (2) | 10.2 | 7.9 | 12.8 | 68 | 584 | 177.96 (<0.001) | – | – | 53.29 (<0.001) |
| Lower middle incomea (2) | 7.7 | 5.4 | 10.5 | 35 | 440 | – | – | |||
| Upper middle incomea (7) | 19.3 | 11.9 | 28.0 | 483 | 2606 | 96.4 | <0.001 | |||
| High incomea (17) | 35.3 | 31.7 | 38.9 | 2771 | 8126 | 89.0 | <0.001 | |||
| Region | Sub-Saharan Africa (4) | 11.0 | 3.6 | 21.8 | 166 | 1208 | 71.47 (<0.001) | 96.1 | <0.001 | 32.83 (<0.001) |
| East Asia and Pacific (7) | 23.9 | 14.3 | 35.2 | 448 | 2288 | 97.1 | <0.001 | |||
| South Asia (1) | 10.0 | 6.7 | 14.2 | 27 | 270 | – | – | |||
| Europe and Central Asia (7) | 32.2 | 27.4 | 37.2 | 1829 | 5463 | 89.3 | <0.001 | |||
| North America (8) | 35.9 | 29.8 | 42.2 | 887 | 2527 | 90.0 | <0.001 | |||
| Total (28) | 26.8 | 22.1 | 31.9 | 3357 | 11 756 | 0.019 | 97.0 | <0.001 | − | |
SA, suicide attempt. Bolded values: p < 0.05.
Meta-regression analyses revealed that sample size (slope = 0.0001, p = 0.91), mean age (slope = −0.006, p = 0.42), the percentage of women (slope = 0.0008, p = 0.81), publication year (slope = −0.004, p = 0.187) and assessment score (slope = 0.04, p = 0.07) did not statistically moderate the lifetime prevalence of suicide attempts.
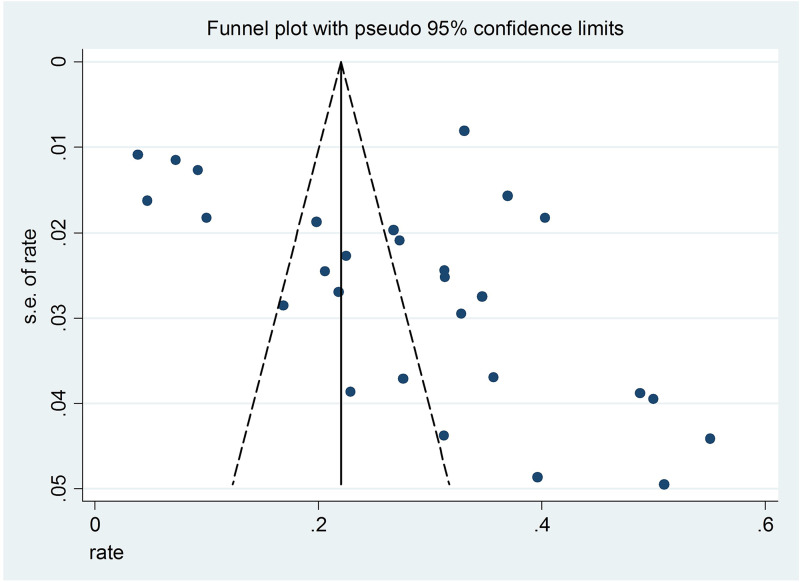
Sensitivity analysis and publication bias
Sensitivity analyses found that after removing each study sequentially, the results of the lifetime prevalence did not change significantly. The funnel plot showed slight asymmetry, but the Egger's tests (t = 1.89, 95% CI −0.45 to 10.92, p = 0.07) did not reveal any publication bias (Fig. 3).
Fig. 3.
Funnel plot of the 28 included studies reporting the lifetime prevalence of suicide attempts.
Discussion
This was the first meta-analysis that examined the prevalence of suicide attempts in individuals with schizophrenia across studies worldwide. This meta-analysis found that the lifetime prevalence of suicide attempts was 26.8% (95% CI 22.1–31.9%), which is approximately two times higher compared to the corresponding figure (14.6%, 95% CI 9.1–22.8%) in China (Dong et al., 2017). In addition, the prevalence in individuals with schizophrenia is much higher than the corresponding figure in general populations among 17 countries (2.7%) (Nock et al., 2008) and in China alone (0.8%, 95% CI 0.7–0.9%) (Cao et al., 2015). Apart from the confounding effects of study characteristics, clinical factors, such as severity of psychiatric symptoms, comorbid disorders and the stigma and discrimination related to the illness, could contribute to the higher risk of suicide attempts in individuals with schizophrenia (Hor and Taylor, 2010; Fuller-Thomson and Hollister, 2016; Duko and Ayano, 2018).
The pooled prevalence of suicide attempts from illness onset (45.9%) was highest, followed by the 6-month prevalence (38%) and the lifetime prevalence (26.8%). Prevalence estimates are significantly influenced by the illness severity and duration of the study. As in the case of this meta-analysis, only one study reported the 6-month prevalence of suicide attempt and two studies reported from-onset prevalence. This may bias the validity of the pooled prevalence of suicide attempts across studies with different timeframes and sampling. Other than the confounding effects caused by potential recall bias and small number of studies, various factors such as more severe psychotic symptoms, impaired global functioning from onset and stigma could increase the risk of suicidal behaviours in individuals with schizophrenia (Kaplan and Harrow, 1996; Radomsky et al., 1999; Assefa et al., 2012; Jakhar et al., 2017). Patients with a younger age of illness onset had a higher risk of suicide attempts, which is consistent with some (Panariello et al., 2010; Vinokur et al., 2014; Niehaus et al., 2004), but not all studies (Popovic et al., 2014). In contrast, individuals with schizophrenia with late-onset illness may have relatively better developed social skills and functioning, and less violent or impulsive tendency, all of which could reduce the risk of suicidality (Patterson et al., 1989; Vinokur et al., 2014).
Individuals with schizophrenia in high-income countries were more likely to attempt suicide than those in the low- or/and middle-incomes countries, while those in North America or Europe and Central Asia had a higher prevalence of suicide attempts than in South Asia, sub-Saharan Africa, East Asia and Pacific areas. The varying prevalence of suicide attempts across different regions could be partly explained by the differences in sociocultural and economic contexts and health care policies. For example, accessible mental health services and resources could effectively lower the risk of suicidal behaviours (Cooper et al., 2006), while societal discrimination of individuals with schizophrenia could lead to internalised stigma and increase the risk of suicide attempt (Assefa et al., 2012). In addition, religious and cultural factors are associated with the prevalence of substance abuse, such as alcohol and cocaine (Karch et al., 2006), which could in turn increase the risk of suicide attempt (Prince, 2018). Further, very few studies on suicide in schizophrenia have been conducted in low- and middle-income countries, which could lead to biased results. Of the included studies reporting lifetime prevalence, only two were conducted in low-income countries, two in lower middle income countries, one in South Asia and four in sub-Saharan Africa, which could reduce the reliability of the results. Apart from two studies in Turkey (upper middle-income country) (Uzun et al., 2009; Togay et al., 2015), studies in other countries were in the North America, Europe and Central Asia groups representing high-income countries. The relatively well-established reporting system for suicidal behaviours in these countries may be another reason for the higher prevalence of suicide attempts.
Gender difference in the prevalence of suicide attempts in individuals with schizophrenia has been controversial. For example, in some studies, females had more frequent suicide attempts (Tang et al., 2007; Fuller-Thomson and Hollister, 2016), while the opposite was found in other studies (Ran et al., 2015; Shrivastava et al., 2016). We did not find any gender difference, which is consistent with some (Dong et al., 2017), but not all studies (Hawton, 2000). Unlike the findings in previous studies (Hor and Taylor, 2010; Zhang et al., 2013), we did not find any association between younger age and risk of suicide attempts. Different illness phases and settings (e.g. inpatients v. outpatient settings) are associated with different risk of suicide for individuals with schizophrenia (Drake et al., 1985). However, subgroup analysis did not find any difference in suicide attempt prevalence between inpatients, outpatients and those in community.
Several methodological limitations need to be addressed. First, only studies published in English were included. Second, subgroup and meta-regression analyses were only performed for lifetime prevalence of suicide attempts due to a low number of studies of other timeframes. Third, some factors related to suicide attempts, such as prescription of antipsychotic medications, psychiatric comorbidities and number of admissions (Fuller-Thomson and Hollister, 2016), were not examined due to lack of data in the included studies. Fourth, similar to other meta-analyses (Winsper et al., 2013; Long et al., 2014; Li et al., 2016; Mata et al., 2015), high heterogeneity remained in the subgroup analyses, which is difficult to avoid in a meta-analysis of observational surveys. The heterogeneity was probably related to certain unmeasured factors, such as severity of psychotic symptoms, family history of psychiatric disorders and suicide, use of psychotropic medications and access to health services. In addition, only individuals with schizophrenia were included in this study, therefore the findings cannot be generalised to those with schizoaffective or schizophrenia spectrum disorders. Finally, only one study reported the 6-month prevalence of suicide attempt, two studies reported the 1-year prevalence, two studies reported the 1-month prevalence and two studies reported from-onset prevalence. Hence, the small number of studies in these timeframes may bias the validity of the pooled prevalence of suicide attempts.
In conclusion, suicide attempts are common in individuals with schizophrenia, especially those with an early age of onset and living in high-income countries and regions. Careful screening and effective preventive measures should be implemented routinely for this population.
Acknowledgements
None.
Availability of data and materials
All the data involved have been included in Tables and Figures of this manuscript.
Author ORCIDs
Yu-Tao Xiang, 0000-0002-2906-0029.
Financial Support
The study was supported by the University of Macau (MYRG2015-00230-FHS; MYRG2016-00005-FHS), National Key Research & Development Program of China (No. 2016YFC1307200), Beijing Municipal Administration of Hospitals Clinical Medicine Development of Special Funding Support (No.ZYLX201607) and Beijing Municipal Administration of Hospitals' Ascent Plan (No. DFL20151801).
Ethical standards
Not applicable.
Supplementary material
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S2045796019000313.
click here to view supplementary material
Conflict of interest
None.
References
- Andriopoulos I, Ellul J, Skokou M and Beratis S (2011) Suicidality in the ‘prodromal’ phase of schizophrenia. Comprehensive Psychiatry 52, 479–485. [DOI] [PubMed] [Google Scholar]
- Assefa D, Shibre T, Asher L and Fekadu A (2012) Internalized stigma among patients with schizophrenia in Ethiopia: a cross-sectional facility-based study. BMC Psychiatry 12, 239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bhugra D (2005) The global prevalence of schizophrenia. PLoS Medicine 2, e151, quiz e175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown S (1997) Excess mortality of schizophrenia. A meta-analysis. British Journal of Psychiatry 171, 502–508. [DOI] [PubMed] [Google Scholar]
- Caldwell CB and Gottesman II (1992) Schizophrenia – a high-risk factor for suicide: clues to risk reduction. Suicide and Life-Threatening Behavior 22, 479–493. [PubMed] [Google Scholar]
- Cao XL, Zhong BL, Xiang YT, Ungvari GS, Lai KY, Chiu HF and Caine ED (2015) Prevalence of suicidal ideation and suicide attempts in the general population of China: a meta-analysis. International Journal of Psychiatry in Medicine 49, 296–308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chong SA, Lee WL, Tan CH, Tay AH, Chan AO and Tan EC (2000) Attempted suicide and polymorphism of the serotonin transporter gene in Chinese patients with schizophrenia. Psychiatry Research 97, 101–106. [DOI] [PubMed] [Google Scholar]
- Cooper SL, Lezotte D, Jacobellis J and Diguiseppi C (2006) Does availability of mental health resources prevent recurrent suicidal behavior? An ecological analysis. Suicide and Life-Threatening Behavior 36, 409–417. [DOI] [PubMed] [Google Scholar]
- De Luca V, Voineskos D, Wong GW, Shinkai T, Rothe C, Strauss J and Kennedy JL (2005) Promoter polymorphism of second tryptophan hydroxylase isoform (TPH2) in schizophrenia and suicidality. Psychiatry Research 134, 195–198. [DOI] [PubMed] [Google Scholar]
- Dixon L, Postrado L, Delahanty J, Fischer PJ and Lehman A (1999) The association of medical comorbidity in schizophrenia with poor physical and mental health. The Journal of Nervous and Mental Disease 187, 496–502. [DOI] [PubMed] [Google Scholar]
- Dong M, Wang SB, Wang F, Zhang L, Ungvari GS, Ng CH, Meng X, Yuan Z, Wang G and Xiang YT (2017) Suicide-related behaviours in schizophrenia in China: a comprehensive meta-analysis. Epidemiology and Psychiatric Sciences 28, 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drake RE, Gates C, Whitaker A and Cotton PG (1985) Suicide among schizophrenics: a review. Comprehensive Psychiatry 26, 90–100. [DOI] [PubMed] [Google Scholar]
- Duko B and Ayano G (2018) Suicidal ideation and attempts among people with severe mental disorder, Addis Ababa, Ethiopia, comparative cross-sectional study. Annals of General Psychiatry 17, 23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Egger M, Davey Smith G, Schneider M and Minder C (1997) Bias in meta-analysis detected by a simple, graphical test. BMJ 315, 629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finseth PI, Sonderby IE, Djurovic S, Agartz I, Malt UF, Melle I, Morken G, Andreassen OA, Vaaler AE and Tesli M (2014) Association analysis between suicidal behaviour and candidate genes of bipolar disorder and schizophrenia. Journal of Affective Disorders 163, 110–114. [DOI] [PubMed] [Google Scholar]
- Freeman MF and Tukey JW (1950) Transformations related to the angular and the square root. The Annals of Mathematical Statistics 21, 607–611. [Google Scholar]
- Fulginiti A and Brekke JS (2016) Suicide attempt status and quality of life disparity among individuals with schizophrenia: a longitudinal analysis. Journal of the Society for Social Work and Research 7, 269–288. [Google Scholar]
- Fuller-Thomson E and Hollister B (2016) Schizophrenia and suicide attempts: findings from a representative community-based Canadian sample. Schizophrenia Research and Treatment 2016, 3165243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harkavy-Friedman JM, Restifo K, Malaspina D, Kaufmann CA, Amador XF, Yale SA and Gorman JM (1999) Suicidal behavior in schizophrenia: characteristics of individuals who had and had not attempted suicide. American Journal of Psychiatry 156, 1276–1278. [DOI] [PubMed] [Google Scholar]
- Hawton K (2000) Sex and suicide. Gender differences in suicidal behaviour. The British Journal of Psychiatry 177, 484–485. [DOI] [PubMed] [Google Scholar]
- Higgins JP and Green S (2011) Cochrane Handbook for Systematic Reviews of Interventions. The Cochrane Collaboration, Uk: John Wiley & Sons. [Google Scholar]
- Higgins JP, Thompson SG, Deeks JJ and Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327, 557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hor K and Taylor M (2010) Suicide and schizophrenia: a systematic review of rates and risk factors. Journal of Psychopharmacology 24, 81–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hung CF, Lung FW, Chen CH, O'Nions E, Hung TH, Chong MY, Wu CK, Wen JK and Lin PY (2011) Association between suicide attempt and a tri-allelic functional polymorphism in serotonin transporter gene promoter in Chinese patients with schizophrenia. Neuroscience Letters 504, 242–246. [DOI] [PubMed] [Google Scholar]
- Jakhar K, Beniwal RP, Bhatia T and Deshpande SN (2017) Self-harm and suicide attempts in Schizophrenia. Asian Journal of Psychiatry 30, 102–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kao YC, Liu YP, Cheng TH and Chou MK (2012) Subjective quality of life and suicidal behavior among Taiwanese schizophrenia patients. Social Psychiatry and Psychiatric Epidemiology 47, 523–532. [DOI] [PubMed] [Google Scholar]
- Kaplan KJ and Harrow M (1996) Positive and negative symptoms as risk factors for later suicidal activity in schizophrenics versus depressives. Suicide and Life-Threatening Behavior 26, 105–121. [PubMed] [Google Scholar]
- Karch DL, Barker L and Strine TW (2006) Race/ethnicity, substance abuse, and mental illness among suicide victims in 13 US states: 2004 data from the National Violent Death Reporting System. Injury Prevention 12(suppl. 2), ii22–ii27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kebede D, Alem A, Shibre T, Negash A, Fekadu A, Fekadu D, Deyassa N, Jacobsson L and Kullgren G (2003) Onset and clinical course of schizophrenia in Butajira-Ethiopia – a community-based study. Social Psychiatry and Psychiatric Epidemiology 8, 625–631. [DOI] [PubMed] [Google Scholar]
- Landmark J, Cernovsky ZZ and Merskey H (1987) Correlates of suicide attempts and ideation in schizophrenia. The British Journal of Psychiatry 151, 18–20. [DOI] [PubMed] [Google Scholar]
- Laursen TM (2011) Life expectancy among persons with schizophrenia or bipolar affective disorder. Schizophrenia Research 131, 101–104. [DOI] [PubMed] [Google Scholar]
- Lee JL, Ma WF, Yen WJ, Huang XY and Chiang LC (2012) Predicting the likelihood of suicide attempts for rural outpatients with schizophrenia. Journal of Clinical Nursing 21, 2896–2904. [DOI] [PubMed] [Google Scholar]
- Li Y, Cao XL, Zhong BL, Ungvari GS, Chiu HF, Lai KY, Zheng W, Correll CU and Xiang YT (2016) Smoking in male patients with schizophrenia in China: a meta-analysis. Drug and Alcohol Dependence 162, 146–153. [DOI] [PubMed] [Google Scholar]
- Limosin F, Loze JY, Philippe A, Casadebaig F and Rouillon F (2007) Ten-year prospective follow-up study of the mortality by suicide in schizophrenic patients. Schizophrenia Research 94, 23–28. [DOI] [PubMed] [Google Scholar]
- Loney PL, Chambers LW, Bennett KJ, Roberts JG and Stratford PW (1998) Critical appraisal of the health research literature: prevalence or incidence of a health problem. Chronic Disease in Canada 19, 170–176. [PubMed] [Google Scholar]
- Long J, Huang G, Liang W, Liang B, Chen Q, Xie J, Jiang J and Su L (2014) The prevalence of schizophrenia in mainland China: evidence from epidemiological surveys. Acta Psychiatrica Scandinavica 130, 244–256. [DOI] [PubMed] [Google Scholar]
- Malandain L, Thibaut F, Grimaldi-Bensouda L, Falissard B, Abenhaim L and Nordon C (2018) Correlates and predictors of antipsychotic drug polypharmacy in real-life settings: results from a nationwide cohort study. Schizophrenia Research 192, 213–218. [DOI] [PubMed] [Google Scholar]
- Marcinko D, Popovic-Knapic V, Franic T, Karlovic D, Martinac M, Brataljenovic T and Jakovljevic M (2008) Association of cholesterol and socio-demographic parameters with suicidality in the male patients with schizophrenia. Psychiatria Danubina 20, 390–395. [PubMed] [Google Scholar]
- Mata DA, Ramos MA, Bansal N, Khan R, Guille C, Di Angelantonio E and Sen S (2015) Prevalence of depression and depressive symptoms among resident physicians: a systematic review and meta-analysis. JAMA 314, 2373–2383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ndetei DM, Khasakhala L, Meneghini L and Aillon JL (2013) The relationship between schizo-affective, schizophrenic and mood disorders in patients admitted at Mathari Psychiatric Hospital, Nairobi, Kenya. African Journal of Psychiatry (Johannesbg) 16, 110–117. [DOI] [PubMed] [Google Scholar]
- Niehaus DJ, Laurent C, Jordaan E, Koen L, Oosthuizen P, Keyter N, Muller JE, Mbanga NI, Deleuze JF, Mallet J, Stein DJ and Emsley R (2004) Suicide attempts in an African schizophrenia population: an assessment of demographic risk factors. Suicide and Life-Threatening Behavior 34, 320–327. [DOI] [PubMed] [Google Scholar]
- Nock MK, Borges G, Bromet EJ, Alonso J, Angermeyer M, Beautrais A, Bruffaerts R, Chiu WT, de Girolamo G, Gluzman S, de Graaf R, Gureje O, Haro JM, Huang Y, Karam E, Kessler RC, Lepine JP, Levinson D, Medina-Mora ME, Ono Y, Posada-Villa J and Williams D (2008) Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. British Journal of Psychiatry 192, 98–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okusaga O, Langenberg P, Sleemi A, Vaswani D, Giegling I, Hartmann AM, Konte B, Friedl M, Groer MW, Yolken RH, Rujescu D and Postolache TT (2011) Toxoplasma gondii antibody titers and history of suicide attempts in patients with schizophrenia. Schizophrenia Research 133, 150–155. [DOI] [PubMed] [Google Scholar]
- Olfson M, Gerhard T, Huang C, Crystal S and Stroup TS (2015) Premature mortality among adults with schizophrenia in the United States. JAMA Psychiatry 72, 1172–1181. [DOI] [PubMed] [Google Scholar]
- Palmer BA, Pankratz VS and Bostwick JM (2005) The lifetime risk of suicide in schizophrenia: a reexamination. Archives of General Psychiatry 62, 247–253. [DOI] [PubMed] [Google Scholar]
- Panariello F, O'Driscoll L, de Souza RP, Tiwari A, Manchia M, Kennedy J and De Luca V (2010) Age at onset in Canadian schizophrenia patients: admixture analysis. Schizophrenia Research 122, 278–279. [DOI] [PubMed] [Google Scholar]
- Patterson GR, DeBaryshe BD and Ramsey E (1989) A developmental perspective on antisocial behavior. American Psychologist 44, 329–335. [DOI] [PubMed] [Google Scholar]
- Polsinelli G, Zai CC, Strauss J, Kennedy JL and De Luca V (2013) Association and CpG SNP analysis of HTR4 polymorphisms with suicidal behavior in subjects with schizophrenia. Journal of Neural Transmission (Vienna) 120, 253–258. [DOI] [PubMed] [Google Scholar]
- Popovic D, Benabarre A, Crespo JM, Goikolea JM, Gonzalez-Pinto A, Gutierrez-Rojas L, Montes JM and Vieta E (2014) Risk factors for suicide in schizophrenia: systematic review and clinical recommendations. Acta Psychiatrica Scandinavica 130, 418–426. [DOI] [PubMed] [Google Scholar]
- Prasad AJ and Kellner P (1988) Suicidal behaviour in schizophrenic day patients. Acta Psychiatrica Scandinavica 77, 488–490. [DOI] [PubMed] [Google Scholar]
- Prince J (2018) Substance use disorder and suicide attempt among people who report compromised health. Substance Use & Misuse 53, 9–15. [DOI] [PubMed] [Google Scholar]
- Radomsky ED, Haas GL, Mann JJ and Sweeney JA (1999) Suicidal behavior in patients with schizophrenia and other psychotic disorders. American Journal of Psychiatry 156, 1590–1595. [DOI] [PubMed] [Google Scholar]
- Ran MS, Wu QH, Conwell Y, Chen EY and Chan CL (2004) Suicidal behavior among inpatients with schizophrenia and mood disorders in Chengdu, China. Suicide and Life-Threatening Behavior 34, 311–319. [DOI] [PubMed] [Google Scholar]
- Ran MS, Mao WJ, Chan CLW, Chen EYH and Conwell Y (2015) Gender differences in outcomes in people with schizophrenia in rural China: 14-year follow-up study. The British Journal of Psychiatry 206, 283–288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy A (1983) Family history of suicide. Archives of General Psychiatry 40, 971–974. [DOI] [PubMed] [Google Scholar]
- Roy A, Mazonson A and Pickar D (1984) Attempted suicide in chronic schizophrenia. The British Journal of Psychiatry 144, 303–306. [DOI] [PubMed] [Google Scholar]
- Shrivastava AK, De Sousa AA, Karia SB and Shah NB (2016) Study of suicidality and suicide behavior among individuals with long-standing duration of schizophrenia in India: an explorative study. Asean Journal of Psychiatry 17, 179–187. [Google Scholar]
- Tamminga CA, Ivleva EI, Keshavan MS, Pearlson GD, Clementz BA, Witte B, Morris DW, Bishop J, Thaker GK and Sweeney JA (2013) Clinical phenotypes of psychosis in the Bipolar-Schizophrenia Network on Intermediate Phenotypes (B-SNIP). American Journal of Psychiatry 170, 1263–1274. [DOI] [PubMed] [Google Scholar]
- Tang YL, Gillespie CF, Epstein MP, Mao PX, Jiang F, Chen Q, Cai ZJ and Mitchell PB (2007) Gender differences in 542 Chinese inpatients with schizophrenia. Schizophrenia Research 97, 88–96. [DOI] [PubMed] [Google Scholar]
- Togay B, Noyan H, Tasdelen R and Ucok A (2015) Clinical variables associated with suicide attempts in schizophrenia before and after the first episode. Psychiatry Research 229, 252–256. [DOI] [PubMed] [Google Scholar]
- Tremeau F, Staner L, Duval F, Correa H, Crocq MA, Darreye A, Czobor P, Dessoubrais C and Macher JP (2005) Suicide attempts and family history of suicide in three psychiatric populations. Suicide and Life-Threatening Behavior 35, 702–713. [DOI] [PubMed] [Google Scholar]
- Uzun O, Tamam L, Ozculer T, Doruk A and Unal M (2009) Specific characteristics of suicide attempts in patients with schizophrenia in Turkey. The Israel Journal of Psychiatry and Related Sciences 46, 189–194. [PubMed] [Google Scholar]
- Vinokur D, Levine SZ, Roe D, Krivoy A and Fischel T (2014) Age of onset group characteristics in forensic patients with schizophrenia. European Psychiatry 29, 149–152. [DOI] [PubMed] [Google Scholar]
- Whiteford HA, Degenhardt L, Rehm J, Baxter AJ, Ferrari AJ, Erskine HE, Charlson FJ, Norman RE, Flaxman AD, Johns N, Burstein R, Murray CJ and Vos T (2013) Global burden of disease attributable to mental and substance use disorders: findings from the Global Burden of Disease Study 2010. Lancet 382, 1575–1586. [DOI] [PubMed] [Google Scholar]
- Winsper C, Ganapathy R, Marwaha S, Large M, Birchwood M and Singh SP (2013) A systematic review and meta-regression analysis of aggression during the first episode of psychosis. Acta Psychiatrica Scandinavica 128, 413–421. [DOI] [PubMed] [Google Scholar]
- Xiang YT, Weng YZ, Leung CM, Tang WK and Ungvari GS (2008) Socio-demographic and clinical correlates of lifetime suicide attempts and their impact on quality of life in Chinese schizophrenia patients. Journal of Psychiatric Research 42, 495–502. [DOI] [PubMed] [Google Scholar]
- Zhang XY, Al Jurdi RK, Zoghbi AW, Chen DC, Xiu MH, Tan YL, Yang FD and Kosten TR (2013) Prevalence, demographic and clinical correlates of suicide attempts in Chinese medicated chronic inpatients with schizophrenia. Journal of Psychiatric Research 47, 1370–1375. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
For supplementary material accompanying this paper visit http://dx.doi.org/10.1017/S2045796019000313.
click here to view supplementary material
Data Availability Statement
All the data involved have been included in Tables and Figures of this manuscript.