Abstract
Background
This report is a case of bilateral vocal cord granulomas (VCG) in a 9-year-old child presenting as an airway foreign body and stridor following prolonged intubation due to COVID-19 pneumonia complicated by multisystem inflammatory syndrome in children (MIS-C).
Case presentation
This case reports a 9-year-old male who presented to the emergency department with acute stridor concerning for airway obstruction. X-ray findings suggested an airway foreign body; however, on rigid bronchoscopy, ball-valving bilateral VCG obstructing 90% of the glottic airway were identified. After excision of the VCGs, the patient's symptoms resolved with no postoperative complications.
Conclusion
With suspected foreign body aspiration in a pediatric patient with a history of prolonged intubation, it is important to consider a broad differential diagnosis. VCGs are rare complications of prolonged intubation that could be in children with prior history of intubation following COVID-19 pneumonia.
Keywords: Vocal cord granulomas, Foreign body, Pediatric, COVID-19, Multisystem inflammatory syndrome
Introduction
Vocal cord granulomas (VCG) are benign laryngeal lesions that occur at the vocal process of the arytenoid [1]. Traditionally, VCGs in adults arise due to prolonged intubation, inappropriate voice use such as repetitive throat clearing and coughing, or laryngopharyngeal reflux [2]. Prolonged intubation, variably defined as lasting greater than 24 hours or 7 days, causes an inflammatory response in the mucosa of the airway due to the endotracheal tube contact and intubation trauma that can lead to reactive granuloma formation [3,4]. These most commonly occur at the vocal cord process. Symptoms commonly include dysphonia, dyspnea and foreign body sensation. When bilateral VCGs are present, patients can present with more severe symptoms of upper airway obstruction including stridor [5]. VCGs are rarely reported in children as few require prolonged intubation and increased awareness to use smaller endotracheal tubes and conservative endotracheal cuff pressures compared to adults. However, in the setting of COVID-19 pneumonia and MIS-C, more children are requiring prolonged intubation making them susceptible to post-intubation complications [6]. In this report, we present a case of a 9-year-old boy who presented acutely with progressive stridor and dysphonia due to bilateral VCGs that were originally mistaken for supraglottic foreign bodies causing airway obstruction.
Case presentation
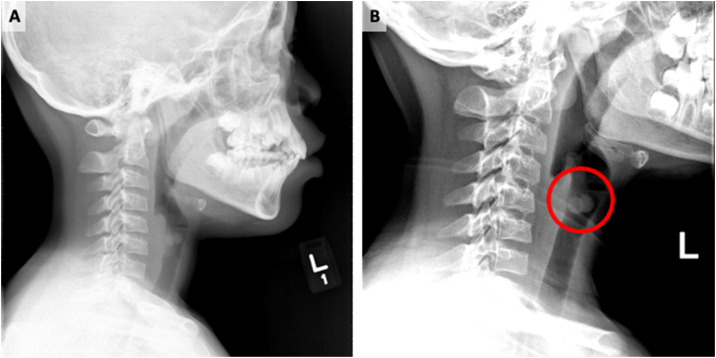
A 9-year-old male with past medical history of prematurity (born at 32-weeks gestation) and COVID-19 pneumonia complicated by MIS-C requiring intubation presented to the emergency department (ED) with acute onset of inspiratory stridor and dyspnea. The patient was intubated for 3 days and, following extubation, developed progressive respiratory symptoms including snoring, dysphonia, dyspnea with audible stridor. In the week leading to presentation, he had worsening shortness of breath (SOB) and dysphonia that ultimately progressed to persistent inspiratory stridor and inability to lay flat. A lateral cervical spine x-ray performed at presentation showed two round opacities inferior to the vallecula at the level of the larynx measuring 8mm, concerning for ingested foreign bodies (FB) (Fig. 1 ). The patient was stabilized using racemic epinephrine and steroids and transferred to our tertiary care pediatric hospital. Otolaryngology was consulted in the ED, and an emergency direct laryngoscopy with a rigid endoscope was performed in the operating room (OR) for further evaluation and possible emergency intubation.
Fig. 1.
(A) Lateral cervical spine x-ray shows two round opacities inferior to the vallecula at the level of the larynx measuring 8mm. (B) Shows more radiolucent airway with prominent round opacities.
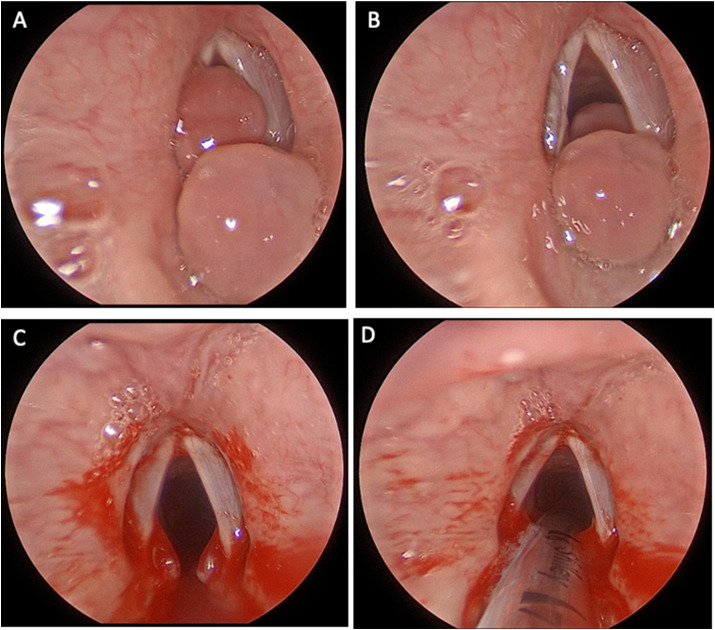
Patient was anesthetized using propofol gas, bag mask ventilation was performed prior to paralysis. Oxygenation and ventilation was provided via bag mask without intubation. On rigid endoscopy, bilateral ball-valving VCGs originating from the vocal processes of the arytenoids were appreciated obstructing 90% of the glottis and laryngeal inlet (Fig. 2 A and B). Both granulomas were excised using forceps and coblator coagulation for control of hemostasis. The glottic airway was patent following removal of the obstructing granulomas (Fig. 2C). Bronchoscopy showed no evidence of subglottic obstruction, foreign bodies, or stenosis. Patient's airway was then secured with an endotracheal tube prior to emergence (Fig. 2D). Patient was successfully extubated in the operating room and monitored overnight in the pediatric intensive care unit. Intraoperative video of the endoscopic procedure to remove the bilateral granulomas and secure the airway is shown below.
Fig. 2.
(A) Both vocal cord granulomas are observed ball-valving into the glottis causing near obstruction of the airway. (B) Shows both vocal cord granulomas when ball-valving is not obstructing the airway. (C) Patent supraglottic, glottic and infraglottic airway after removal of both granulomas. (D) Post-endotracheal intubation to secure the airway and allow for emergence.
On postoperative day 1, the patient reported no respiratory complaints and was tolerating oral intake. Voice was normal and he was able to sleep uneventfully in a supine position. Patient was discharged home with high-dose prednisone for 3 days and a proton pump inhibitor to limit reflux laryngitis for 2 weeks. On one week follow-up visit in otolaryngology clinic, the patient's mother reported immediate and persistent improvement in sleep, voice and breathing following the procedure. On flexible nasolaryngoscopy, the upper aerodigestive tract including the supraglottis, glottis and subglottis were patent. No recurrent vocal cord granulomas were appreciated and vocal cord mobility was preserved bilaterally.
Discussion
VCGs are ordinarily unilateral and lead to minor symptoms such as dysphonia that can be managed conservatively with voice therapy and proton pump inhibitors to limit laryngopharyngeal reflux. However, in the case of bilateral granulomas presenting acutely with stridor and airway obstruction, immediate surgical intervention is necessary. In the present case, the VCGs resembled a foreign body on lateral chest x-ray at the level of the larynx.
VCGs are benign lesions that rarely occur in children and present commonly with dyspnea, stridor and dysphonia. A cohort study of children with the average age of 2 years, including a majority of premature neonates, found that there is a significantly higher incidence of granulomas in children with history of prior intubation than children without; of the children with history of intubation, 3.6% presented with granulomas [7]. However, most children with laryngeal pathology presented with minor lesions such as vocal cord nodules, cysts or ulcers [7]. The pediatric larynx has loose areolar submucosal tissue as well as a rich vascular and lymphatic supply facilitating faster healing making granulomas less common in children [8]. Due to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infections, some pediatric patients with COVID-19 pneumonia and MIS-C require prolonged intubation [9]. A recent study, investigating post-intubation adverse events in a cohort of 18 pediatric patients intubated for COVID-19 associated MIS-C, found new onset dysphagia, dysphonia and snoring to be the most commonly reported symptoms [10]. Furthermore, the most commonly observed post-intubation endoscopy findings were post-inflammatory changes of laryngeal mucosa and weakness of unilateral or bilateral vocal cords [10]. There were no reports of granuloma formation in this cohort of patients. While our patient did report new onset snoring post-intubation, he also presented acutely with bilateral granulomas; a novel sequela of post-intubation trauma not yet reported in the pediatric COVID-19 related MIS-C cohort of patients. It is possible that the mucosal inflammation related to COVID-19 in conjunction with mucosal inflammation from prolonged intubation may put pediatric patients at increased risk of VCGs.
In adults, common causes of laryngeal lesions that may present with acute respiratory symptoms such as stridor and dysphonia include squamous cell carcinoma, vascular lesions such as hemangiomas, Kaposi sarcoma, or angiosarcoma, as well as inflammatory and infectious processes, namely sarcoidosis, fungal or mycobacterial infection [11]. These etiologies should all be on the differential diagnosis when considering a glottic obstruction. However, in patients with history of recent intubation and progressive inspiratory stridor, subglottic stenosis is an important consideration as this influences management of the airway with regards to options for endotracheal intubation vs. need for emergent tracheostomy. In any patient presenting with progressive stridor, emergent bronchoscopy may be required to evaluate the upper aerodigestive tract and trachea to decide how to best proceed with airway management.
Commonly, VCGs are managed medically and only refractory cases require surgical or laser excision. Medical management includes a trial of anti-reflux therapy with a proton pump inhibitor, speech therapy, and inhaled steroids [12]. Refractory cases can be managed with botulinum toxin with some studies reporting up to 100% resolution rates [12]. Surgery was reserved for refractory cases or patients presenting with airway obstruction, and surgical techniques included conventional cold steel excision, carbon dioxide laser ablation or potassium titanyl phosphate laser ablation [2,12].
In the emergency setting, it can be difficult to stabilize patients' airways that present with near-total obstruction which can include vocal cord granulomas or subglottic stenosis. In our case, the patient was consciously sedated while maintaining spontaneous respirations. Then, a bronchoscopy was performed with tracheal oxygen supplementation, providing a short time period to examine the glottic lesions and to carefully excise obstructing tissue. The patient was subsequently intubated to facilitate ventilations and emergence.
To our knowledge, this is the first case of pediatric bilateral post-intubation VCGs causing acute airway obstruction in the setting of COVID-19 related MIS-C to be reported in the literature. COVID-19 pneumonia and MIS-C requiring intubation have not yet demonstrated associations with specific post-intubation injuries.
Conclusion
This case presentation illustrates that VCGs are an unusual cause of acute airway obstruction that can be mistaken for foreign bodies. VCGs are rare complications of prolonged intubation that could be present in children with prior history of intubation in the setting of COVID-19 pneumonia complicated by MIS-C.
Financial Support
None.
Ethical statement for solid state ionics
Hereby, I Leonardo Torres consciously assure that for the manuscript “Pediatric Bilateral vocal cord granulomas presenting as airway foreign body following prolonged intubation due to COVID-19 related multisystem inflammatory syndrome” the following is fulfilled:
-
1)
This material is the authors' own original work, which has not been previously published elsewhere.
-
2)
The paper is not currently being considered for publication elsewhere.
-
3)
The paper reflects the authors' own research and analysis in a truthful and complete manner.
-
4)
The paper properly credits the meaningful contributions of co-authors and co-researchers.
-
5)
The results are appropriately placed in the context of prior and existing research.
-
6)
All sources used are properly disclosed (correct citation). Literally copying of text must be indicated as such by using quotation marks and giving proper reference.
-
7)
All authors have been personally and actively involved in substantial work leading to the paper, and will take public responsibility for its content.
The violation of the Ethical Statement rules may result in severe consequences.
To verify originality, your article may be checked by the originality detection software iThenticate. See also http://www.elsevier.com/editors/plagdetect.
I agree with the above statements and declare that this submission follows the policies of Solid State Ionics as outlined in the Guide for Authors and in the Ethical Statement.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.xocr.2021.100311.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Lemos E.M., et al. Vocal process granuloma: clinical characterization, treatment and evolution. Braz J Otorhinolaryngol. 2005;71(4):494–498. doi: 10.1016/S1808-8694(15)31205-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kraimer K.L., Husain I. Updated medical and surgical treatment for common benign laryngeal lesions. Otolaryngol Clin. 2019;52(4):745–757. doi: 10.1016/j.otc.2019.03.017. [DOI] [PubMed] [Google Scholar]
- 3.Jang M., Basa K., Levi J. Risk factors for laryngeal trauma and granuloma formation in pediatric intubations. Int J Pediatr Otorhinolaryngol. 2018;107:45–52. doi: 10.1016/j.ijporl.2018.01.008. [DOI] [PubMed] [Google Scholar]
- 4.Martins R.H.G., et al. Treatment of laryngeal granulomas. Int Arch Otorhinolaryngol. 2019;23(3):e322–e324. doi: 10.1055/s-0039-1688456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cuestas G., et al. [Post-intubation laryngeal granuloma: a rare complication of tracheal intubation in pediatrics. Case report] Arch Argent Pediatr. 2017;115(5):e315–e318. doi: 10.5546/aap.2017.e315. [DOI] [PubMed] [Google Scholar]
- 6.Naunheim M.R., et al. Laryngeal complications of COVID-19. Laryngoscope Investig Otolaryngol. 2020;5(6):1117–1124. doi: 10.1002/lio2.484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Weiss M., et al. Endoscopic airway findings in children with or without prior endotracheal intubation. Paediatr Anaesth. 2013;23(2):103–110. doi: 10.1111/pan.12102. [DOI] [PubMed] [Google Scholar]
- 8.Elsamma Y.E., et al. Laryngeal intubation granuloma. J Laryngol Otol. 1971;85(9):939–946. doi: 10.1017/s0022215100074259. [DOI] [PubMed] [Google Scholar]
- 9.Hennon T.R., et al. COVID-19 associated multisystem inflammatory syndrome in children (MIS-C) guidelines; a western New York approach. Prog Pediatr Cardiol. 2020:101232. doi: 10.1016/j.ppedcard.2020.101232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cheong R.C.T., et al. Otolaryngologic manifestations in pediatric inflammatory multisystem syndrome temporally associated with COVID-19. JAMA Otolaryngol Head Neck Surg. 2021 doi: 10.1001/jamaoto.2020.5698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Devaney K.O., Rinaldo A., Ferlito A. Vocal process granuloma of the larynx-recognition, differential diagnosis and treatment. Oral Oncol. 2005;41(7):666–669. doi: 10.1016/j.oraloncology.2004.11.002. [DOI] [PubMed] [Google Scholar]
- 12.Karkos P.D., et al. Vocal process granulomas: a systematic review of treatment. Ann Otol Rhinol Laryngol. 2014;123(5):314–320. doi: 10.1177/0003489414525921. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.