Abstract
Background:
Lipedema is a loose connective tissue disease affecting the limbs of women, that is difficult to lose by diet, exercise, or bariatric surgery. Publications from Europe demonstrate that lipedema reduction surgery improves quality of life for women with lipedema. There are no comparable studies in the United States (USA). The aim of this study was to collect data from women with lipedema in the USA who have undergone lipedema reduction surgery in the USA to determine if quality of life, pain, and other measures improved after lipedema reduction surgery.
Methods:
Subjects were recruited and consented online for a 166-item questionnaire in REDCap. In total, 148 women answered the questionnaire after undergoing lipedema reduction surgery in the USA. Significance set at P < 0.05 was determined by ANOVA, Tukey’s multiple comparison test, or paired t-test.
Results:
Quality of life improved in 84% and pain improved in 86% of patients. Ambulation improved most in lipedema Stage 3 (96%). Weight loss occurred in all stages by 3 months after surgery. Complications included growth of loose connective tissue within and outside treated areas, tissue fibrosis, anemia, blood clots, and lymphedema.
Conclusions:
Women with lipedema noticed significant benefits after lipedema reduction surgery in the USA. Prospective studies are needed to assess benefits and complications after lipedema reduction surgery in the USA.
INTRODUCTION
Lipedema is a painful disease occurring almost exclusively in women in which abnormal fat (loose connective tissue; LCT) grows out of proportion on the limbs, sparing the trunk, hands, and feet. Lipedema LCT contains excess fibrotic connective tissue and fluid bound to glycosaminoglycans within the extracellular matrix,1,2 resulting in tissue resistant to loss after diet, exercise, or bariatric surgery.3–5 Tissue fibrosis may be a primary mechanism that makes it difficult for patients with lipedema to lose weight.6,7 Lipedema tissue contains abnormal lymphatic vessels8 and bruises easily demonstrating fragility of blood vessels.
Lipedema is graded by stage. In Stage 1, the skin surface is smooth over an enlarged hypodermis. Stage 2 skin is uneven, with indentations in the skin and fat and larger hypodermal masses. Large extrusions of tissue in Stage 3 inhibit mobility and fluid flux through the tissue. When lymphedema occurs with lipedema, it is called lipolymphedema. Most women with lipolymphedema also have a body mass index consistent with obesity.
The prevalence of lipedema is unknown, but estimates range from ~5% to 19%,9–12 meaning millions of women in the USA may be affected.
Standard conservative therapy for lipedema includes complete decongestive therapy with manual lymphatic drainage, sequential pneumatic compression pumps, compression garments, food, and exercise programs to maintain weight.
Lipedema reduction surgery is a standard method of improving the lives of patients with lipedema in Germany and is now being performed in the USA. Lipedema reduction surgery includes suction-assisted lipectomy (liposuction) modified to reduce injury to lymphatic vessels and manual extraction or excision. Most authors publishing on lipedema reduction surgery show improved quality of life and pain reduction by employing the tumescent technique of modified suction lipectomy with blunt cannulas, with or without a power-assisted liposuction hand piece.13–15 Water-assisted liposuction16,17 and laser-assisted liposuction18 have shown some success for patients with lipedema.
Liposuction is generally considered cosmetic. However, because lipedema LCT is associated with pain, lymphedema, obesity, venous disease,19,20 hypermobile joints,21 and dysmobility, lipedema reduction surgery is medically necessary to reduce LCT that cannot be reduced by usual measures.
Publications from Germany attest to the benefits of lipedema reduction surgery, supporting this procedure as medically necessary. Rapprich et al found that 25 women with lipedema, who had lipedema reduction surgery six months prior, had a 7% reduction in leg volume, pain reduction on a visual analogue scale of 7 down to 2 (P < 0.001), and improvement in quality of life.22 Wollina et al found a similar reduction in pain after surgery for 111 women with lipedema.23 Dadras et al followed 25 women at least 2 years after liposuction for lipedema and found a significant reduction in spontaneous pain, sensitivity to pressure, feeling of tension, bruising, and general impairment (P < 0.0001).24 The authors also found the women had a significant reduction in the need for complete decongestive therapy. Baumgartner et al followed 85 women with lipedema 4, 8 and 12 years after liposuction and found that benefits in pain, restriction of movement, edema, quality of life, and bruising at 4 years after liposuction persisted up to 12 years.25
There are no data on the benefits of lipedema reduction surgery in the USA. This article presents self-reported data by women with lipedema who have undergone lipedema reduction surgery in the USA, with a focus on pain and quality of life that have been followed long-term in studies out of Germany.
MATERIALS AND METHODS
Participants
This study was approved by the University of Arizona Human Protections Program; ClinicalTrials.gov NCT02838277. The study was advertised on the internet, requesting participation by women who had undergone lipedema reduction surgery in the USA; due to the open nature of the survey, anyone could participate. All participants signed a consent form before answering a questionnaire designed on REDCap.26 Participants included in the study were women diagnosed with lipedema stages 1–3 or women with Stage 3 and lymphedema (lipolymphedema) who had undergone at least one lipedema reduction surgery procedure in the USA from 2013 to 2018. Participants were excluded from the study if they did not have lipedema, did not have lipedema reduction surgery, or had their procedure outside the USA.
Statistics
Data are reported as average ± SD. Differences amongst groups were analyzed by 1-way ANOVA followed by Tukey’s multiple comparison test (GraphPad Prism Software 8; San Diego, Calif.). Differences between pre- and postsurgery within subjects were evaluated by a paired t-test. Significance was set at P < 0.05.
Questionnaires
Body shape questionnaire (BSQ): The BSQ has 34 subjective questions about body shape. Proposed scoring: <80 no concern, 80–110 mild concern, 111–140 moderate concern, and >140–204 marked concern with shape.27
Lower extremity functional scale (LEFS): The LEFS has 20 questions about a person’s ability to perform everyday tasks especially related to leg function. A perfect score of 80 indicates no impediment to daily activities.28
Lipedema reduction surgery questionnaire: Nonvalidated questionnaire contained 166 questions for self-reporting about lipedema, lifestyle, and how surgery affected these factors.
RESULTS
Demographics
In total, 148 female participants enrolled in our study (Fig. 1); the majority had Stage 2 or 3 lipedema, were White, and aged ~50 years (Table 1). Over half reported hypermobile joints consistent with previous data.29 Except for participants with Stage 1 lipedema, the average body mass index of participants was >30 mg/m2, indicating obesity.
Fig. 1.
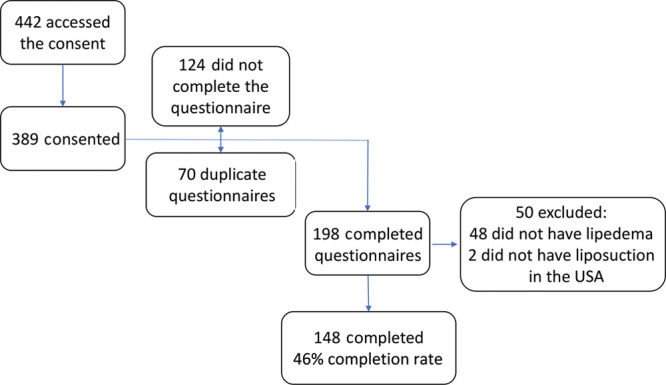
Flowchart of enrollment. Participant responses were not included if they did not consent, did not complete the questionnaire, did not have lipedema, or had lipedema reduction surgery outside of the USA. Completion rate is the number of completed surveys/number of respondents who entered the survey.
Table 1.
Demographics of Participants
| Lipedema Stages | Lipolymphedema | All | |||
|---|---|---|---|---|---|
| 1 | 2 | 3 | |||
| No. female participants | 6 | 71 | 55 | 16 | 148 |
| Race: White/Black/Asian | 5/1/0 | 69/2/0 | 53/2/0 | 14/1/1 | 141/6/1 |
| Ethnicity: Hispanic/not Hispanic | 1/5 | 3/68 | 1/54 | 0/16 | 5/143 |
| Age (y ± SD) | 42 ± 14 | 50 ± 11 | 52 ± 9.4 | 56 ± 9 | 51 ± 11 |
| Height (cm ± SD) | 176 ± 3.6 | 165 ± 4.3 | 165 ± 6.3 | 166 ± 7.6 | 165 ± 5.6 |
| Weight (kg ± SD) | 78 ± 20*† | 85.0 ± 16*† | 105 ± 23 | 120 ± 43 | 96 ± 26.4 |
| Body mass index (kg/m2 ± SD) | 29 ± 6.3*† | 31 ± 6.4*† | 39 ± 8.3 | 43.7 ± 15.8 | 35 ± 9.7 |
| Hypermobile joints (%) | 50 | 52 | 62 | 53 | 56 |
| History of cellulitis (%) | 33 | 16 | 33 | 29 | 24 |
*P < 0.05 versus Stage 3.
†P < 0.05 versus lipolymphedema.
Lipedema LCT Location
Before lipedema reduction surgery, lipedema tissue was notable in specific areas on the body by participants, with the highest percentage of fat on the legs (Fig. 2). Unusually, 20% of the participants reported fat on their feet, as reported previously,21 an area that is thought to be unaffected in lipedema.
Fig. 2.
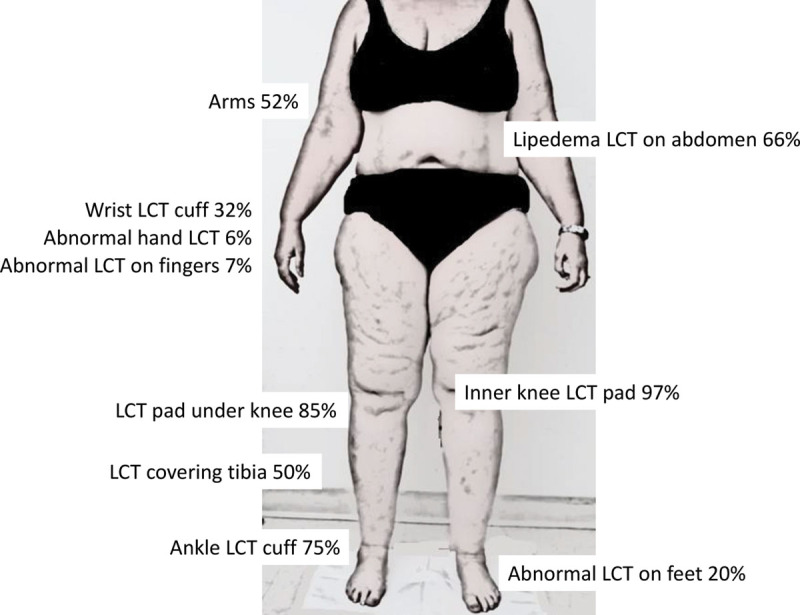
Locations of lipedema tissue in women before lipedema reduction surgery. In addition to affected arms and legs, shown are the percent of 148 women with lipedema tissue in defined areas. Of the 66% of women with lipedema tissue on the abdomen, 3 of the 6 had Stage 1, 40 of the 71 had Stage 2, 42 of the 55 had Stage 3 and 12 of the 16 had lipolymphedema. LCT = loose connective tissue.
Surgeries
Participants had 3.8 ± 2.3 surgeries other than lipedema reduction surgery. Nine individuals had 10 or more surgeries. Of these surgeries, only 13% of the participants underwent weight-loss surgeries such as gastric band, vertical sleeve gastrectomy, or gastric bypass before lipedema reduction surgery.
Participants had an average of 2.4 ± 1.3 lipedema reduction surgeries. The maximum reported by a participant was 6 procedures. While the names of the surgeons remained anonymous in this survey, most liposuction reduction surgery procedures were performed by a plastic or cosmetic surgeon (63%), with the second largest group performed by dermatologists (13.5%) and the third by vascular surgeons (11.5%), all with expertise in lipedema. As part of lipedema reduction surgery, tumescent (61%) or WAL technique (38%) was used; 3 had other procedures. The average number of days after a surgery that subjects completed the questionnaire was 601 ± 1178 days.
PHYSICAL IMPACT OF LIPEDEMA REDUCTION SURGERY PROCEDURE(S)
LCT Pre- and Postlipedema Reduction Surgery
Participants were asked to self-assess areas where they lost lipedema tissue after lipedema reduction surgery. The largest decreases were noted by 44% under the knees, 38% in the ankle cuff, 37% in inner knee fat, and 23% in lower arm fat. Of the 108 women who could not wear boots on their legs before surgery, 71 were able to wear boots postprocedure (66%).
Clothing Size
Dress size significantly decreased 2 sizes (n = 133), pant size significantly decreased 3 sizes (n = 141), and shirt size significantly decreased 1 size (n = 140) after lipedema reduction surgery (Fig. 3).
Fig. 3.
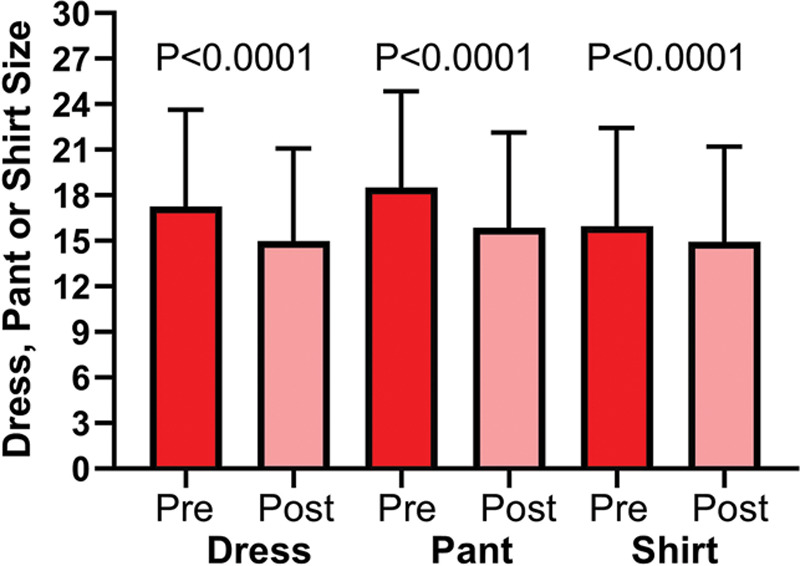
Dress, shirt, and pant sizes of women with lipedema and lipolymphedema pre- and within 1-year postlipedema reduction surgery.
Swelling and Compression
Swelling of LCT was reported by 117 participants before lipedema reduction surgery; 36% stated this swelling resolved after lipedema reduction surgery. Just over half (58%) reported acute swelling postprocedure, which resolved. Almost all women (96 ± 0.2%) used compression garments after surgery, a 33% increase from prelipedema reduction surgery (62 ± 0.5%). About 30% of women without lymphedema were able to stop wearing compression garments within 3 months after their procedure as they no longer felt the need to wear compression or were no longer required to or both.
Pain
A majority of participants (89%) reported pain in their lipedema LCT before lipedema reduction surgery; 86% of these participants reported pain reduction after lipedema reduction surgery (P = 0.018; Fig. 5).
Fig. 5.
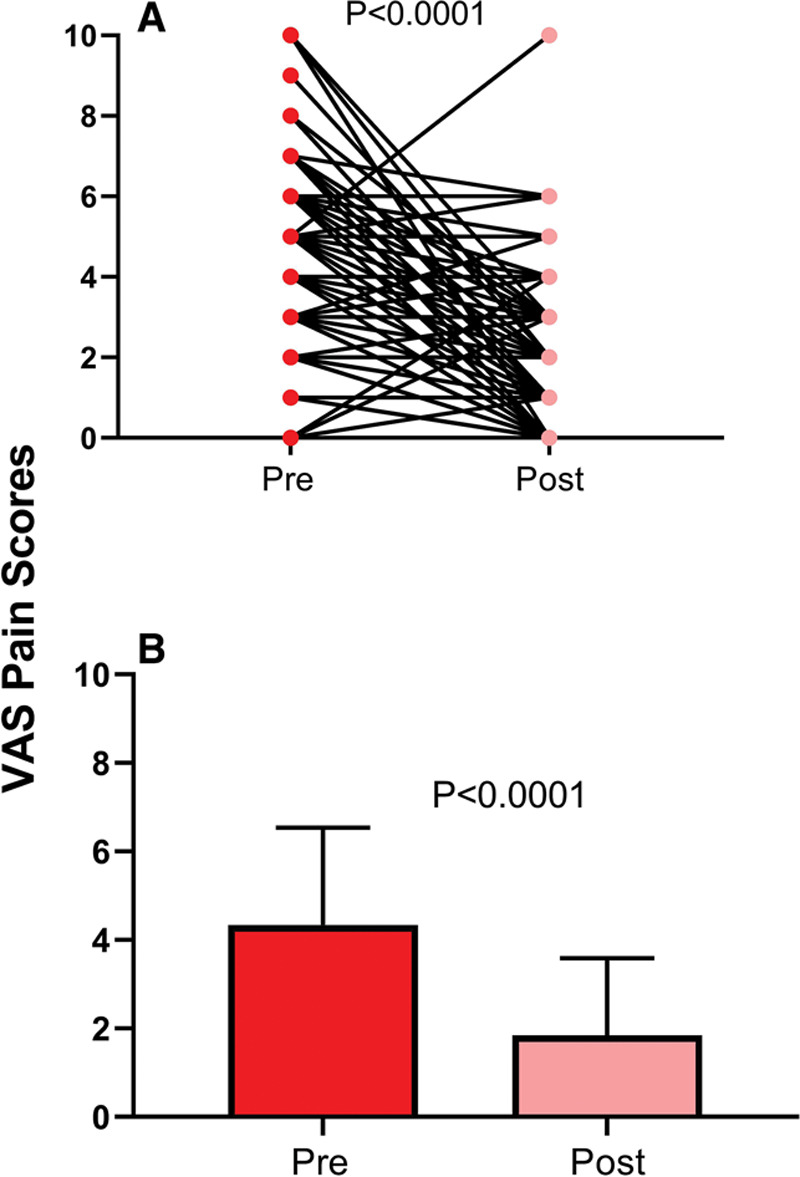
Perceived daily pain scores pre- and postlipedema reduction surgery in women in the USA. Participants rated their daily pain both before and after their lipedema reduction surgery on a scale of 0 to 10: 0 indicating no pain at all and 10 indicating that the pain was excruciating. A, Individual pain scores pre- and postlipedema reduction surgery. B, Average daily pain scores pre- and postlipedema reduction surgery for all participants (n = 148).
Bruising
Easy bruising was reported by 90 ± 30% before lipedema reduction surgery, which decreased to 43 ± 50% postsurgery (P < 0.0001).
Mobility
Participants were asked how lipedema affected walking/mobility; respondents could list more than 1 factor. A majority (81%) of 148 respondents reported walking was negatively affected by lipedema due to increased LCT on the inner knees (72%) or thighs (62%), leg pain (60%), knee arthritis (41%), and/or muscle weakness (36%). Walking improved after lipedema reduction surgery (Fig. 4). In order of benefit, walking improved for women with Stage 3 (96 ± 20%), Stage 2 (88 ± 33%), lipolymphedema (79 ± 43%), and Stage 1 lipedema (33 ± 58%). Most women (82%) were able to return to their regular activities in 1 month or less after surgery. An estimated 11% of women took more than 6 weeks to recover.
Fig. 4.
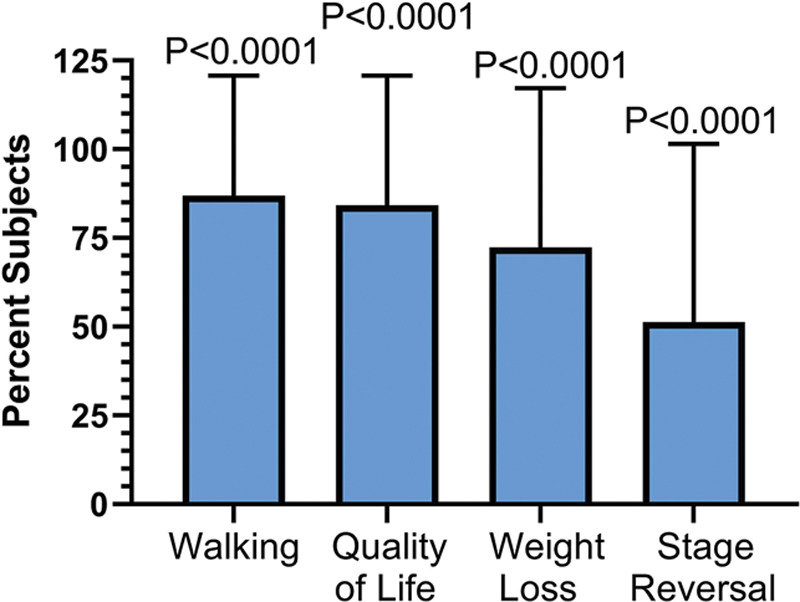
Perceived benefits after lipedema reduction therapy by women with lipedema in the USA. Benefits included improvement in walking, improved quality of life, weight loss, and reversal of stage.
Quality of Life
A majority of participants felt their quality of life improved after lipedema reduction surgery (Fig. 4). In addition, 67 ± 47% felt stronger postprocedure, and 74.7 ± 43.6% indicated they were able to be more physically active postsurgery. When asked about their day-to-day energy levels, 61% indicated their energy level was improved, 30% indicated no change, and 7% felt their energy level was worse after their procedure. Success of the lipedema reduction surgery procedure(s) on a scale of 0 = worst, 50 = same and 100 = best was similar for all stages, with an overall average rating of 72 ± 24.
Weight Loss
Almost two thirds of participants reported weight loss after lipedema reduction surgery (Fig. 4); 54% lost weight within the first 3 months. Weight loss was reported secondary to the procedure in 68% with the remainder noting weight loss from increased physical activity and/or change in diet.
Stage Reversal
About half of the participants felt their lipedema reversed (Fig. 4) by 1 stage (35%) or 2 stages (16%). Of all participants, 11% experienced a total reversal of their lipedema to the point they found no evidence of the disease after lipedema reduction surgery.
Body Image and Emotional Reactions
Most participants (92%) reported feeling their body was misshapen before lipedema reduction surgery; after the procedure, 18% reported feeling their body was in worse shape, and 77% indicated they felt their body was in better shape. Twelve women reported not feeling misshapen before lipedema reduction surgery; of these 12, 3 reported a misshapen body after surgery. Participants were asked to rate self-perception of their body after lipedema reduction surgery compared with before on a scale of 0 to 100: 0 = much worse, 50 = the same, and 100 = much better; the average score was 68 ± 22. Participants were asked to describe how their emotional state was affected by lipedema reduction surgery. The greatest percentage (46%) reported feeling happiness. Depression was noted in 22% after their procedure, and 22% were unsure about their new body.
BSQ-34
Participants completing the BSQ-34 postprocedure had moderate concern about their shape (Fig. 6).
Fig. 6.
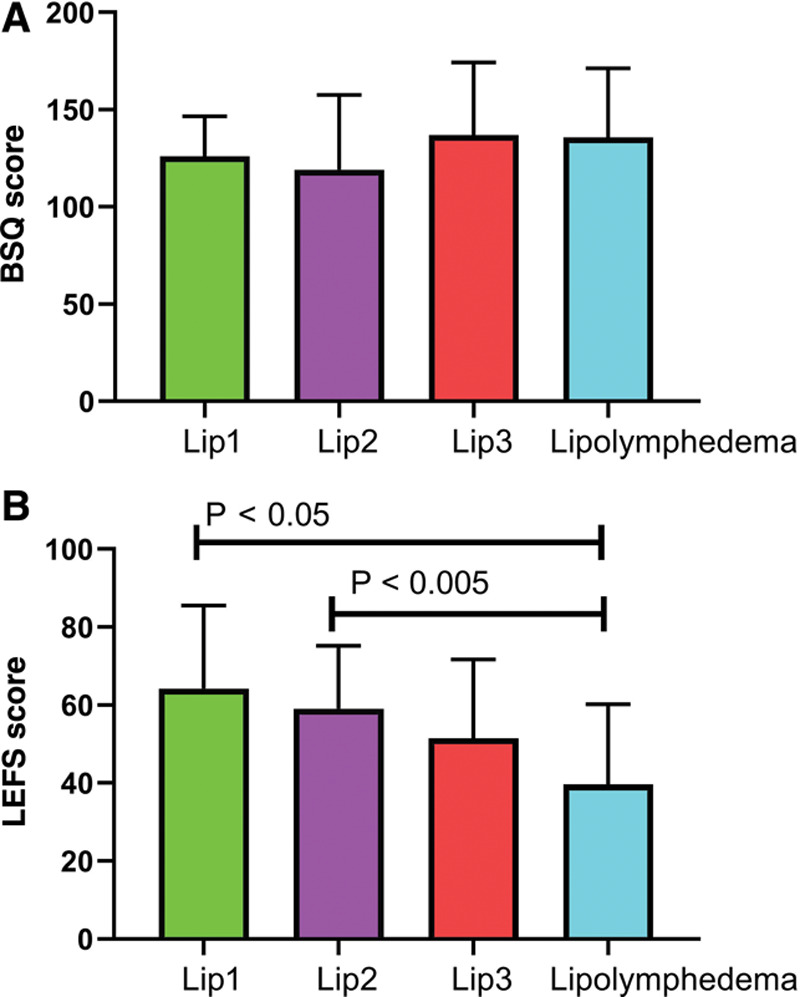
Body shape questionnaire (BSQ) and lower extremity functional scale (LEFS) scores in women who have been treated with lipedema reduction surgery. A, BSQ scores were similar amongst the women. B, LEFS scores were significantly lower in women with lipolymphedema (ANOVA with Tukey’s multiple comparison).
LEFS
Postprocedure, participants with Stage 1 or Stage 2 lipedema scored significantly higher than women with lipolymphedema on the LEFS (Fig. 6). There was a significant inverse relationship between stage or lipolymphedema and LEFS scores (r2 = 0.11; P = 0.0001).
Future Lipedema Reduction Surgery
Eighty-four percent of women reported a desire to have additional lipedema reduction surgery, and 90% indicated that if they were given the chance to have the same lipedema reduction surgery procedure(s) over again, they would.
Surgical Complications
Complications due to lipedema reduction surgery procedures were reported by the participants and included anemia, leg deep venous thrombosis, pulmonary embolus, lymphedema, pneumonia, cellulitis, skin irritation, tissue or skin folds, asymmetry, wrinkles, sagging skin, or the largest percentage of subjects with no complications (Fig. 7).
Fig. 7.
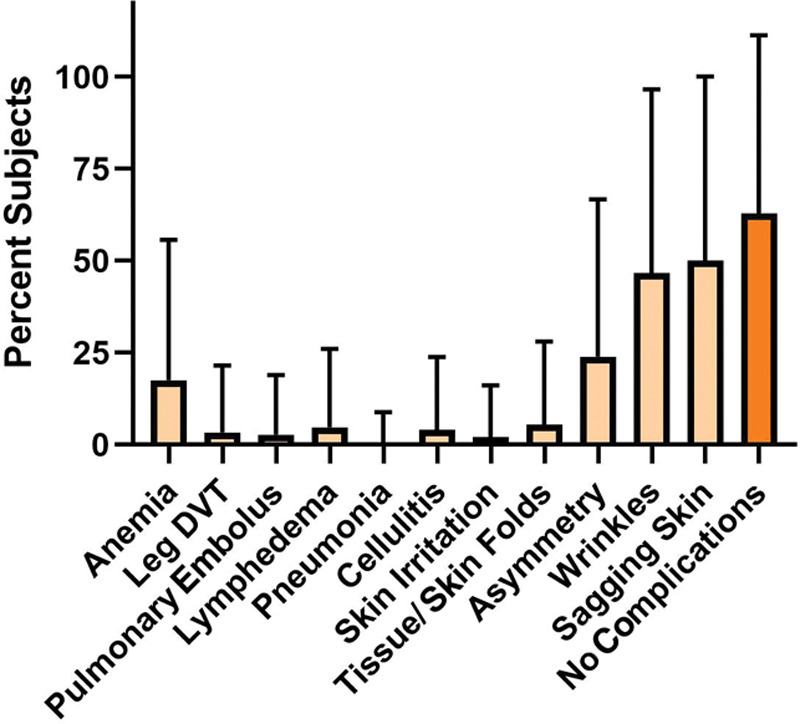
Complications reported by women after lipedema reduction surgery. Anemia, wrinkles, sagging skin, and asymmetry were the most common complications. More than 50% of women did not experience complications. DVT = deep venous thrombosis.
Postsurgical Growth of LCT
Tissue growth after surgery was noted within and outside treated areas (Fig. 8). Regrowth outside of treated areas was found for >50% of women with Stage 2, 3, and lipolymphedema.
Fig. 8.
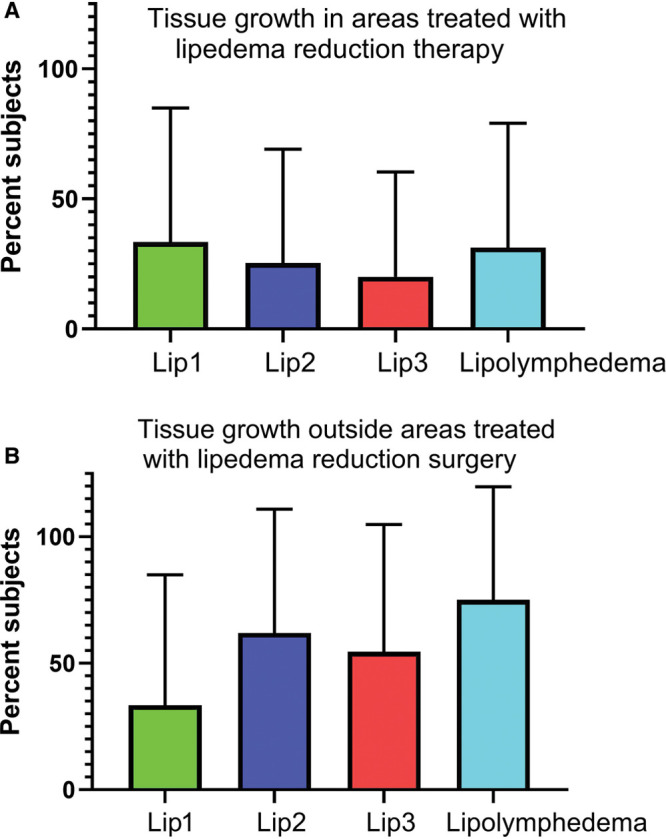
Tissue growth after lipedema reduction surgery. A, Women with lipedema reported growth of tissue in areas that were treated with lipedema reduction surgery. B, Growth of tissue also occurred outside of areas treated with surgery. Over half (61%) noted new tissue growth within the first 6 months.
Fibrosis
Tissue fibrosis is defined as overgrowth, hardening, and/or scarring attributed to excess deposition of extracellular matrix components including collagen in LCT, such as in fat nodules and lipomas.30 Of 148 participants, 86 (58%) noted fibrosis in their fat tissue before lipedema reduction surgery. Participants developed new fibrosis postsurgery in areas treated by lipedema reduction surgery, including new lipomas and pearl-sized nodules (Fig. 9).
Fig. 9.
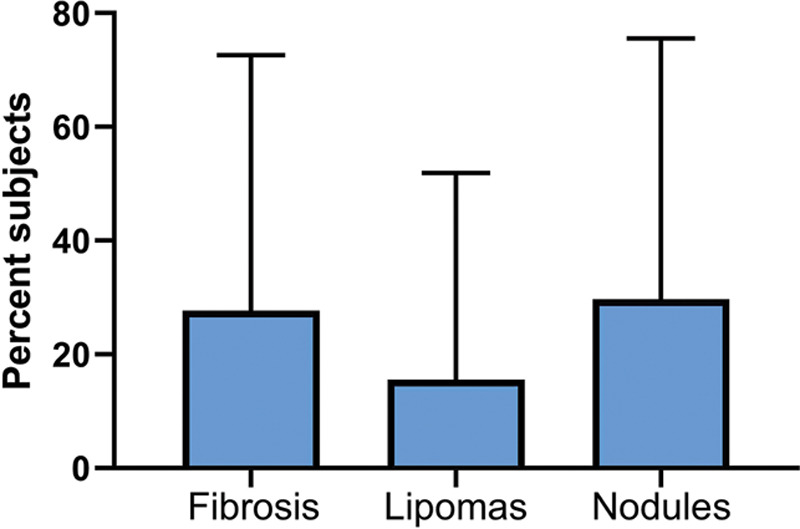
Tissue fibrosis as a complication after lipedema reduction surgery. Fibrosis follows inflammation in tissue. Lipomas and nodules in loose connective tissue in people with lipedema have fibrosis.
Lipolymphedema
Two women with Stage 1 lipedema had lipolymphedema before lipedema reduction surgery; none developed new lymphedema after the procedure. Fourteen women with Stage 2 lipedema had lipolymphedema before lipedema reduction surgery and 5 new women developed lipolymphedema after the procedure. Twenty-two women with Stage 3 lipedema had lymphedema before lipedema reduction surgery; 3 new women developed lipolymphedema postprocedure. Only 4.7% (7 women) felt they developed lipolymphedema due to the surgery.
Loose Skin
Loose skin was reported by 75% of participants after lipedema reduction surgery, a 53% increase from presurgery. Five participants (3.4%) had skin removal surgery after lipedema reduction surgery.
DISCUSSION
Lipedema is a LCT disease likely affecting millions of women in the USA. Symptoms of lipedema range from mild without pain (11% of women in our study), to disabling due to pain, obesity, dysmobility, and lymphedema. There are few treatment options for lipedema other than standard conservative therapy that helps reduce tissue fluid but not lipedema tissue. Bariatric surgery appears to be effective for nonlipedema obesity but not lipedema.3–5 Once standard treatment options have failed to reduce lipedema tissue, lipedema reduction surgery becomes a treatment option.9,31,32 Many publications on lipedema reduction surgery for lipedema are from Germany and indicate improvement in pain and quality of life after liposuction13,15,22; there are currently no published prospective studies in the USA. We conducted a questionnaire study consisting of 3 parts: 2 validated questionnaires, BSQ-34 and LEFS, and a general portion that allowed women to self-report their experience with lipedema reduction surgery. Our data agree that overall, women with lipedema had reduced lipedema tissue, including a reduction in stage, improved quality of life, reduced pain, and perceived benefit from the surgery, including energy level, strength, and the ability to walk (Table 2). This benefit was found for all stages and women with lipolymphedema. Most reported they would undergo lipedema reduction surgery again.
Table 2.
Positive and Negative Outcomes of Lipedema Reduction Surgery Identified by Patients, Postprocedure
| Outcomes | |
|---|---|
| Positive | Negative |
| Improvement in energy level or fatigue | Fat returning or increasing after treatment, including lipomas in treated and nontreated areas |
| Improvement in joint/arthritic pain | Fibrosis |
| Improved mobility | Asymmetrical body proportions |
| Decreased pain levels | Numbness in treated area |
| Improved self-esteem and body image | Recovery interfered with daily life longer than expected |
Some individuals noted lower energy levels, depression, and uncertainty with their bodies after lipedema reduction surgery, which should be investigated further.
Complications after lipedema reduction surgery are rarely reported. Participants in our study reported lymphedema/swelling, blood clots, and anemia (Table 2). Whether participants developed lymphedema due to the procedure, or whether they developed lymphedema over time due to underlying lymphatic dysfunction is unclear. Close and long-term monitoring of patients with lipedema postsurgery is needed to determine the risks of these procedures in the USA.
A concerning outcome of this questionnaire was the number of participants reporting growth of tissue after surgery within and outside treatment areas. Over half of all participants noted growth in new areas, and a quarter saw growth in areas that had been treated. This has not been reported previously for lipedema.
Fat redistribution on the abdomen has been demonstrated by dual x-ray absorptiometry scans after suction lipectomy of the thigh in women with disproportionate tissue on the lower abdomen, hips, or thighs33; it is unclear if any of these women had lipedema. Swanson followed 58 female participants without lipedema who had liposuction or a combination of liposuction and abdominoplasty for 5–19 months post procedure and found no redistribution of fat to the breasts or upper body.34 However, this study was limited by sample size and the use of photographs as a source of upper body measurements. The possibility of regrowth and redistribution of LCT in participants with lipedema has yet to be established. The self-reported data by women with lipedema who participated in our questionnaire highlights the possibility of tissue growth or fat redistribution after surgery. Prospective studies monitoring body composition by bioimpedance spectroscopy, dual x-ray absorptiometry, 3D volume, or other modality are needed pre- and postsurgery. Surgeries should also be carefully described by location on the body, type of surgery, and amount of aspirate to better understand benefits and downsides after lipedema reduction surgery.
A second concerning complication reported by women in the USA after lipedema reduction surgery was the development of fibrosis, including formation of small nodules and lipomas. The development of fibrosis after liposuction has been reported.35–39 Fibrosis is a marker of inflammation which can occur from underlying lymphatic dysfunction. Dadras et al note that fibrosis associated with lipolymphedema is due to edema, characteristic of the disease,24 but is rare if lipolymphedema is not present.40 Our questionnaire study reports that 27.7% of women developed fibrosis, which is much higher than 2.3% reported by Triana et al for 26,259 people undergoing liposuction.39 Triana et al also reported that fibrosis was successfully treated with massage and other techniques.39 Women with lipedema have underlying lymphatic abnormalities even in early stages,8,41 which could increase the risk of development of fibrosis. These data need confirmation in prospective studies where assessment of fibrosis in LCT and skin is evaluated before and after lipedema reduction surgery for lipedema. These data also support the use of therapies such as manual lymphatic drainage and deeper manual and instrument-assisted techniques to reduce the incidence of fibrosis after lipedema reduction surgery.
Compression wear is a standard therapy for lipedema and lipolymphedema care meant to support lymphatic flow and reduce inflammation. Thirty percent of our participants were able to stop wearing compression garments within the first 3 months following lipedema reduction surgery in agreement with published data from Germany.15,17,24Although our data indicate positive results, the information given by the participants was subject to recall bias; for example, some participants had lipedema reduction surgery over 4 years ago. Questions regarding physical changes and frequency that compression was worn, as well as pain, self-image, and mobility ratings are more likely to be affected by this bias. Some participants had trouble recalling weight changes before and after lipedema reduction surgery. Other factors such as cost, and treatment methods (physician, lipedema reduction surgery type, etc.) were less likely to be affected by recall bias. However, this does not mean that they were without error. To offset this, future studies should be prospective and long term.
The applicability of the study was limited by the enrolled participants. Of the 148 participants, only 6 were not White. Future studies should be more inclusive of participants of diverse race and ethnicity. Additionally, different stages of lipedema were underrepresented in this study, with only 6 participants having lipedema Stage 1, and women with lipedema Stage 2 represented nearly half of all participants.
CONCLUSIONS
This retrospective questionnaire study allowed women in the USA to self-report their experience with lipedema reduction surgery. Overall, women with lipedema had improved quality of life with reduced pain, weight and clothing size, and improved ability to walk, but there were concerning complications that need to be addressed in future prospective studies. In addition to pain and quality of life, future studies should monitor lifestyle changes after surgery, weight and body shape, type of surgery, location of surgery, and amount of tissue removed.
ACKNOWLEDGMENT
Thank you to all the women living with lipedema who answered this questionnaire, which could make a difference.
Footnotes
Published online 23 April 2021.
Presented at the 2019 Endocrine Society Meetings, New Orleans, LA.
Disclosure: All the authors have no financial interest in relation to content of this article.This study was funded by the Lipedema Foundation (lipedema.org).
REFERENCES
- 1.Suga H, Araki J, Aoi N, et al. Adipose tissue remodeling in lipedema: adipocyte death and concurrent regeneration. J Cutan Pathol. 2009; 3:3. [DOI] [PubMed] [Google Scholar]
- 2.Felmerer G, Stylianaki A, Hägerling R, et al. Adipose tissue hypertrophy, an aberrant biochemical profile and distinct gene expression in lipedema. J Surg Res. 2020; 253:294–303 [DOI] [PubMed] [Google Scholar]
- 3.Bast JH, Ahmed L, Engdahl R. Lipedema in patients after bariatric surgery. Surg Obes Relat Dis. 2016; 12:1131–1132 [DOI] [PubMed] [Google Scholar]
- 4.Pouwels S, Huisman S, Smelt HJM, et al. Lipoedema in patients after bariatric surgery: report of two cases and review of literature. Clin Obes. 2018; 8:147–150 [DOI] [PubMed] [Google Scholar]
- 5.Pouwels S, Smelt HJ, Said M, et al. Mobility problems and weight regain by misdiagnosed lipoedema after bariatric surgery: illustrating the medical and legal aspects. Cureus. 2019; 11:e5388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chabot K, Gauthier MS, Garneau PY, et al. Evolution of subcutaneous adipose tissue fibrosis after bariatric surgery. Diabetes Metab. 2017; 43:125–133 [DOI] [PubMed] [Google Scholar]
- 7.Bel Lassen P, Charlotte F, Liu Y, et al. The FAT score, a fibrosis score of adipose tissue: predicting weight-loss outcome after gastric bypass. J Clin Endocrinol Metab. 2017; 102:2443–2453 [DOI] [PubMed] [Google Scholar]
- 8.Forner-Cordero I, Oliván-Sasot P, Ruiz-Llorca C, et al. Lymphoscintigraphic findings in patients with lipedema. Rev Esp Med Nucl Imagen Mol. 2018; 37:341–348 [DOI] [PubMed] [Google Scholar]
- 9.Reich-Schupke S, Schmeller W, Brauer WJ, et al. S1 guidelines: lipedema. J Dtsch Dermatol Ges. 2017; 15:758–767 [DOI] [PubMed] [Google Scholar]
- 10.Schook CC, Mulliken JB, Fishman SJ, et al. Differential diagnosis of lower extremity enlargement in pediatric patients referred with a diagnosis of lymphedema. Plast Reconstr Surg. 2011; 127:1571–1581 [DOI] [PubMed] [Google Scholar]
- 11.Herpertz U. Krankheitsspektrum des lipödems an einer lymphologischen fachklinik - erscheinungsformen, mischbilder und behandlungsmöglichkeiten. Vasomed. 1997; ;9:301–307 [Google Scholar]
- 12.Forner-Cordero I, Szolnoky G, Forner-Cordero A, et al. Lipedema: an overview of its clinical manifestations, diagnosis and treatment of the disproportional fatty deposition syndrome - systematic review. Clin Obes. 2012; 2:86–95 [DOI] [PubMed] [Google Scholar]
- 13.Rapprich S, Baum S, Kaak I, et al. Treatment of lipoedema using liposuction. Results of our own surveys. Phlebologie. 2015; 44:121–132 [Google Scholar]
- 14.Sandhofer M, Hanke CW, Habbema L, et al. Prevention of progression of lipedema with liposuction using tumescent local anesthesia: results of an international consensus conference. Dermatol Surg. 2020; 46:220–228 [DOI] [PubMed] [Google Scholar]
- 15.Schmeller W, Hueppe M, Meier-Vollrath I. Tumescent liposuction in lipoedema yields good long-term results. Br J Dermatol. 2012; 166:161–168 [DOI] [PubMed] [Google Scholar]
- 16.Stutz JJ, Krahl D. Water jet-assisted liposuction for patients with lipoedema: histologic and immunohistologic analysis of the aspirates of 30 lipoedema patients. Aesthetic Plast Surg. 2009; 33:153–162 [DOI] [PubMed] [Google Scholar]
- 17.Witte T, Dadras M, Heck FC, et al. Water-jet-assisted liposuction for the treatment of lipedema: standardized treatment protocol and results of 63 patients [published online ahead of print, 2020 Mar 14]. J Plastic Reconstr Aesthet Surg. 2020; 73:1634–1644 [DOI] [PubMed] [Google Scholar]
- 18.Wollina U, Heinig B, Nowak A. Treatment of elderly patients with advanced lipedema: a combination of laser-assisted liposuction, medial thigh lift, and lower partial abdominoplasty. Clin Cosmet Investig Dermatol. 2014; 7:35–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wold LE, Hines EA, Jr, Allen EV. Lipedema of the legs; a syndrome characterized by fat legs and edema. Ann Intern Med. 1951; 34:1243–1250 [DOI] [PubMed] [Google Scholar]
- 20.Sandhofer M, Schauer P, Sandhofer M, et al. Lipödem. Journal für Ästhetische Chirurgie. 2017; 10:61–70 [Google Scholar]
- 21.Herbst K, Mirkovskaya L, Bharhagava A, et al. Lipedema fat and signs and symptoms of illness, increase with advancing stage. Archive Med. 2015; 7:1–8 [Google Scholar]
- 22.Rapprich S, Dingler A, Podda M. Liposuction is an effective treatment for lipedema-results of a study with 25 patients. J Dtsch Dermatol Ges. 2011; 9:33–40 [DOI] [PubMed] [Google Scholar]
- 23.Wollina U, Heinig B. Treatment of lipedema by low-volume micro-cannular liposuction in tumescent anesthesia: results in 111 patients. Dermatol Ther. 2019; 32:e12820. [DOI] [PubMed] [Google Scholar]
- 24.Dadras M, Mallinger PJ, Corterier CC, et al. Liposuction in the treatment of lipedema: a longitudinal study. Arch Plast Surg. 2017; 44:324–331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Baumgartner A, Hueppe M, Meier-Vollrath I, et al. Improvements in patients with lipedema 4, 8 and 12 years after liposuction. Phlebology. 2020; 26:152–159 [DOI] [PubMed] [Google Scholar]
- 26.Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)–a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009; 42:377–381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Taylor MJ. The Nature and Significance of Body Image Disturbance. 1987Cambridge, UK: Wolfson College, University of Cambridge [Google Scholar]
- 28.Binkley JM, Stratford PW, Lott SA, et al. The lower extremity functional scale (LEFS): scale development, measurement properties, and clinical application. North American Orthopaedic Rehabilitation Research Network. Phys Ther. 1999; 79:371–383 [PubMed] [Google Scholar]
- 29.Beltran K, Herbst KL. Differentiating lipedema and Dercum’s disease. Int J Obes (Lond). 2017; 41:240–245 [DOI] [PubMed] [Google Scholar]
- 30.Wynn TA. Cellular and molecular mechanisms of fibrosis. J Pathol. 2008; 214:199–210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Halk AB, Damstra RJ. First Dutch guidelines on lipedema using the international classification of functioning, disability and health. Phlebology. 2017; 32:152–159 [DOI] [PubMed] [Google Scholar]
- 32.Coppel T, Cunneen J, Fetzer S, et al. Best practice guidelines: the management of lipoedema. Wounds UK. 2017; 13:1–13. Available at: http://www.wounds-uk.com/best-practice-statements/best-practice-guidelines-the-management-of-lipoedema [Google Scholar]
- 33.Hernandez TL, Kittelson JM, Law CK, et al. Fat redistribution following suction lipectomy: defense of body fat and patterns of restoration. Obesity (Silver Spring). 2011; 19:1388–1395 [DOI] [PubMed] [Google Scholar]
- 34.Swanson E. No increase in female breast size or fat redistribution to the upper body after liposuction: a prospective controlled photometric study. Aesthet Surg J. 2014; 34:896–906 [DOI] [PubMed] [Google Scholar]
- 35.Illouz YG. Complications of liposuction. Clin Plast Surg. 2006; 33:129–163, viii [DOI] [PubMed] [Google Scholar]
- 36.Shiffman MA. Shiffman MA, Di Giuseppe A. Prevention and treatment of liposuction complications. Liposuction – Principles and Practice. 2006, New York: Springer, 333–341 [Google Scholar]
- 37.Toledo LS, Mauad R. Complications of body sculpture: prevention and treatment. Clin Plast Surg. 2006; 33:1–11, v [DOI] [PubMed] [Google Scholar]
- 38.Chacur R, Menezes HS, Chacur NMBDS, et al. Aesthetic correction of lesion by post-liposuction corticoid infiltration using subcision, PMMA filling, and CO2 laser. Case Reports Plast Surg Hand Surg. 2019; 6:140–144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Triana L, Triana C, Barbato C, et al. Liposuction: 25 years of experience in 26,259 patients using different devices. Aesthet Surg J. 2009; 29:509–512 [DOI] [PubMed] [Google Scholar]
- 40.Shin BW, Sim YJ, Jeong HJ, et al. Lipedema, a rare disease. Ann Rehabil Med. 2011; 35:922–927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Amann-Vesti BR, Franzeck UK, Bollinger A. Microlymphatic aneurysms in patients with lipedema. Lymphology. 2001; 34:170–175 [PubMed] [Google Scholar]


