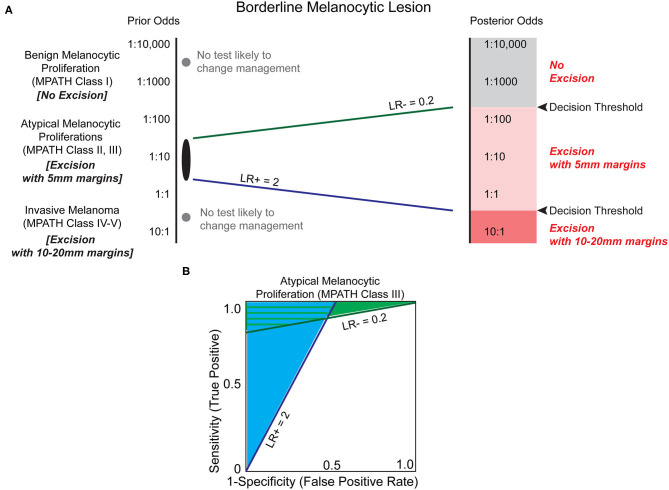
Figure 4.
Biomarkers have the potential to clarify the risk of melanoma in the histopathologic interpretation of borderline pigmented lesions. (A) Melanocytic lesions exist on a histologic spectrum from benign-appearing to malignant. At the extremes of this spectrum (e.g., unambiguous benign melanocytic nevus (MPATH-Dx class I) or unambiguous invasive melanoma (MPATH-Dx class IV-V) no biomarker test is likely to change management (gray dots, Table 1). For borderline melanocytic lesions, especially MPATH-Dx class II-III lesions, pathologists are generally conservative and recommend excision of ambiguous lesions that may have no malignant potential to avoid potential adverse consequences of underdiagnosis (36). This results in excision using 5 mm margins of many atypical and dysplastic melanocytic lesions without full knowledge of malignant potential. A LR– of 0.2, corresponding to a 5-fold reduction in estimated malignant potential, may be sufficient to avoid a recommendation of excision in a more benign-appearing atypical/dysplastic specimen if threshold for treatment is set at ~1:200. At the more dysplastic end of the spectrum, a biomarker test with LR+ of 2 may be sufficient to increase recommendation from excision with 5 mm margins to excision with 10 mm margins. This results in a significant increase in size of total excision and repair that is commensurate with the higher estimated increased risk of malignancy. Due to the inherently ambiguous nature of MPATH-Dx class II–III lesions, it is challenging to estimate the decision thresholds for treatment. Depending on the pathologist's level of suspicion and the clinician's threshold for intervention (which may be influenced by patient specific-factors including prior odds and morbidity of procedure), different LR values are almost certainly necessary to justify changing intervention, such as deferring excision or increasing excision margins. (B) The estimated minimum necessary likelihood ratios indicate that there is a significant range of biomarker characteristics that provide clinical utility in deferring excision (light green shaded area) and/or increasing excision margins (light blue shaded area).