Graphical Abstract
 Listen to the podcast associated with this article, which can also be found at ESC CardioTalk https://www.escardio.org/The-ESC/Whatwe-do/news/ESC-Cardio-Talk
Listen to the podcast associated with this article, which can also be found at ESC CardioTalk https://www.escardio.org/The-ESC/Whatwe-do/news/ESC-Cardio-Talk
This editorial refers to ‘C-reactive protein and clinical outcomes in patients with COVID-19’†, by N.R. Smilowitz et al., on page 2270.
C-reactive protein (CRP) has an illustrious scientific ‘parentage’. The laboratory of Oswald Avery, who first demonstrated unequivocally that DNA is the genetic material, also characterized CRP as a protein with calcium-dependent binding to pneumococcal somatic C-polysaccharide. In addition, he introduced the term ‘acute phase’ for serum containing CRP from patients acutely ill with infectious disease.1,2 The early, insensitive, semi-quantitative tests for CRP established it as a marker of infections, inflammatory, ischaemic, and traumatic tissue injuries, and malignancy, whilst the advent of sensitive quantitative immunoassays in the 1970s greatly enhanced its clinical utility.
C-polysaccharide is a phosphocholine-substituted ribitol teichoic acid and, in 1971, Volanakis and Kaplan identified phosphocholine as the structure to which CRP binds.3 Indeed, phosphocholine residues are the natural ligand bound with highest affinity by CRP. In 1974, Kaplan and Volanakis4 and Siegel et al.5 independently reported that CRP bound to C-polysaccharide and other ligands, and activated the classical complement pathway, and showed that CRP was thereby capable of mediating inflammation. In fact, Francis and Abernethy6 had already shown in 1934 that intracutaneous injection of C-polysaccharide in acutely ill patients elicited a characteristic immediate weal-and-flare reaction, followed by a more extensive oedematous erythema maximal at 6–10 h. These reactions only occurred when CRP was detectable in the patient’s serum.
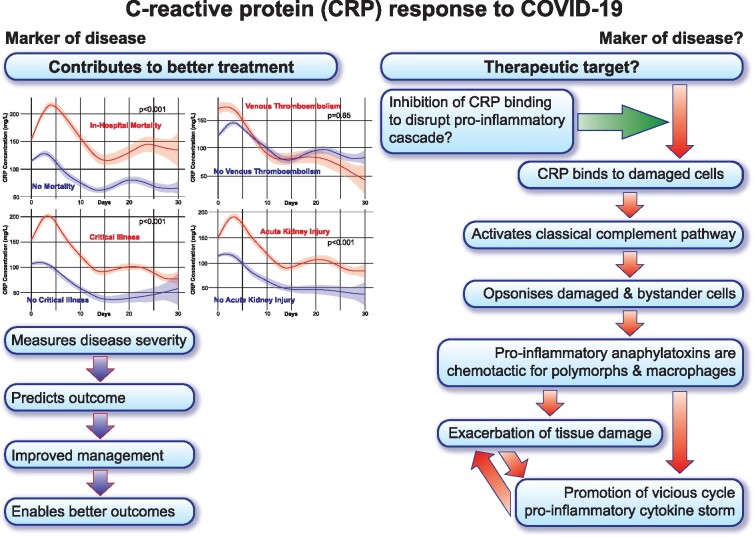
Reviewing the CRP field in 19817 and again in 2003,8 I was able to show the range of clinical applications of CRP measurements and to hypothesize about a pathophysiological role for CRP (Graphical Abstract). Sensitive quantitative clinical measurement of CRP has three different roles: (i) as a sensitive screening test for an active inflammatory or tissue-damaging process; (ii) to monitor the activity, extent, and response to treatment of any disease process that triggers an acute phase response; and (iii) among the small number of disease processes, such as systemic lupus erythematosus and leukaemia, that themselves stimulate little or no acute phase response, CRP is a very sensitive and useful marker of intercurrent microbial infection. The exemplary study of CRP in coronavirus disease 2019 (COVID-19) by Smilowitz et al.9 in this issue of the European Heart Journal illustrates the value of CRP for monitoring and prognosis in a most challenging clinical situation (Graphical Abstract).
C-reactive protein (CRP) response to COVID-19.
The universal application of their actual CRP values is underpinned by the robust standardization of clinical CRP assays. The automation of clinical chemistry CRP immunoassays in the early 1980s, and resulting major expansion of CRP testing, had mandated robust reference standards. The World Health Organization therefore invited me to create and validate the International Standard for Human C-reactive protein, 85/506, on which gold standard all commercial clinical CRP assays have subsequently been based. The International Federation of Clinical Chemistry and Laboratory Medicine and the European Union secondary serum standards were also constructed using CRP that I isolated.
The major acute phase response of CRP in COVID-19 was predictable, based on the known behaviour of CRP in general and particularly in severe viral respiratory infections. From the outset, CRP values were found to reflect the severity of COVID-19 and to predict outcome, as reported in many, mostly small, series published worldwide. However, the present report by Smilowitz et al.9 is distinguished by its large scale, its analysis in relation to more of the major clinical consequences of severe COVID-19, its highlighting of the additive value with D-dimer measurements, and its robust demonstration of prognostic significance. All of these crucial insights will increase in importance as new and effective therapeutic interventions become available, whether directly antiviral or targeting host responses.
What more can be done to exploit for patient benefit the remarkable properties of CRP as a marker of COVID-19 disease activity, extent, and severity? The most obvious is to measure its concentration serially and very frequently. The plasma half-life of CRP is just ∼19 h and is constant, regardless of any pathological processes present.10 Circulating CRP concentration is determined only by its hepatic synthesis rate and, in most conditions, the plasma CRP value very closely reflects the prevailing disease severity. Routine, frequent, serial CRP values, rather than just the admission value and a few other sporadic measurements, combined with critical measures of disease activity and therapeutic interventions, should provide for more granular CRP-based prognostic modelling, potentially leading to more effective management.
Progress on CRP as a potential therapeutic target in human disease has lagged behind universal routine clinical CRP measurement. The compelling association of higher CRP values with disease severity in many different conditions, and the presence of CRP co-localized with activated complement in damaged tissues, stimulated years of speculation about the pathogenicity of CRP; see, for example, Francis and Abernethy7 and Griselli et al.11 However, the first direct experimental evidence of exacerbation of tissue damage by CRP came from the rat acute myocardial infarction model.11 Administration of human CRP after ligating the coronary artery substantially increased infarct size; human CRP was bound to the injured myocardium, activating rat complement, and the adverse effect was completely inhibited by depletion of circulating rat C3, i.e. the pathogenicity of the human CRP was absolutely complement dependent. We then rationally designed bis(phosphocholine)hexane, a new chemical entity, as the first small molecule inhibitor of CRP binding to ligands specifically exposed on damaged but not on healthy cells in vivo.12 Administration of the inhibitor completely abolished the increased infarct size produced by human CRP in the rat model.12 The pathogenicity of CRP has been independently confirmed in different models and inhibited by using antisense oligonucleotide to reduce CRP synthesis13 or apheresis to remove CRP from the circulation.14 Apheresis, pioneered by Pentracor GmbH (https://en.pentracor.de/) using an extracorporeal column of immobilized phosphocholine to absorb CRP from the circulation, is approved for routine clinical use in Germany. The procedure reduces circulating CRP by ∼60% over a couple of days, and unpublished results apparently show significantly reduced infarct size in ST-elevation myocardial infarction patients compared with matched controls. This clinical evidence that CRP contributes to infarct size in humans is fully consistent with the effects of CRP inhibition we originally demonstrated in the rat model.
Following our original report of the predictive significance of CRP and serum amyloid A protein measurement in acute coronary syndrome,15 there was intense cardiological interest in CRP, producing much controversial, confusing, and misleading literature. The early observational epidemiology studies, based on a limited number of events despite large population sizes, exaggerated the significance of the association between increased baseline CRP values and cardiovascular disease risk. The conflation of association with causality popularized the idea that CRP was a risk factor for cardiovascular disease, not just a possible risk marker, and this misconception became widespread despite the general agreement that, for example, the cock crowing before dawn is not actually what causes the sun to rise. The misapprehension was strengthened by poorly conducted and uncontrolled experimental work purporting, falsely, to show that CRP is an inherently proinflammatory mediator of atherosclerosis; see, for example, Pepys.16
In fact, the predictive association between baseline CRP and cardiovascular disease risk in general populations is modest.17,18 It is shared equally by other markers of inflammation such as fibrinogen, plasma viscosity, erythrocyte sedimentation rate (ESR), albumin, and white cell count, and reflects the fact that most of the proven causal risk factors for cardiovascular disease, including obesity, metabolic syndrome and type 2 diabetes, hypertension, smoking, lack of exercise, low socioeconomic status, and chronic low grade inflammatory conditions, are all associated with low grade systemic inflammation and modestly increased baseline CRP values. Even the very limited clinical utility of CRP measurement for cardiovascular disease risk is likely to be outweighed if increased CRP values are used by cardiologists exclusively for this purpose and not considered in the whole-patient context. This risks missing serious underlying diseases. On the other hand, full investigation before CRP testing has been repeated, to ensure that a raised value is persistent, will often reveal nothing but will incur large costs and provoke much spurious anxiety. Clinical CRP testing must be done and interpreted properly.8
Similarly, amidst the plethora of claims and assertions about proinflammatory effects attributed to CRP but actually caused by contaminants in the CRP preparations, it is crucial to focus on the overwhelming negative observations made when rigorously characterized, pure, isolated human CRP is tested. Such pure CRP is not proinflammatory for human cells in vitro, in mice in vivo, or when infused into normal healthy young adult humans.16,19–21 Extensive transgenic animal studies also show that human CRP is either atheroprotective in vivo or has no effect. Most importantly, the compellingly negative large-scale Mendelian randomization studies confirm that CRP does not cause clinical cardiovascular disease events.22 Critically, this must be distinguished from the adverse effects of CRP once an atherothrombotic, or other tissue-damaging, event has occurred, engendering a very different pathobiological environment.
Finally, what about CRP as a therapeutic target in COVID-19? Tissue damage by CRP involves binding of CRP to phosphocholine residues, and potentially other cellular and tissue structures, that are abnormally exposed only on damaged and dead cells. The phosphocholine head group of cellular membrane phospholipids is not accessible in the plasma membrane of normal healthy cells but, when cells are damaged and die, increased abundance of lysophosphatidylcholine and disruption of the lipid bilayer expose phosphocholine residues to which CRP avidly binds.23 Bound CRP then activates complement via C1q and the classical complement pathway, leading to activation of C3, the central and most abundant complement component. Release of the chemotactic anaphylatoxic C3a fragment and fixation of the C3b opsonin are proinflammatory and engage potentially destructive polymorphs and monocyte/macrophages. Complement is necessary for CRP to exert its pathogenic effects in all experimental models in which it has been tested, and there is abundant evidence that this mechanism operates in human diseases. CRP and co-localized activated complement are universally present in the lesions of such disparate conditions as, for example, acute myocardial infarction, rheumatoid arthritis, and influenza virus infection. However, presence at the scene of a crime does not establish guilt. Indeed, CRP and complement might just be facilitating clearance of debris by phagocytic cells. On the other hand, the close positive association between CRP values and severity of tissue damage in many different pathologies, notably including COVID-19 as illustrated by Smilowitz et al., is equally consistent with a pathogenic role for CRP.
Nevertheless, even the strongest associations do not establish causality, and robust validation of CRP as a therapeutic target requires a specific intervention, selectively targeting the proposed pathogenic mechanism. This has been achieved in the rat acute myocardial infarction model, where either C3 depletion11 or bis(phosphocholine)hexane12 completely abrogated the adverse effects of human CRP. Similarly, bis(phosphocholine)hexane treatment of mice infected with virulent avian influenza A markedly reduced morbidity and mortality.24 The presence of CRP in the lesions of COVID-19 has not yet been reported but, given the extensive cell damage and the abundance of circulating CRP, it must be present. CRP bound to damaged tissues, injured by the virus and/or by the host response, will activate complement locally, potentially exacerbating the injury as well as contributing to systemic complement activation. Development of a novel small molecule drug that inhibits CRP binding in vivo is currently in progress to test whether this CRP–complement mechanism contributes significantly to severity of COVID-19 and other diseases (https://apollotherapeutics.com).
Conflict of interest: none declared.
Footnotes
† doi:10.1093/eurheartj/ehaa1103.
The opinions expressed in this article are not necessarily those of the Editors of the European Heart Journal or of the European Society of Cardiology.
References
- 1. Abernethy TJ, Avery OT.. The occurrence during acute infections of a protein not normally present in the blood. I. Distribution of the reactive protein in patient’s sera and the effect of calcium on the flocculation reaction with C polysaccharide of pneumococcus. J Exp Med 1941;73:173–182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Macleod CM, Avery OT.. The occurrence during acute infections of a protein not normally present in the blood. II. Isolation and properties of the reactive protein. J Exp Med 1941;73:183–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Volanakis JE, Kaplan MH.. Specificity of C-reactive protein for choline phosphate residues of pneumococcal C-polysaccharide. Proc Soc Exp Biol Med 1971;136:612–614. [DOI] [PubMed] [Google Scholar]
- 4. Kaplan MH, Volanakis JE.. Interaction of C-reactive protein complexes with the complement system. I. Consumption of human complement associated with the reaction of C-reactive protein with pneumococcal C-polysaccharide and with the choline phosphatides, lecithin and sphingomyelin. J Immunol 1974;112:2135–2147. [PubMed] [Google Scholar]
- 5. Siegel J, Rent R, Gewurz H.. Interactions of C-reactive protein with the complement system. I. Protamine-induced consumption of complement in acute phase sera. J Exp Med 1974;140:631–647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Francis T, Abernethy TJ.. Cutaneous reactions in pneumonia to the somatic (‘C’) polysaccharide of pneumococcus. J Clin Invest 1934;13:692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Pepys MB. C-reactive protein fifty years on. Lancet 1981;i:653–656. [DOI] [PubMed] [Google Scholar]
- 8. Pepys MB, Hirschfield GM.. C-reactive protein: a critical update. J Clin Invest 2003;111:1805–1812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Smilowitz NR, Kunichoff D, Garshick M, Shah B, Pillinger M, Hochman JS, Berger JS.. C-reactive protein and clinical outcomes in patients with COVID-19. Eur Heart J 2021;42:2270–2279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Vigushin DM, Pepys MB, Hawkins PN.. Metabolic and scintigraphic studies of radioiodinated human C-reactive protein in health and disease. J Clin Invest 1993;91:1351–1357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Griselli M, Herbert J, Hutchinson WL, Taylor KM, Sohail M, Krausz T, Pepys MB.. C-reactive protein and complement are important mediators of tissue damage in acute myocardial infarction. J Exp Med 1999;190:1733–1739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Pepys MB, Hirschfield GM, Tennent GA, Gallimore JR, Kahan MC, Bellotti V, Hawkins PN, Myers RM, Smith MD, Polara A, Cobb AJ, Ley SV, Aquilina JA, Robinson CV, Sharif I, Gray GA, Sabin CA, Jenvey MC, Kolstoe SE, Thompson D, Wood SP.. Targeting C-reactive protein for the treatment of cardiovascular disease. Nature 2006;440:1217–1221. [DOI] [PubMed] [Google Scholar]
- 13. Szalai AJ, McCrory MA, Xing D, Hage FG, Miller A, Oparil S, Chen YF, Mazzone M, Early R, Henry SP, Zanardi TA, Graham MJ, Crooke RM.. Inhibiting C-reactive protein for the treatment of cardiovascular disease: promising evidence from rodent models. Mediators Inflamm 2014;2014:353614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Sheriff A, Schindler R, Vogt B, Abdel-Aty H, Unger JK, Bock C, ebauer F, Slagman A, Jerichow T, Mans D, Yapici G, Janelt G, Schröder M, Kunze R, Möckel M.. Selective apheresis of C-reactive protein: a new therapeutic option in myocardial infarction? J Clin Apher 2015;30:15–21. [DOI] [PubMed] [Google Scholar]
- 15. Liuzzo G, Biasucci LM, Gallimore JR, Grillo RL, Rebuzzi AG, Pepys MB, Maseri A.. The prognostic value of C-reactive protein and serum amyloid A protein in severe unstable angina. N Engl J Med 1994;331:417–424. [DOI] [PubMed] [Google Scholar]
- 16. Pepys MB. CRP or not CRP? That is the question. Arterioscler Thromb Vasc Biol 2005;25:1091–1094. [DOI] [PubMed] [Google Scholar]
- 17.Emerging Risk Factors Collaboration, Kaptoge S, Di Angelantonio E, Lowe G, Pepys MB, Thompson SG, Collins R, Danesh J.. C-reactive protein concentration and risk of coronary heart disease, stroke, and mortality: an individual participant meta-analysis. Lancet 2010;375:132–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Emerging Risk Factors Collaboration, Kaptoge S, Di Angelantonio E, Pennells L, Wood AM, White IR, Gao P, Walker M, Thompson A, Sarwar N, Caslake M, Butterworth AS, Amouyel P, Assmann G, Bakker SJ, Barr EL, Barrett-Connor E, Benjamin EJ, Björkelund C, Brenner H, Brunner E, Clarke R, Cooper JA, Cremer P, Cushman M, Dagenais GR, D'Agostino RB Sr, Dankner R, Davey-Smith G, Deeg D, Dekker JM, Engström G, Folsom AR, Fowkes FG, Gallacher J, Gaziano JM, Giampaoli S, Gillum RF, Hofman A, Howard BV, Ingelsson E, Iso H, Jørgensen T, Kiechl S, Kitamura A, Kiyohara Y, Koenig W, Kromhout D, Kuller LH, Lawlor DA, Meade TW, Nissinen A, Nordestgaard BG, Onat A, Panagiotakos DB, Psaty BM, Rodriguez B, Rosengren A, Salomaa V, Kauhanen J, Salonen JT, Shaffer JA, Shea S, Ford I, Stehouwer CD, Strandberg TE, Tipping RW, Tosetto A, Wassertheil-Smoller S, Wennberg P, Westendorp RG, Whincup PH, Wilhelmsen L, Woodward M, Lowe GD, Wareham NJ, Khaw KT, Sattar N, Packard CJ, Gudnason V, Ridker PM, Pepys MB, Thompson SG, Danesh J.. C-reactive protein, fibrinogen, and cardiovascular disease prediction. N Engl J Med 2012;367:1310–1320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Pepys MB, Hawkins PN, Kahan MC, Tennent GA, Gallimore JR, Graham D, Sabin CA, Zychlinsky A, de Diego J.. Proinflammatory effects of bacterial recombinant human C-reactive protein are caused by contamination with bacterial products, not by C-reactive protein itself. Circ Res 2005;97:e97–e103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Pepys MB, Gallimore JR, Lloyd J, Li Z, Graham D, Taylor GW, Ellmerich S, Mangione PP, Tennent GA, Hutchinson WL, Millar DJ, Bennett G, More J, Evans D, Mistry Y, Poole S, Hawkins PN.. Isolation and characterization of pharmaceutical grade human pentraxins, serum amyloid P component and C-reactive protein, for clinical use. J Immunol Methods 2012;384:92–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Lane T, Wassef N, Poole S, Mistry Y, Lachmann HJ, Gillmore JD, Hawkins PN, Pepys MB.. Infusion of pharmaceutical-grade natural human C-reactive protein is not pro-inflammatory in healthy adult human volunteers. Circ Res 2014;114:672–676. [DOI] [PubMed] [Google Scholar]
- 22.C-reactive Protein Coronary Heart Disease Genetics Collaboration, Wensley F, Gao P, Burgess S, Kaptoge S, Di Angelantonio E, Shah T, Engert JC, Clarke R, Davey-Smith G, Nordestgaard BG, Saleheen D, Samani NJ, Sandhu M, Anand S, Pepys MB, Smeeth L, Whittaker J, Casas JP, Thompson SG, Hingorani AD, Danesh J.. Is C-reactive protein causally relevant to coronary disease? Mendelian randomisation analysis based on individual participant data. BMJ 2011;342:d548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Volanakis JE, Narkates AJ.. Interaction of C-reactive protein with artificial phosphatidyl-choline bilayers and complement. J Immunol 1981;126:1820–1825. [PubMed] [Google Scholar]
- 24. Gao R, Wang L, Bai T, Zhang Y, Bo H, Shu Y.. C-reactive protein mediating immunopathological lesions: a potential treatment option for severe influenza A diseases. EBioMedicine 2017;22:133–142. [DOI] [PMC free article] [PubMed] [Google Scholar]