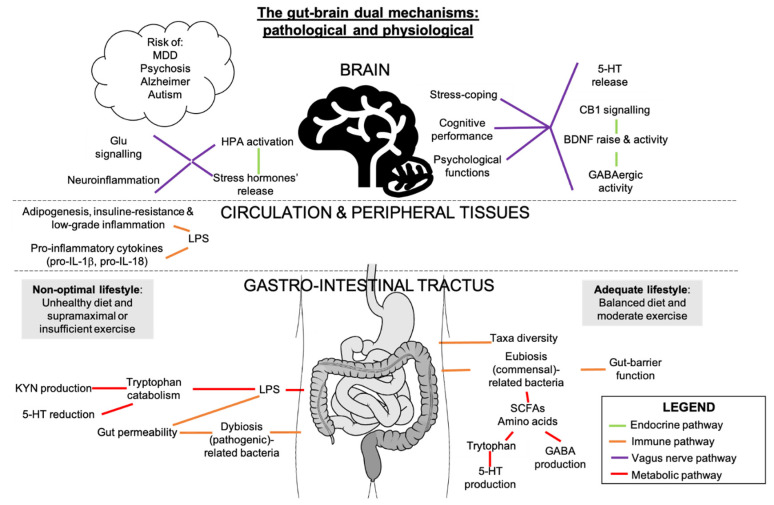
Figure 3.
Gut-brain axis routes in mental health. The gut microbiota and the CNS are connected through immune, vagus nerve, metabolic and neuroendocrine-mediated pathways. These processes can all contribute to mental health or illness where eCBs and other molecules interfere depending on the cell or tissue. SCFAs are primary products of the fermentation of complex fibers by gut microbes in an intestinal balanced environment i.e., eubiosis. SCFAs induce GABA and serotonin (5-HT) production, attenuating depressive-like behavior. These neurotransmitters can also exert their roles in the brain where, with BDNF and CB1, they can bring positive mood changes. On the other hand, LPS-mediated low-grade inflammation in the gut caused by disruption of microbiota composition (dysbiosis) and intestinal barrier perturbation, would induce tryptophan degradation, raising kynurenine (KYN) levels and reducing 5-HT release, two events associated with depressive mood. The action of pro-inflammatory interleukins (pro-IL) and LPS would evolve in an inflammatory state in the brain. Inflammatory stimuli and stressor exposure would engage HPA overstimulation. HPA function through GC and ACTH circuitry release in gut microbiota-mediated anxiety-like behaviors is notable (Kang et al., 2014). Strong bidirectional correlations are found between major depressive disorder (MDD), psychosis, Alzheimer’s disease, autism spectrum disorder and intestinal dysbiosis, which correlates with the dietary and exercise patterns.