Abstract
The purpose of this study was to define risk factors for non-compression radiculitis following anterior lumbar surgery with or without posterior instrumentation and to define a time to resolution. In this study, we followed 58 consecutive patients who had anterior lumbar surgery with or without posterior instrumentation. We identified those with and without post-operative radiculitis. There as a 36.5% rate of postoperative radiculitis. We found that there was a moderate to strong correlation with height change and radiculitis (p = 0.044). Additionally patients treated with rh-BMP2 had a higher risk of developing symptoms. In all of the patients who developed postoperative radiculitis, symptoms resolved by 3 months. In conclusion 36.5% of patients developed post operative radiculitis. This was associated with the use of rh-BMP2, as well as increasing disc height through surgery. All symptoms resolved by 3 months posoperatively.
1. Introduction
Anterior lumbar interbody fusion (ALIF) was introduced by Hodgson and Stock in 1956 for the treatment of selected tuberculosis cases.1 Since that time, the indications for ALIF has expanded to include treatment for spondylolisthesis, degenerative disc disease with or without radiculopathy, degenerative scoliosis, pseudarthrosis from a failed previous fusion, trauma, post laminectomy instability, and tumor surgery.2
Surgeons performing anterior lumbar surgery should be versed in the complication profile to properly counsel prospective patients and appropriately manage them should they arise. The known complications for anterior lumbar procedures include those that occur due to the exposure and those due to the discectomy and fusion itself. The approach related complications include development of a hernia, bowel injury, vascular injury (aorta and iliac vessels), retrograde ejaculation, deep vein thrombosis, and ureteral damage.3 The genitofemoral nerve may also be injured as it courses anterior to the psoas. The complications related to the decompression and fusion include: nerve root injury, durotomy, epidural hematoma, adjacent level disease and pseudarthrosis. Complications at the harvest site may also occur if bone graft is harvested for the fusion.3,4 Reports of radiculitis following ALIF procedures range from 8.3% to 24%.5,6 Lee et al. reported on a series of 41 patients with a rate of radiculitis being 24%.5 The authors attributed this high rate of radiculitis to inflammation caused by the use of recombinant human bone morphogenic protein 2 (rhBMP-2). Likewise, Hirabalek et al. found a rate of 8.3%, but did not postulate a cause.6 Neither of these authors listed a time to resolution of the symptoms.
The purpose of this retrospective case series was to further define the incidence of transient radiculitis. Additionally, we sought to investigate the theory that these symptoms are related to a stretch phenomenon on the nerve root secondary to acute change in disc height.
2. Materials and methods
In this study we hypothesized that a larger change in disc height would be associated with postoperative radiculitis.
After obtaining approval from the institutional review board, a retrospective review was conducted of all ALIF and total disc replacement (TDR) procedures performed between January 2012 and December 2017, by one of two fellowship-trained orthopaedic spine surgeons. Patients were included if they were 18 years or older, undergoing primary, isolated ALIF or TDR, without deficiency of the posterior elements, and had preoperative and postoperative imaging available for review. Multilevel procedures were included. Patients were included if they had minimally invasive posterior instrumentation performed at the index procedure. Patients were excluded if they were younger than 18 years of age, underwent combined anterior surgery with a posterior decompression, underwent the procedure to address malignancy or infection, were pregnant, or lacked imaging available for review.
After identifying patients for inclusion, the Armed Forces Health Longitudinal Technology Application (AHLTA) electronic medical record was reviewed to record demographic information. Operative reports were reviewed to identify surgical variables, including surgery performed, preoperative diagnosis, levels operated on, type of implants (ALIF vs TDR), and graft type used. Additionally, postoperative data was reviewed to identify patients who developed postoperative radiculitis and time to resolution if present. For the purposes of this study, postoperative radiculitis was defined as the presence of postoperative radicular pain that did not exist prior to surgery and was not attributable to compressive pathology after imaging.
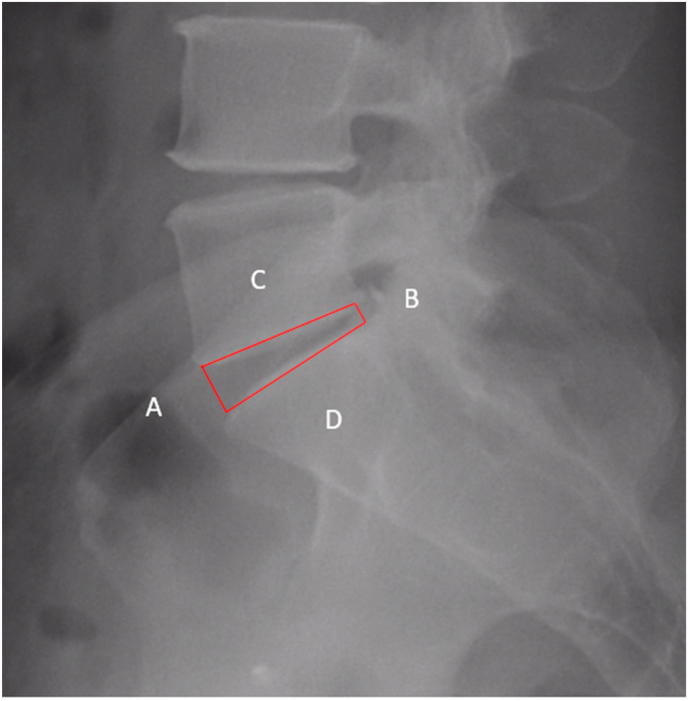
Preoperative imaging studies were reviewed to assess preoperative disc height and were compared against intraoperative fluoroscopic imaging studies. The Farfan ratio is a validated ratio that uses internal measurements to standardize a ratio to assess disc height.7 The ratio is calculated as (anterior disc height-posterior disc height)/((superior endplate length/inferior endplate length)/2) (Fig. 1).The Farfan ratio was calculated preoperatively and after placement of the implant.
Fig. 1.
Zoomed in view of a preoperative L-Spot radiograph of a patient that had postoperative neurapraxia. Line A designates the anterior disc height. Line B designates the posterior disc height. Line C is the superior disc length. Line D is the inferior disc length. Thus, the farfan ratio would be calculated as (A–B)/((C/D)/2).
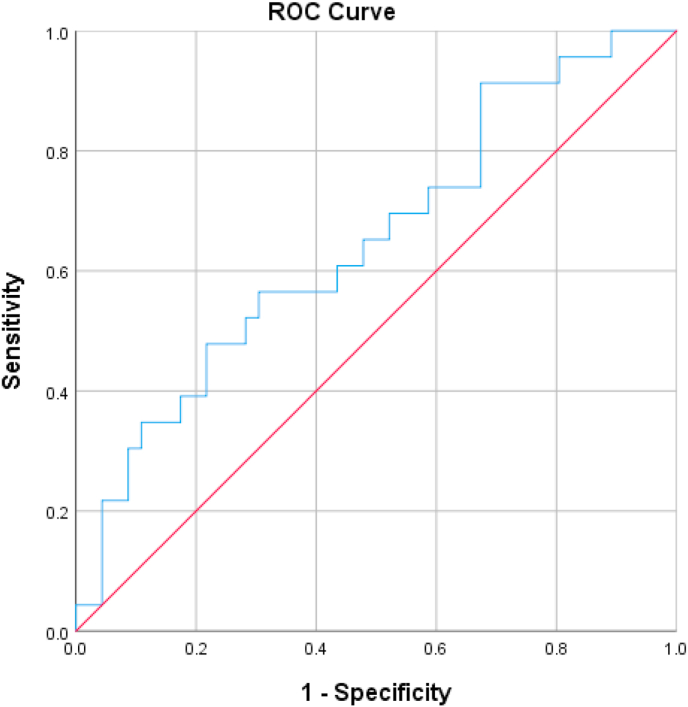
Data analysis was performed using SPSS statistical package version 24 (SPSS Inc, Chicago, IL) and Microsoft Excel (Microsoft Corp, Redmond, WA). Statistical significance was set at p < 0.05. Descriptive statistics were generated to define the incidence of postoperative radiculitis. Pearson's correlation coefficients were used to assess for correlation between disc height and change in height with the development of postoperative radiculitis. A receiver operating characteristic curve (ROC) analysis was used to identify a threshold for disc height change for the development radiculitis. Chi Squared tests were used to analyze the differences between patients developing postoperative symptoms between one and two level surgery and Hybrid (TDR and ALIF) versus two level ALIF.
3. Results
A total of 70 patients were identified for study inclusion. Of those, 12 were excluded (exclusions included 5 for combined posterior decompression surgery, 2 lacking preoperative imaging, 1 revision surgery, 1 with preoperative neuritis, 1 postoperative complication which entailed a small bowel obstruction requiring resection, 1 intraoperative vascular injury, and 1 listhesis of the implant with L5 on S1), leaving 58 patients (average 42.5 years, range 30–63 years, 37.9% female) for study inclusion. Patient demographic information is summarized in Table 1.
Table 1.
Demographic data, diagnoses and procedures.
| PatientPatient | AAaaaAge | Sexsexsex | DiagD Diagnosis | Dia Procedure(s) |
|---|---|---|---|---|
| 1 | 61 | f | L5-S1 Post-laminectomy syndrome | L5-S1 ALIF |
| 2 | 37 | m | L4-L5 and L5-S1 DDD, L5-S1 DDD | L4-L5 TDR, L5-S1 TDR |
| 3 | 30 | f | L5-S1 pseudoarthrosis | L5-S1 ALIF |
| 4 | 43 | m | L5-S1 DDD | L5-S1 ALIF |
| 5 | 36 | f | L4-L5 DDD, L5-S1 DDD | L4-L5 TDR, L5-S1 ALIF |
| 6 | 50 | m | L5-S1 facet arthropathy and DDD | L5-S1 ALIF |
| 7 | 38 | m | L5-S1 DDD with S1 radiculopathy | L5-S1 ALIF |
| 8 | 33 | f | L5-S1 DDD | L5-S1 TDR |
| 9 | 43 | m | L4-L5 DDD, L5-S1 DDD | L4-L5 ALIF, L5-S1 TDR |
| 10 | 35 | m | L5-S1 DDD | L5-S1 TDR |
| 11 | 46 | m | L5-S1 Spondylolisthesis | L5-S1 AlIF |
| 12 | 55 | f | L5-S1 spondylolisthesis | l5-S1 ALIF |
| 13 | 52 | f | L5-S1 DDD | L5-S1 ALIF |
| 14 | 56 | f | L4-L5 Spondylolisthesis | L4-L5 ALIF |
| 15 | 41 | m | L5-S1 Spondylolisthesis | L5-S1 ALIF |
| 16 | 38 | m | L4-L5 DDD, L5-S1 DDD | L4-L5 ALIF, L5-S1 TDR |
| 17 | 38 | m | L4-L5 DDD, L5-S1 DDD | L4-L5 ALIF, L5-S1 TDR |
| 18 | 46 | m | L4-L5 DDD, L5-S1 Spondylolisthesis | L4-L5 ALIF, L5-S1 ALIF |
| 19 | 53 | f | L4-L5 Spondylolisthesis, L5-S1 DDD | L4-L5 ALIF, L5-S1 ALIF |
| 20 | 35 | f | L4-L5 DDD, L5-S1 DDD | L4-L5 ALIF, L5-S1 ALIF |
| 21 | 37 | f | L4-L5 Facet arthropathy | L4-L5 ALIF |
| 22 | 43 | f | L4-L5 DDD | L4-L5 ALIF |
| 23 | 46 | f | L5-S1 DDD | L5-S1 ALIF |
| 24 | 40 | f | L4-L5 post laminectomy syndrome, L5-S1 DDD | L4-L5 ALIF, L5-S1 ALIF |
| 25 | 53 | f | L4-L5 DDD | L4-L5 ALIF |
| 26 | 32 | m | L4-L5 DDD, L5-S1 DDD | L4-L5 ALIF, L5-S1 ALIF |
| 27 | 35 | m | L5-S1 DDD | L5-S1 ALIF |
| 28 | 40 | f | L5-S1 post-laminectomy syndrome | L5-S1 ALIF |
| 29 | 36 | m | L5-S1 DDD | L5-S1 ALIF |
| 30 | 55 | f | L5-S1 DDD | L5-S1 ALIF |
| 31 | 32 | m | L5-S1 post-laminectomy syndrome | L5-S1 ALIF |
| 32 | 47 | m | L5-S1 DDD | L5-S1 ALIF |
| 33 | 63 | f | L5-S1 DDD | L5-S1 ALIF |
| 34 | 37 | m | L5-S1 DDD | L5-S1 ALIF |
| 35 | 39 | f | L4-L5 DDD | L4-L5 ALIF |
| 36 | 32 | m | L5-S1 DDD | L5-S1 ALIF |
| 37 | 41 | m | L5-S1 DDD | L5-S1 ALIF |
| 38 | 39 | f | L5-S1 Spondylolisthesis | L5-S1 ALIF, PSIF |
| 39 | 39 | f | L5-S1 Spondylolisthesis | L5-S1 ALIF, PSIF |
| 40 | 39 | m | L5-S1 recurrent disc herniation | L5-S1 ALIF |
| 41 | 36 | m | L5-S1 DDD | L5-S1 ALIF |
| 42 | 37 | m | Post-discectomy DDD | L5/S1 ALIF |
| 43 | 40 | m | L5/S1 DDD | L5/S1 ALIF |
| 44 | 40 | f | L5/S1 DDD | L5/S1 ALIF |
| 45 | 59 | m | Isthmic Sponylolisthesis | L5/S1 ALIF, PSIF |
| 46 | 53 | m | L5/S1 DDD | L5/S1 ALIF |
| 47 | 43 | m | L5/S1 DDD | L5/S1 ALIF |
| 48 | 45 | m | L5/S1 DDD | L5/S1 ALIF |
| 49 | 45 | m | L5/S1 DDD | L5/S1 ALIF |
| 50 | 40 | m | L5/S1 DDD | L5/S1 ALIF |
| 51 | 43 | f | L5/S1 isthmic spondylolisthesis | L5/S1 ALIF, PSIF |
| 52 | 37 | m | L5/S1 isthmic spondylolisthesis | L5/S1 ALIF, PSIF |
| 53 | 49 | m | L5/S1 DDD | L5/S1 ALIF |
| 54 | 41 | m | L5/S1 DDD | L5/S1 ALIF |
| 55 | 32 | m | L5/S1 DDD | L5/S1 ALIF |
| 56 | 59 | m | L5/S1 DDD | L5/S1 ALIF |
| 57 | 38 | m | Post-discectomy DDD | L5/S1 ALIF |
| 58 | 36 | m | Congenital Isthmic Spondylolisthesis | L5/S1 ALIF |
DDD – degenerative disc disease, ALIF – Anterior lumbar interbody fusion TDR – Total disc replacement PSIF – Posterior spinal instrumented fusion.
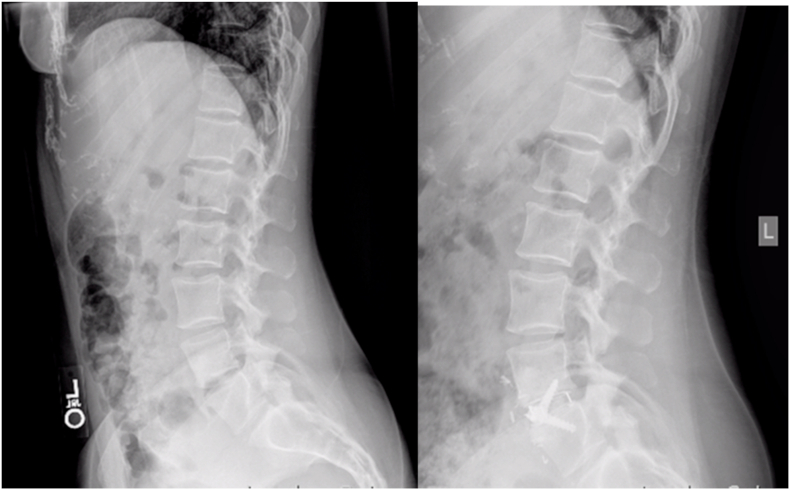
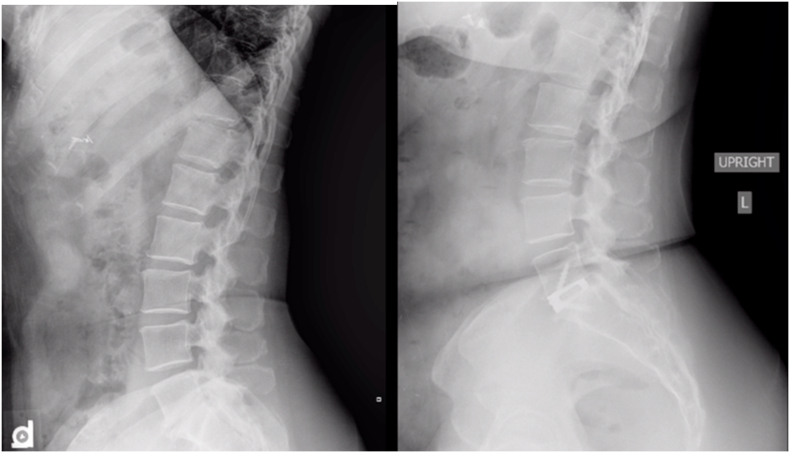
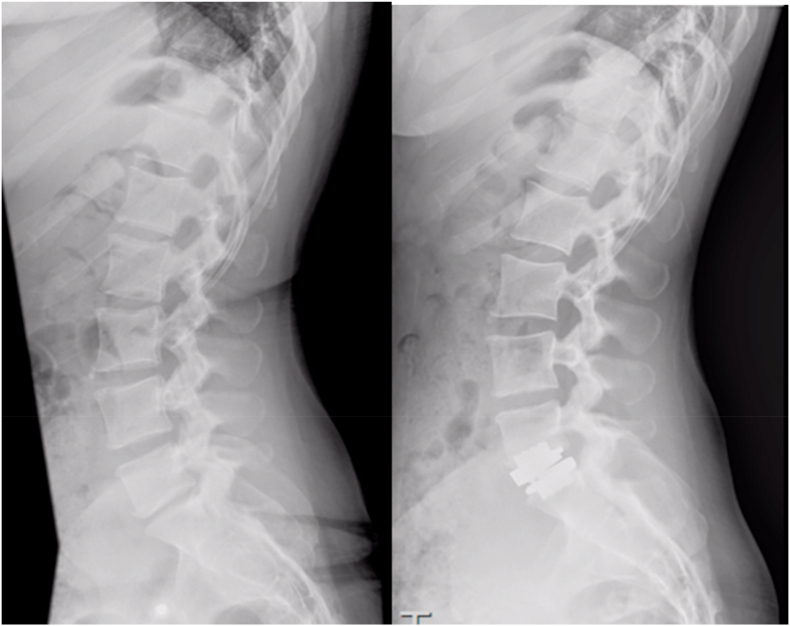
Of the 58 patients included, 47 underwent a single level procedure while the remaining 11 had two level procedures. All procedures were performed at the L4-L5 or L5-S1 levels. Of the single level surgeries, 4 were L4-L5 ALIFs, 41 were L5-S1 ALIFs with or without percutaneous pedicle screws, and 2 were L5-S1 TDRs. Of the patients undergoing two levels of surgery, six had L4-L5 and L5-S1 ALIFs, three had an L4-L5 ALIF with an L5-S1 TDR, one had a L4-L5 TDR and an L5-S1 ALIF, and one patient had TDRs at L4-L5 and L5-S1. Fig. 2, Fig. 3, Fig. 4, Fig. 5, Fig. 6, Fig. 7, Fig. 8 show preoperative and postoperative images of patients undergoing these various surgeries. The most common diagnosis was L5-S1 degenerative disc disease (N = 27, 46.5%), Table 1. The remainder of the diagnoses can be found in Table 1. The most common procedure performed was an L5-S1 ALIF with or without percutaneous posterior instrumentation (N = 41, 70.7%). Ninety percent of patients undergoing fusion had rhBMP-2 applied (52/58). Two patients had iliac crest cancellous autograft, one had allograft with platelet-derived growth factor and three patients had allograft bone putty.
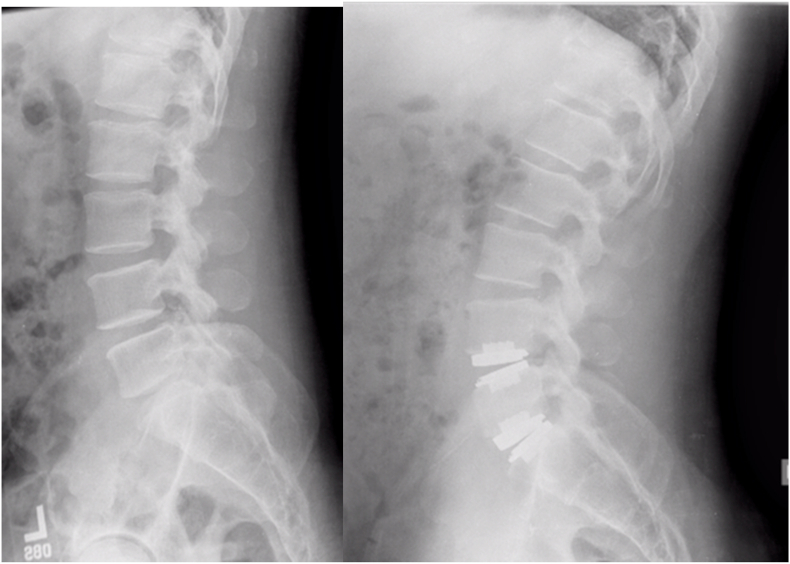
Fig. 2.
- Preoperative and Postoperative images of a patient undergoing a L4-L5 ALIF.
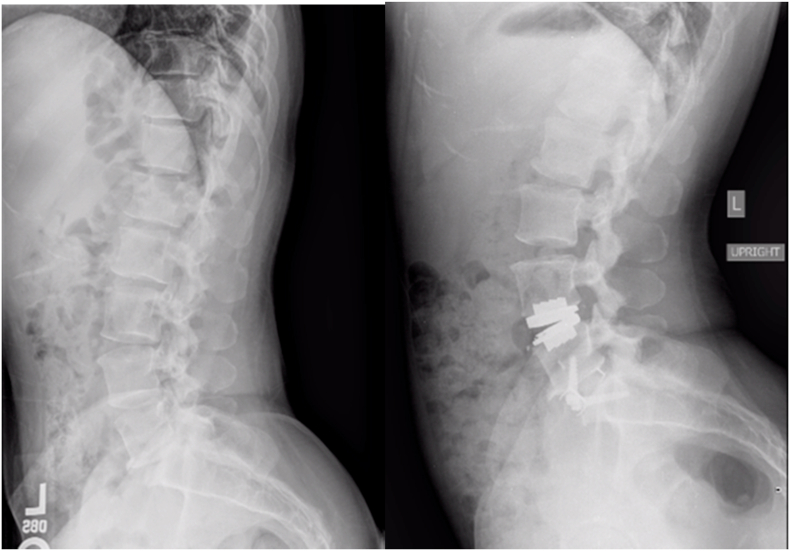
Fig. 3.
- Preoperative and Postoperative images of a patient undergoing a L5-S1 ALIF.
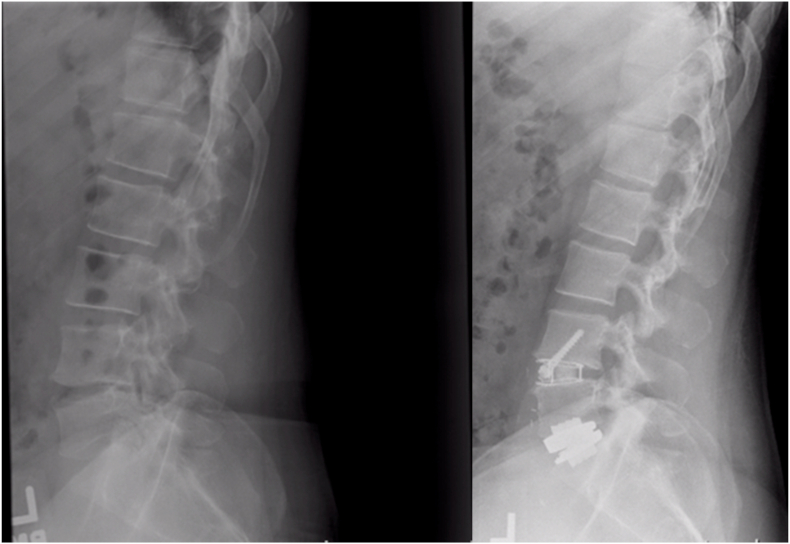
Fig. 4.
- Preoperative and Postoperative images of a patient undergoing a L5-S1 TDR.
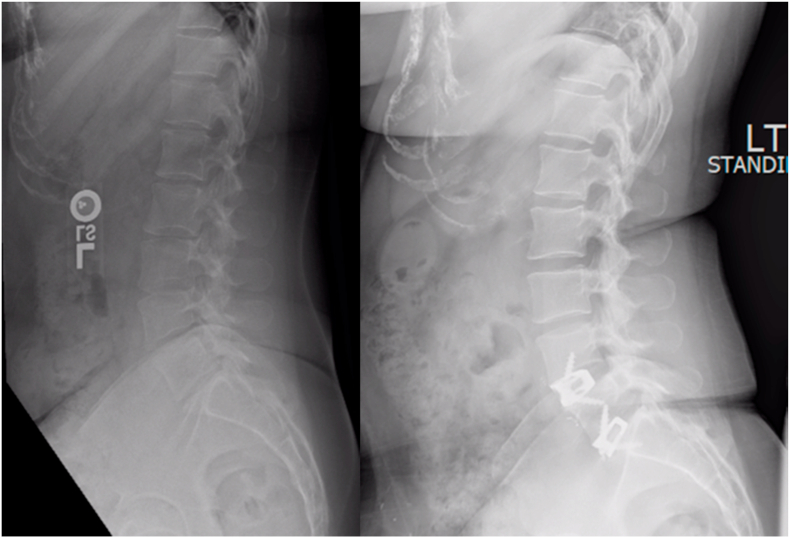
Fig. 5.
- Preoperative and Postoperative images of a patient undergoing a L4-L5 and L5-S1 TDR.
Fig. 6.
- Preoperative and Postoperative images of a patient undergoing a L4-L5 TDR with a L5-S1 ALIF.
Fig. 7.
Preoperative and Postoperative images of a patient undergoing a L4-L5 ALIF with a L5-S1 TDR.
Fig. 8.
Preoperative and Postoperative images of a patient undergoing a L4-L5 and L5-S1 ALIF.
During the study period, 21 patients (36.2%) developed postoperative radiculitis. However, all 21 patients demonstrated symptom resolution by the 3 month follow up. One patient who had surgery for post-laminectomy syndrome exhibited persistent right and left leg radiculopathy following the initial decompression. The patient had resolution of the right leg pain, but worsening left leg pain following his ALIF procedure. A repeat MRI showed lateral recess stenosis at L4-L5 and foraminal stenosis bilaterally at L5-S1. The patient had a transforaminal steroid injection with no significant relief of his symptoms. Ultimately he wished to undergo medical separation from the military and be discharged from the army rather than have any additional procedures. This patient was not included in the group of patients with postoperative radiculitis as there was evidence of continued neuroforaminal stenosis on repeat imaging. Of the patients who had rhBMP-2 applied, 19 (36.5%) developed radiculitis compared to 1 of 6 (16.7%) of patients not having rhBMP-2.
A summary of preoperative and postoperative Farfan ratios in relation to postoperative radiculitis is provided in Table 2. There was no significant difference for preoperative (11.1% ± 7.9% vs 9.3% ± 6.4%; p = 0.533) or postoperative disc height (20.3% ± 9.9% vs 23.09% ± 7.3%; p = 0.256) and the development of a postoperative radiculitis. There was, however, a significant correlation with height change and the development of a postoperative radiculitis (R = 0.262, p = 0.029), with increasing height change being mildly correlated with the development of postoperative radiculitis. Despite this mild correlation, the between group differences from height change were not statistically significant (13.78% of vertebral body width ± 8.23% in patients with radiculitis, vs 9.19% ± 7.97 for those without, P = 0.694).
Table 2.
Patient information reporting occurrence of post-operative radiculitis in relation to preoperative and postoperative Farfan ratios.
| Patient | Post-Operative Radiculitis (Y or N) | Pre-operative Farfan Ratio | Post-Operative Farfan Ratio | Farfan Ratio Change |
|---|---|---|---|---|
| 1 | N | 3.22 | 4.87 | 1.65 |
| 2 | Y | 10.20 | 31.86 | 21.65 |
| 13.50 | 23.46 | 9.96 | ||
| 3 | N | 10.53 | 19.18 | 8.66 |
| 4 | Y | 10.63 | 28.67 | 18.04 |
| 5 | N | 21.92 | 28.82 | 6.90 |
| 19.90 | 20.14 | 0.24 | ||
| 6 | N | 14.81 | 28.06 | 13.24 |
| 7 | N | 12.79 | 24.19 | 11.40 |
| 8a | N | −3.16 | 8.74 | 11.90 |
| 9 | N | 5.37 | 18.06 | 12.69 |
| 9.75 | 13.37 | 3.62 | ||
| 10 | N | 7.92 | 11.48 | 3.55 |
| 11 | Y | 17.54 | 22.01 | 4.47 |
| 12 | N | 23.20 | 25.67 | 2.47 |
| 13 | Y | 6.45 | 28.57 | 22.12 |
| 14 | Y | 15.73 | 28.39 | 12.65 |
| 15 | Y | 4.43 | 35.28 | 30.85 |
| 16 | N | 0.60 | 18.29 | 17.69 |
| 9.77 | 5.26 | −4.50 | ||
| 17 | Y | 4.59 | 8.57 | 3.98 |
| 4.27 | 16.86 | 12.59 | ||
| 18 | Y | 8.36 | 17.54 | 9.18 |
| 14.23 | 14.47 | 0.24 | ||
| 19 | N | 11.46 | 15.50 | 4.04 |
| 6.69 | 14.04 | 7.35 | ||
| 20 | Y | 0.28 | 24.90 | 24.63 |
| 3.92 | 9.66 | 5.74 | ||
| 21 | N | 2.60 | 12.46 | 9.87 |
| 22 | N | 0.58 | 0.61 | 0.03 |
| 23 | N | 10.22 | 9.14 | −1.07 |
| 24 | Y | 2.59 | 16.49 | 13.90 |
| 16.91 | 17.02 | 0.11 | ||
| 25 | Y | 0.77 | 16.77 | 16.00 |
| 26 | N | 15.88 | 12.00 | −3.88 |
| 9.17 | 16.10 | 6.93 | ||
| 27 | Y | 19.53 | 26.19 | 6.66 |
| 28 | N | 1.94 | 16.92 | 14.99 |
| 29 | N | 11.47 | 20.51 | 9.04 |
| 30 | Y | 0.28 | 7.81 | 7.53 |
| 31 | N | 7.41 | 17.97 | 10.56 |
| 32 | Y | 8.44 | 31.08 | 22.64 |
| 33 | Y | 8.08 | 17.21 | 9.13 |
| 34 | N | 11.86 | 19.97 | 8.11 |
| 35 | Y | 11.17 | 16.52 | 5.35 |
| 36 | N | 4.60 | 19.67 | 15.07 |
| 37 | y | 2.95 | 28.95 | 26.00 |
| 38 | N | 7.97 | 21.33 | 13.36 |
| 39 | Y | 7.91 | 21.04 | 13.13 |
| 40 | N | 9.82 | 16.57 | 6.75 |
| 41 | N | 2.26 | 16.03 | 13.78 |
| 42 | Y | 11.13 | 22.24 | 11.11 |
| 43 | N | 28.43 | 40.43 | 12.00 |
| 44 | Y | 3.71 | 22.36 | 18.65 |
| 45 | N | 12.06 | 39.25 | 27.19 |
| 46 | N | 8.45 | 30.33 | 21.89 |
| 47 | N | 27.59 | 39.44 | 11.84 |
| 48 | N | 5.28 | 23.65 | 18.37 |
| 49 | N | 5.78 | 15.84 | 10.05 |
| 50 | N | 29.46 | 46.35 | 16.89 |
| 51 | N | 15.57 | 33.56 | 17.99 |
| 52 | N | 11.70 | 22.90 | 11.21 |
| 53 | N | 8.82 | 37.18 | 28.36 |
| 54 | Y | 19.74 | 34.04 | 14.30 |
| 55 | N | 25.94 | 26.80 | 0.86 |
| 56 | N | 7.82 | 29.74 | 21.92 |
| 57 | N | 25.77 | 17.16 | −8.61 |
| 58 | N | 18.67 | 21.40 | 2.73 |
Patient 8 had a significant amount of kyphosis at the operative level preoperatively, leading to a larger posterior disc height than anterior and a negative Farfan Ratio.
ROC curve analysis found a threshold of 9.91% height change relative to the vertebral body width was 65.2% sensitive and 52.2% specific for development of a postoperative radiculitis, however, this did not reach statistical significance (p = 0.071, AUC = 0.649), Fig. 9.
Fig. 9.
Receiver Operating Characteristic Curve demonstrating the lack of a significant threshold finding for change in disc height and the development of post-operative radiculitis.
There was no statistical significance of patients developing symptoms between patients undergoing one versus two level surgery (X2=1.9765, p=0.18). There was also no statistical significance of patients developing symptoms between patients undergoing hybrid surgery (ALIF with TDR) versus those undergoing two level ALIF (X2 = 1.9765, p = 0.16).
4. Discussion
In this study, we identified a 36.2% rate of developing a postoperative radiculitis following anterior lumbar surgery. There was a mild correlation between change in discal height and the development of a postoperative radiculitis, however, between groups differences did not reach statistical significance. Additionally, patients treated with rhBMP-2 appeared to have a higher rate of developing postoperative radiculitis compared to other graft sources (36.5% vs 17%), unfortunately the number of patients not treated with rhBMP-2 were too few to make a statistical comparison. This number, however, is similar to what Lee reported in patients undergoing anterior lumbar surgeries.5 We also found that all of the symptoms resolved by the 3 month postoperative appointment.
There are multiple studies in the literature discussing transient leg pain or radiculitis in patients undergoing interbody fusion with the use of rhBMP-2. In 2009, Mindea et al. published the first study looking at this phenomenon showing a rate of 11% postoperative nonstructural radiculitis in patients when using rhBMP-2 during TLIF procedures. All symptoms were on the side of the TLIF procedure, and in their study, all resolved within 6 weeks.8 Likewise, in 2012, Rowan et al. showed there was a 2.33 odds ratio of developing postoperative radiculitis in patients having a posterolateral or posterior fusion with the use of rhBMP-2. They also found that patients treated with rhBMP-2 filled interbody cages were twice as likely to have non-structural radiculitis compared to those treated without.9 In 2016 Villavicencio et al. looked at a dose dependent rate of postoperative radiculitis with the use of rhBMP-2. They found an overall rate of 11.3% of postoperative radiculitis in patients undergoing TLIF surgery. They did not find a correlation with the dose of rhBMP-2 used. A majority of their symptoms resolved by 6 months postoperatively. 10 Finally, in 2017 Lee et al. evaluated postoperative radiculitis in patients undergoing ALIF procedures. They found 40% of patients developed radiculitis when rhBMP-2 was used compared to 9.52% of patients when allograft was used.5
In contrast to the above listed studies, and the current study, Sebastian et al., prospectively evaluated patients undergoing TLIF procedures with the use of rhBMP-2 and compared them to patients undergoing TLIF without the use of BMP. They found no difference in the rate of postoperative radiculitis. Additionally, they found a similar improvement in preoperative leg symptoms in both group.11
The results of this study also suggest that these symptoms may be related to an acute stretch phenomenon on the nerve root. There have been multiple animal models investigating the development of nerve changes following acute stretch. Ming et al. showed that sciatic nerve blood flow and somatosensensory evoked potentials both decreased significantly after lengthening of the femur 24% and 32%, and this corresponded to decreased neurologic function.12 Additionally, there have been multiple reports of motor, sensory and mixed motor/sensory neuropathies following limb lengthening procedures, valgus knee injuries and limb lengthening after total hip arthroplasty.13, 14, 15, 16 Finally, a study by Kershner et al. used a cadaveric model to show the effects of spinal column lengthening on exiting nerve roots. They found that lengthening of the spinal column by 4 cm caused proximal migration of the spinal cord by 2.8 mm. They found a significant increase in dorsal nerve roots being tethered by intrathecal ligaments during lengthening. They speculated that this is a cause of lumbar back pain in astronauts during space flight.17
To date two studies list post-operative radiculitis as complications in patients undergoing ALIF procedures. Lee et al. reviewed 41 patients undergoing ALIF procedures. They treated 20 patients with allograft and 21 patients with rhBMP-2. They found that overall 10 patients experienced a postoperative “radiculitis,” 2 in the allograft group and 8 in the rhBMP-2 group.5 There was a trend towards more complications in the rhBMP-2 group. Similarly, Hirabalek et al. compared their results in patients undergoing anterior versus lateral interbody fusions. They found a rate of 8.3% radiculitis in their ALIF patients, 6 of which were groin numbness, while 4 complained of pain. They did not discuss time to resolution or possible causes of the symptoms.6
The results of this study, however, should be viewed in the light of its limitations. First, this is a retrospective study, relying on review of postoperative notes to identify patients with neurologic symptoms. The number of patients affected may be under-reported in this study if the symptoms were not disclosed during their follow up visit. Likewise, the number of patients included in this study is relatively small. Additionally, the number of patients not treated with rhBMP-2 for their fusion were too few to develop a statistical comparison. Finally, the follow up in this study is short, but with the primary outcome being resolution of post-operative radiculitis, and all patients with these symptoms resolved within 3 months, our primary outcome was achieved in all patients. Future prospective research is needed to assess the development of a postoperative radiculitis following anterior lumbar surgery.
In conclusion, this study identified a 36.2% rate of postoperative radiculitis following anterior lumbar surgery, with 100% of patients demonstrating spontaneous symptom resolution within 3 months of surgery. There was a significant correlation between postoperative radiculitis and change in disc height following surgery. There also appeared to be an increased rate when rhBMP-2 was used, with 36.5% of patients developing postoperative radiculitis when rhBMP-2 was used when compared to 17% when rhBMP-2 was not used. This information can aid in the preoperative and postoperative counseling for patients undergoing anterior lumbar surgery.
Funding
No funding was received for this study. Each author certifies that he or she has no commercial associations that might pose a conflict of interest in connection with the submitted article.
The opinions or assertions contained herein are the private views of the authors and are not to be construed as official or reflecting the views of the Department of Defense or US Government. The authors are employees of the US government. This work was prepared as part of their official duties and, as such there is no copyright to be transferred.
The Device(s)/Drug(s) is/are FDA-approved or approved by corresponding national agency for this indication.
References
- 1.Crook H.V. Anterior lumbar interbody fusion. Clin Orthoped Related Res. 1982;165:157–170. [PubMed] [Google Scholar]
- 2.Mobbs R., Loganathan A., Yeung V., Rao P. Indications for anterior lumbar interbody fusion. Orthop Surg. 2013;5(3):153–163. doi: 10.1111/os.12048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Heary R., Yanni D., Halim A., Benzel E. fourth ed. Online; Philadelphia: 2017. Anterior Lumbar Interbody Fusion. Spine Surgery. [Google Scholar]
- 4.Sasso R., Best Na, Mummaneni P., Reily T., Hussain S. Analysis of operative complications in a series of 471 anterior lumbar interbody fusion procedures. Spine. 2005;30(6):670–674. doi: 10.1097/01.brs.0000155423.18218.75. [DOI] [PubMed] [Google Scholar]
- 5.Lee D.D., Kim J.Y. A comparison of radiographic and clinical outcomes of anterior lumbar interbody fusion performed with either a cellular bone allograft containing multipotent adult progenitor cells or recombinant human bone morphogenetic protein-2. J Orthop Surg Res. 2017;12:126–134. doi: 10.1186/s13018-017-0618-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hirabalek L., Adamus M., Gryga A., Wanek T., Tucek P. A comparison of complication rate between anterior and lateral approaches to the lumbar spine. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2014;158(1):127–132. doi: 10.5507/bp.2012.079. [DOI] [PubMed] [Google Scholar]
- 7.Farfan H.F. Lea and Febiger; Philadelphia: 1972. Mechanical Disorders of the Low Back; pp. 33–40. [Google Scholar]
- 8.Mindea S., Shih P., Song J. Recombinant, human bone morphogenetic protein-2-induced radiculitis in elective minimally invasive transforaminal lumbar interbody fusions. Spine. 2009;34(14):480–1484. doi: 10.1097/BRS.0b013e3181a396a1. [DOI] [PubMed] [Google Scholar]
- 9.Rowan F., O'Malley N., Poynton A. RhBMP-2 Use in lumbar fusion surgery is associated with transient immediate post-operative leg pain. Eur Spine J. 2012;21:1331–1337. doi: 10.1007/s00586-011-2113-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Villavicencio A., Burneikiene S. RhBMP-2-Induced radiculitis in patients undergoing transforaminal lumbar interbody fusion: relationship to dose. Spine J. 2016;16:1208–1212. doi: 10.1016/j.spinee.2016.06.007. [DOI] [PubMed] [Google Scholar]
- 11.Sebastian A., Wanderman N., Currier B. Prospective evaluation of radiculitis following bone morphogenic protein-2 Use for transforaminal interbody arthrodesis in spine surgery. Asian Spine J. 2019;13(4):544–555. doi: 10.31616/asj.2018.0277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ming J., Kuo-An L., Chin-Liang S., Yoshiki Y. Changes in conduction, blood flow, histology, and neurological status following acute nerve-stech injury induced by femoral lengthening. J Orthop Res. 2000;18:149–155. doi: 10.1002/jor.1100180121. [DOI] [PubMed] [Google Scholar]
- 13.Nogueira M., Paley D., Bhave A., Herbert A., Nocente C., Herzenberg J. Nerve lesions associated with limb –lengthening. J Bone Joint Surg. 2003;85A(8):1502–1510. doi: 10.2106/00004623-200308000-00011. [DOI] [PubMed] [Google Scholar]
- 14.Faber F., Keesen W., Roermund P. Complications of leg lengthening: 46 procedures in 28 patients. Acta Orthop Scand. 1991;62(4):327–332. doi: 10.3109/17453679108994463. [DOI] [PubMed] [Google Scholar]
- 15.Sedel L., Nizard R. Nerve grafting for traction injuries of the common peroneal nerve. J Bone Joint Surg. 1993;75(B):772–774. doi: 10.1302/0301-620X.75B5.8376437. [DOI] [PubMed] [Google Scholar]
- 16.Farrell C., Springer B., Haidukewych G., Morrey B. Motor nerve palsy following primary total hip arthroplasty. J Bone Joint Surg. 2005;87A(12):1619–2625. doi: 10.2106/JBJS.C.01564. [DOI] [PubMed] [Google Scholar]
- 17.Kershner D., Binhammer R. Intrathecal ligaments and nerve root tension: possible sources of lumbar pain during spaceflight. Aviat Space Environ Med. 2004;75(4):354–358. [PubMed] [Google Scholar]