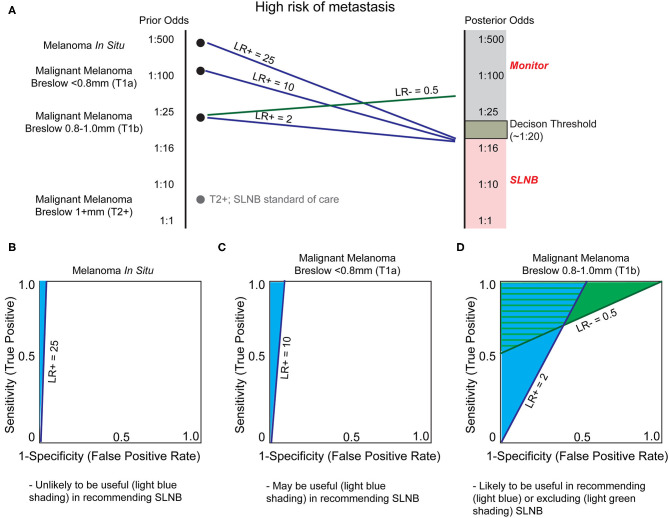
Figure 5.
Utility of biomarkers to augment Breslow depth in determining which patients are offered sentinel lymph node biopsy (SLNB). (A) As depth of melanoma increases, from in situ to greater than one millimeter, the probability of sentinel lymph node positivity, and thereby stage and treatment selection, increases. Sentinel lymph node biopsy (SLNB) is positive in ~5% of patients with T1b melanoma, resulting in a decision threshold posterior odds of ~1:20 for many surgical oncologists to offer SLNB and reflecting NCCN guideline recommendations (90). As SLNB is not routinely offered for melanoma in situ or T1a melanomas, the incidence of SLNB positivity is unknown. We therefore estimate that these are substantially and progressively less positive as tumor thickness decreases. SLNB is standard of care for T2+ melanomas (gray dot) and thus no biomarker is likely to alter this recommendation without exceptionally low LR- test characteristics. (B) Currently patients with melanoma in situ are not generally offered SLNB since the likelihood of positivity (prior odds) is very low. A very high LR+, estimated at 25, would be necessary to recommend SLNB. (C) As the melanoma Breslow depth increases, the prior odds of sentinel lymph node metastasis increases (becomes closer to 1:1). Therefore, a lower LR+, such as LR+ ≥10, would be necessary to prompt SLNB. (D) Biomarkers may have the greatest utility for T1b malignant melanomas. Current NCCN guidelines recommend thoughtful consideration of SLNB based on patient-specific factors, and any test that could offer relatively small changes in certainty could be of great clinical utility. Thus, a modest LR+ of 2.0 or LR– of 0.5 may be sufficient for a clinically-actionable biomarker.