Abstract
Objective
To evaluate the reproducibility of digital tray transfer fit on digital indirect bonding by analyzing the differences in bracket positions.
Materials and Methods
Digital indirect bonding was performed by positioning brackets on digital models superimposed by tomography using Ortho Analyzer (3Shape) software. Thirty-three orthodontists performed indirect bonding on prototyped models of the same malocclusion using prototyped transfer trays for two types of brackets (MiniSprint Roth and BioQuick self-ligating). The models with brackets were scanned using an intraoral scanner (Trios, 3Shape). Superimpositions were made between the digital models obtained after indirect bonding and those from the original virtual setup. To analyze the differences in bracket positions, three planes were examined for each bracket: vertical, horizontal, and angulation. Three orthodontists repeated indirect bonding after 15 days, and Bland-Altman plots and intraclass correlation coefficients were used to evaluate inter- and intraevaluator reproducibility and reliability, respectively. Repeated-measures analysis of variance (ANOVA) was used to analyze the differences between bracket positions, and multivariate ANOVA was used to evaluate the influence of orthodontists' experience on the results.
Results
Differences between bracket positions were not statistically significant, except mesial-distal discrepancies in the BioQuick group (P = .016). However, differences were not clinically significant (horizontal varied from 0.04 to 0.13 mm; angulation, 0.45° to 2.03°). There was no significant influence of orthodontist experience and years of clinical practice on bracket positions (P = .314 and P = .158). The reproducibility among orthodontists was confirmed.
Conclusions
The reproducibility of digital indirect bonding was confirmed in terms of bracket positions using three-dimensional printed transfer trays.
Keywords: Indirect bonding, Three-dimensional image, Computer-aided design
INTRODUCTION
Orthodontic treatment should be efficient and effective, with the purpose of achieving excellent results during the final phase of treatment. Indirect bonding has been investigated over the years as a method with which to improve the bonding of orthodontic appliances.1
Previous studies2,3 found more accurate results by positioning the brackets with indirect bonding technique because the laboratory step eliminated the effect of salivary flow control, stress caused by longer duration of patient chair time, and impaired visualization due to the patient's lips, tongue, and cheeks. Yildirim and Sanglam-Aydinatay4 compared direct bonding with indirect bonding and observed that both techniques had successful outcomes; however, indirect bonding presented better results with better leveled marginal ridges.
Digital technology has increasingly been used to obtain three-dimensional (3D) models for diagnosis and treatment planning. Virtual occlusal records were shown5 to be precise for contact size and location in virtual bite registrations with an intraoral scanner. The digital indirect bonding technique also enables the possibility of superimposing the patient's tomographic image on the digital models in order to view dental roots and to determine accurate bracket positions.6 Virtual setup, 3D printing of models, and digital transfer trays for indirect bonding are among the other advances.7–10
Originally, brackets were bonded to plaster models and transferred back to a patient's teeth with an indirect bonding tray. More recently, it became possible to plan the bracket position virtually and to design an indirect bonding tray on a computer to be 3D printed and used to transfer the digital plan back to the patient's malocclusion.11
The digital indirect bonding technique was previously investigated for the efficacy and precision of the method, comparing final results with the virtual setup or with the results achieved by other bonding methods. and, in general, it was considered an efficient technique.12–16 However, there are few studies on digital indirect bonding techniques.1,17 Another consideration is that indirect bonding could be subject to errors involving construction of the transfer trays. This could be due to the type of material used, inelasticity or inadequate accuracy (resulting in incorrect transfer of the bracket position), or incorrect tray fit or distortion.18 Therefore, the aims of this study were to investigate the reproducibility of 3D-printed transfer tray fit on digital indirect bonding technique among orthodontists and to determine whether prior experience with other indirect bonding techniques or the number of years in clinical practice influenced the reproducibility of the procedure.
MATERIALS AND METHODS
This study was approved by the institutional review board of the Rio de Janeiro State University Hospital. One patient was selected and scanned with the Trios Color intraoral scanner (3Shape; Copenhagen, Denmark). The digital models were exported to Ortho Analyzer software (3Shape) for planning of bracket positions for performing digital indirect bonding performed by the Compass 3D company lab (Belo Horizonte, Minas Gerais, Brazil).
The patient's cone-beam computed tomography image was selected in order to superimpose this image on the digital models. To superimpose these two images, three equivalent points on each image were selected. Subsequently, the software set a best-fit superimposition, and the resulting image consisted of digital models reproducing the clinical crowns, while the tomography image showed the dental roots and surrounding bony structures.
For planning the bracket position on digital models, two different plans were devised using two bracket types: Mini Sprint Roth slot 0.022-inch (Forestadent, Pforzheim, Germany) and BioQuick self-ligating slot 0.022-inch (Forestadent). The virtual planning of Mini Sprint brackets did not include molars because of limited availability in the software virtual library.
The digital models with the brackets in position were exported to Appliance Designer software (3Shape), where the digital transfer trays were made. The software allowed for the construction of the tray limits on the buccal and lingual surfaces.
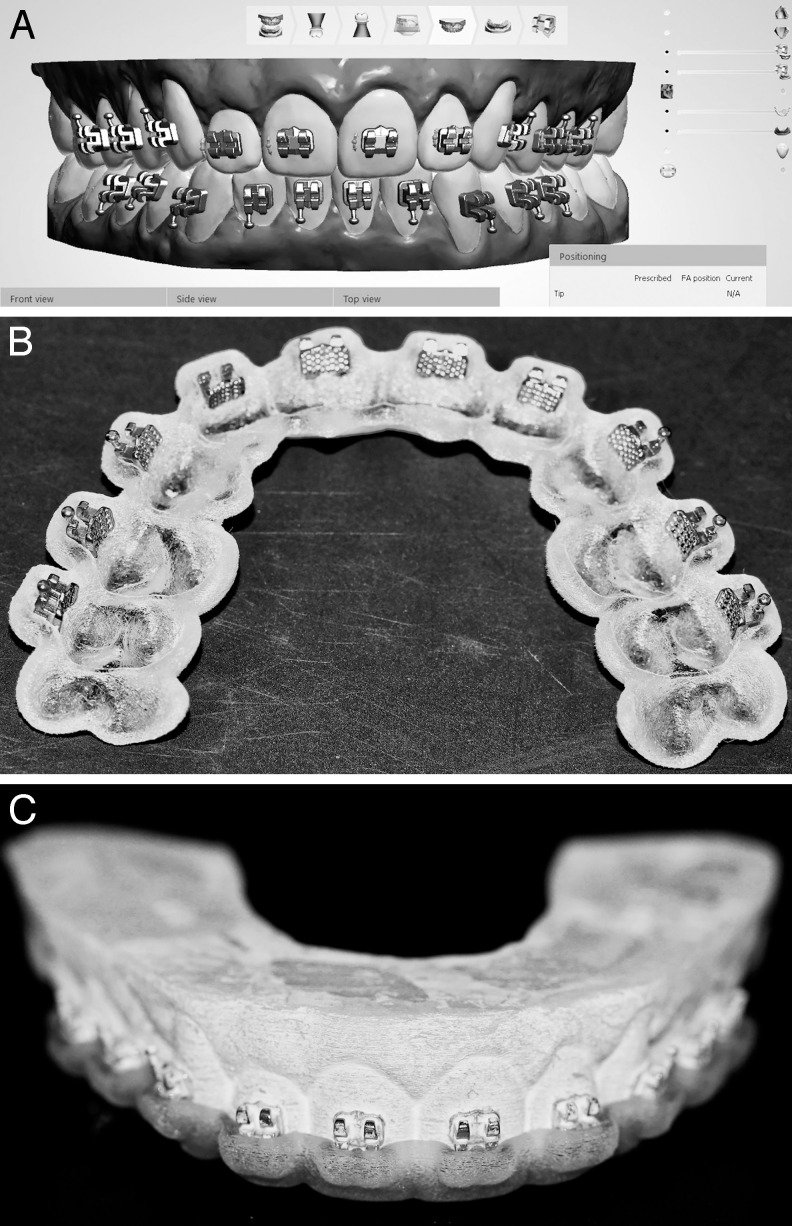
Thirty-three transfer trays and 33 prototype models of the selected occlusion were 3D printed using the 3D Stratasys printer (Objet 500 from Stratasys, Eden Prairie, Minn), and 33 orthodontists were asked to bond. The digital and prototyped models and the 3D-printed transfer trays are shown in Figure 1.
Figure 1.
A, Three-dimensional virtual plan; B, three-dimensional printed prototyped transfer tray for indirect bonding; C, indirect bonding performed by orthodontists.
All of the orthodontists were asked to complete an informed consent form. They also answered four questions related to the following: their age; whether they had practiced another specialty beside orthodontics; their years of clinical practice; and whether they had previous experience with an indirect bonding technique. The sample was gathered from the 20th Brazilian Congress of Orthodontics of São Paulo and from the Orthodontics Clinic of the Rio de Janeiro State University. Inclusion criteria were completion of an orthodontic residency at least 1 year prior to this study and current practice of orthodontics.
Each orthodontist was instructed on how to complete indirect bonding. To perform bonding, the orthodontists used the Transbond XT (3M Unitek, St. Paul, Minn) system. After indirect bonding, the brackets were light cured for 20 seconds on the buccal and occlusal surfaces. The prototyped models with bonded brackets were then scanned by an experienced operator with the intraoral scanner (Trios, 3Shape) after adequate calibration. The 33 sets of digital models with the indirect bonded brackets were imported into Ortho Analyzer software to compare the scanned models to their respective original digital plans.
Since there was no tooth movement, dental anatomy was selected to perform superimposition. Three points were selected in each arch. For the upper arch, one point on each buccal cusp ridge of the second premolars and one point on the mesial incisal edge of the right central incisor were selected. For the lower arch, one point on each buccal cusp ridge of the first premolars and one on the cusp tip of the right canine were selected.
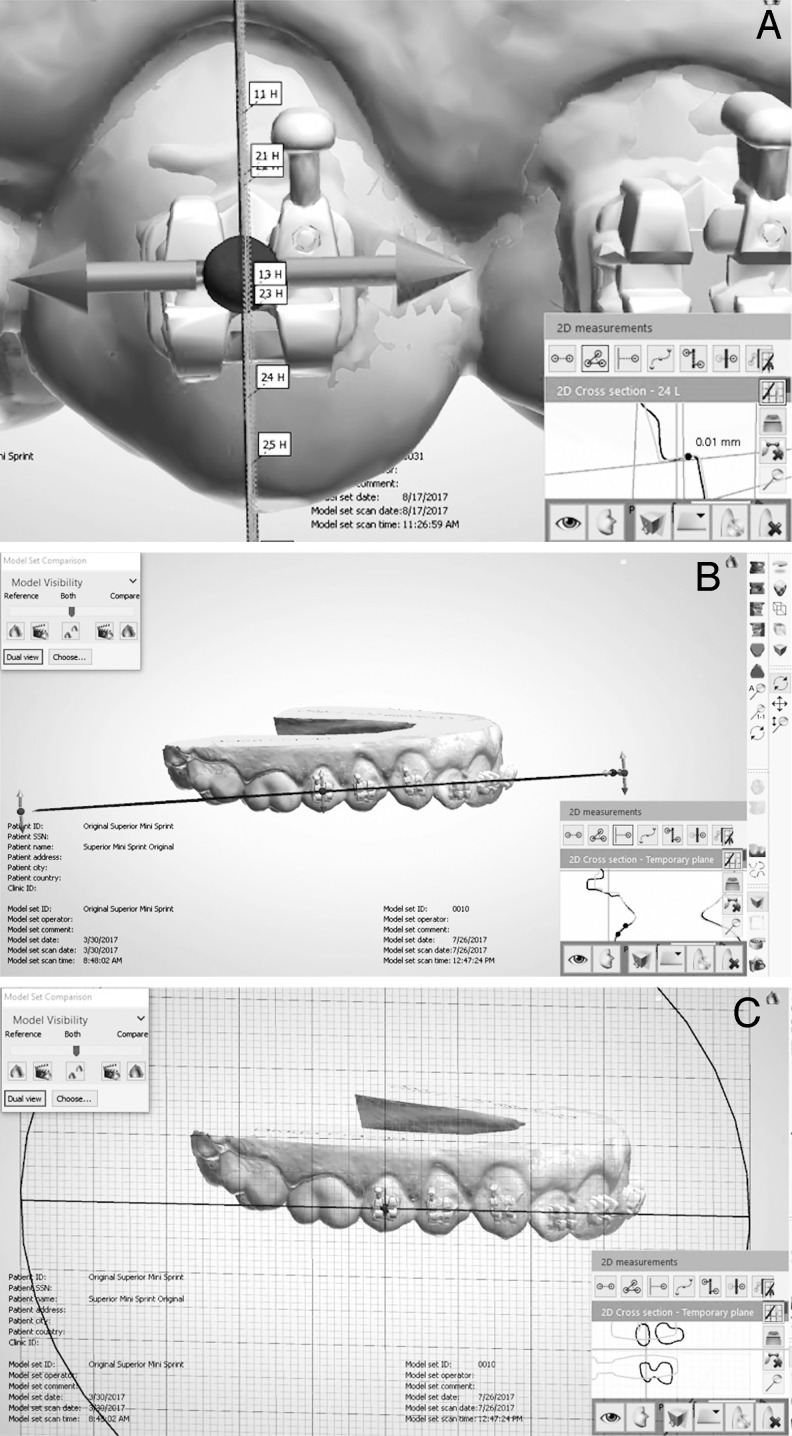
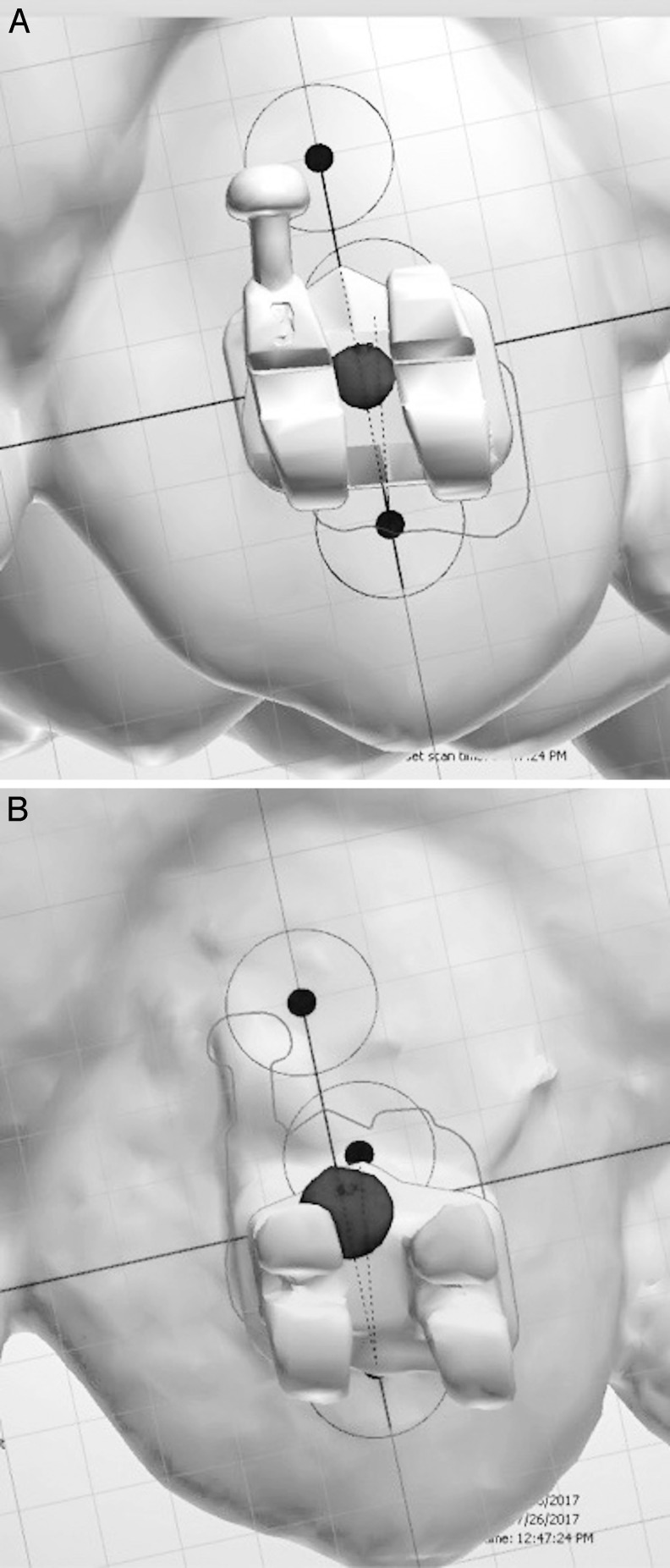
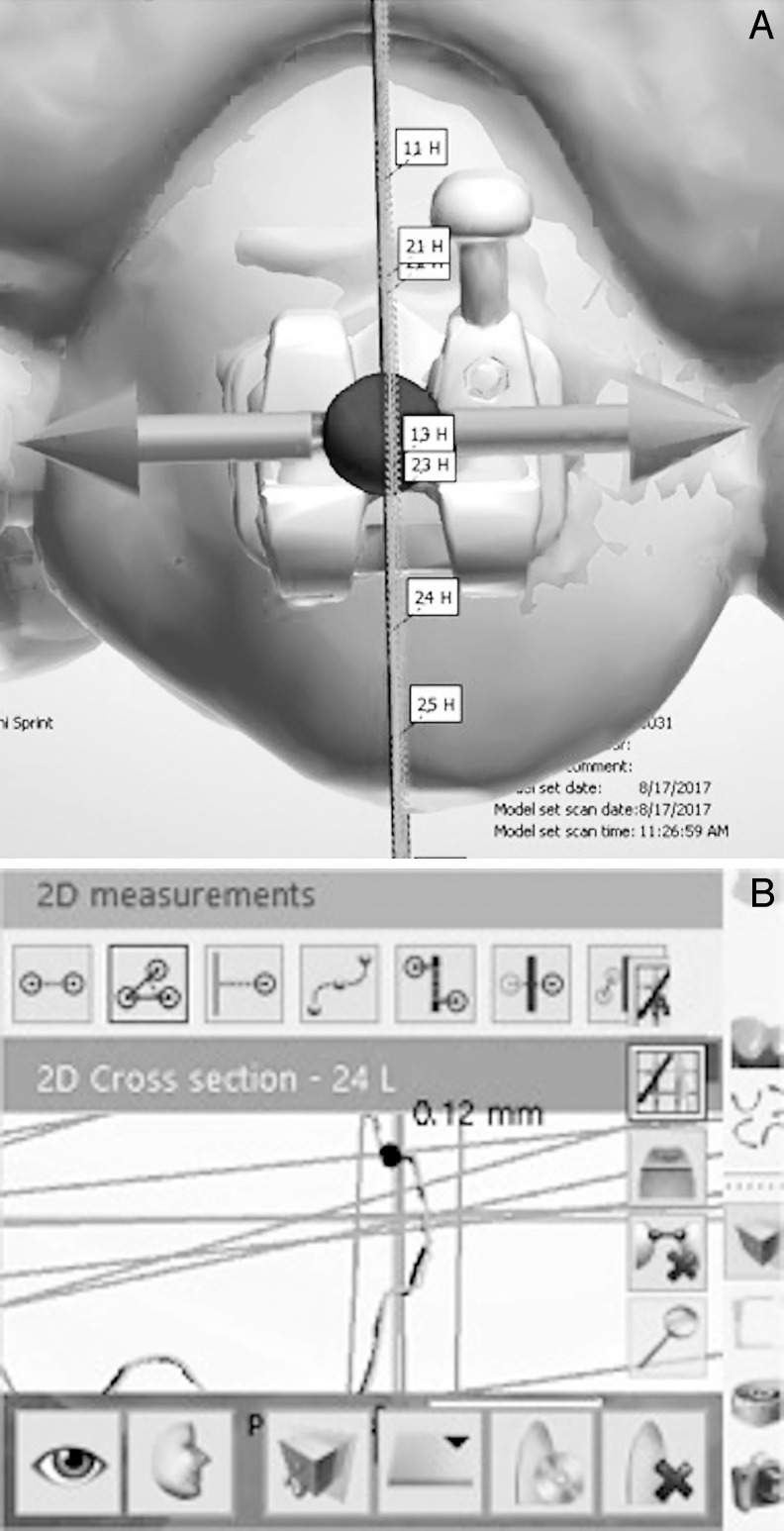
A previously trained evaluator performed the measurements to analyze the possible differences between brackets. Every bracket image was evaluated by defining three different measurements: vertical (occluso-gingival), horizontal (mesial-distal), and angulation (the angle resulting from the difference between the long axis of the brackets). Three planes for each bracket were traced for sectioning in each of these directions. This allowed each bracket base to be used to calculate the differences.
The vertical plane was traced to be parallel to the long axis of the bracket in a frontal view (using the bracket from the original planned model as a reference) and to be perpendicular to the bracket base, considered an occlusal view. The horizontal plane was parallel to the inner limits of the bracket wings and was positioned in the center of the slot in the frontal view. For the angulation measurements, the plane was positioned in a frontal view parallel to the bracket base (Figure 2).
Figure 2.
Reference planes for measuring the bracket positions. A, vertical plane for occluso-gingival dimension; B, horizontal plane for mesial-distal dimension; C, plane for analyzing bracket angulation.
Two points were then marked to quantify the differences between superimposed brackets for angulation: one on each limit representing the bracket's long axis of the original planned model and a third point on the bracket's long axis of the scanned model (Figure 3). To measure the difference in the vertical and horizontal planes, a sectional view from each plane was obtained, and the greater distance was measured (Figure 4). In this study, the analysis included a total of 356 brackets with 1038 measurements.
Figure 3.
Angulation measurement. A, selection of points representing the long axis of the bracket of the original virtual planning model; B, selection of point representing the long axis of the bracket of the scanned model after indirect bonding.
Figure 4.
Vertical measurement. A, Brackets after superimposition; B, cross-sectional view to calculate the difference in bracket position.
The method used to measure bracket differences was tested for reproducibility by having the same evaluator repeat the process 15 days later. Intra- and interevaluator reproducibilities were tested among the orthodontists. Three orthodontists were selected and asked to repeat the indirect bonding with the prototype transfer trays under identical conditions 15 days after the original procedure.
Statistical analysis was performed using ANOVA with repeated measures to evaluate the differences between the digital planning models and the models after bonding. Multivariate ANOVA was used to measure the influence of experience with indirect bonding and years of clinical practice. Bland-Altman plots were used to analyze reproducibility among orthodontists. Intraclass correlation coefficient measured the reproducibility of the method used. Statistical analysis was performed with statistical product and service solutions, SPSS for Mac (version 23.0; IBM Corp; Aramonk, NY).
RESULTS
Thirty-three orthodontists participated in this study, and they had a mean age of 40 years. Eighteen orthodontists had <15 years of clinical practice, while 15 had >15 years of clinical practice. Eighteen orthodontists had clinical experience with indirect bonding techniques, while 15 did not.
Means and standard deviations for the differences between bracket positions were obtained. The means of linear differences for upper Mini Sprint brackets ranged from 0.05 to 0.75 mm and for lower brackets from 0.02 to 0.29 mm. Angular differences were from 0.83° to 4.15° for the upper and from 0.45° to 1.64° for the lower. The means of linear differences for upper BioQuick brackets ranged from 0.02 to 0.15 mm and for lower brackets from 0.02 to 0.16 mm. Angular differences were from 0.18° to 1.05° for the upper and from 0.24° to 1.07° for the lower.
ANOVA for repeated measures found no statistically significant differences for bracket positions in all four groups, with the exception of horizontal differences for the lower BioQuick brackets (P = .016).
Intra- and interevaluator reproducibility were confirmed by the Bland-Altman plots (Figure 5) for each of the three orthodontists, divided by each dimension.
Figure 5.
Altman-Bland plot for intraevaluator analysis: A, B, C, Reproducibility regarding vertical dimension for each of the three orthodontists who repeated the indirect bonding (orthodontists 30, 31, and 32, respectively); D, E, F, for horizontal dimension; G, H, I, for angulation. First and third lines: upper confidence intervals; second line: upper limit; fourth and sixth lines: lower confidence intervals; fifth line: lower limit.
Figure 5.
Continued.
Intraclass correlation coefficient results were all >0.75, indicating excellent agreement. The results for the four models were 0.831, 0.848, 0.762, and 0.905.
Multivariate ANOVA demonstrated no statistically significant influence of the number of years of clinical practice or previous experience with indirect bonding techniques for the results of difference in bracket positions (P = .314 and P = .158).
DISCUSSION
To evaluate the reproducibility in bracket position, tracing the vertical, horizontal, and angulation planes allowed the same standard view for the measurements taken by the evaluator. This increased the accuracy of the method, as previously confirmed by Horton et al.19 They concluded that every method that allowed the evaluator to move and rotate the digital model in any direction resulted in a higher risk of bias.
The horizontal differences among positions of lower BioQuick brackets were statistically significant (P = .016). However, analysis of the other two dimensions (vertical and angulation) for the BioQuick group did not show significant differences. Additionally, the overall mean difference in bracket positions among this group was 0.05 mm, with a standard deviation of 0.04 mm, confirming that the difference was minimal.
Armstrong et al.20 stated that only differences of >0.25 mm for the positioning of incisor brackets and 0.5 mm for other teeth should be considered clinically significant. The model grading system developed by the American Board of Orthodontics noted that discrepancies of >0.5 mm in alignment and leveling of teeth would result in a negative evaluation.21 Castilla et al.22 concluded that differences of >0.13 mm in opposite directions for adjacent brackets should be considered clinically significant. Koo et al.23 found horizontal differences of 0.18 mm and vertical differences of 0.31 mm when analyzing indirect bonding. In the current study, the overall linear differences ranged from a mean of 0.04 mm to 0.42 mm, in agreement with those observed in the literature, confirming the reproducibility of the technique.
With regard to angulation, Larson et al.12 stated that differences of less than 2° could be considered clinically acceptable. Koo et al.23 found mean differences of 2.43° among brackets after indirect bonding. In the current study, the differences in means for each group were also less than those observed in the literature: 2.03° (upper Mini Sprint), 0.91° (lower Mini Sprint), 0.45° (upper BioQuick), and 0.59° (lower BioQuick).
Kim et al.24 evaluated the accuracy of a digital indirect bonding system by comparing the differences between the intended digital bracket positions and actual bracket positions after indirect bonding of five maxillary arch models. The current study confirmed the findings of Kim et al.24, who found no clinically relevant differences in bracket position. In that study,24 angulation mean differences were 1.53° and 1.52°.12,23
De Oliveira et al.25 compared the accuracy of digital indirect bonding with direct bonding performed by experienced clinicians and postgraduate students. Their results showed that clinical experience had a positive influence on accuracy with regard to angular dimension in digital bonding. The current findings demonstrate that clinical experience had no influence on the reproducibility of bonding with prototyped transfer trays, although the accuracy of bonding between different techniques was not compared.
A possible reason for the discrepancies observed among bracket positions could be the differences in positioning and fit of the prototype transfer trays on the models by each orthodontist. Incorrect fit of the tray could lead to an error in its occlusal position. Additionally, the wrong fit of each bracket in its respective space in the tray could also lead to errors, thereby decreasing the accuracy of the technique.22,26
Advantages of the digital indirect bonding technique include possibly less archwire bending, the need for fewer appointments to change bracket positions, and the opportunity to demonstrate to the patient the 3D treatment plan on a computer screen.14,27,28 Additionally, digital indirect bonding with 3D-printed transfer trays allows the bracket base to be free of adhesive before clinical bonding. This advantage decreases the risk of failure of adhesion after clinical bonding and the possibility of having excess adhesive on the bracket base surface.16
This study was a preliminary investigation of the digital indirect bonding technique regarding the precision of 3D-printed tray fit, with controlled variables such as different types of malocclusions. Therefore, further clinical studies to test the reproducibility of bracket positioning with a variety of malocclusions, as well to test the influence of the clinical environment to analyze the accuracy of the technique, are required.
CONCLUSIONS
Indirect bonding using 3D-printed guides can accurately reproduce the position of brackets virtually placed on digital models. This can occur regardless of the orthodontist's previous experience with the technique or the number of years of clinical practice.
Both self-ligating and conventional bracket libraries can be used for digital indirect bonding. There were no statistically significant differences between the digital plan and the bonded brackets placed with 3D-printed indirect bonding trays, except for lower BioQuick brackets, in which case the difference was not clinically relevant.
ACKNOWLEDGMENTS
We thank the professors and students of the Department of Orthodontics of Rio de Janeiro State University, Dr. Carlo Marassi, and Dr. Diogo Frazão for having assisted in this research and Dr. Ronir Raggio Luiz for the guidance regarding the statistics. This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – Brasil (CAPES) – Finance Code 001. The authors do not have any financial interest in the companies whose materials are included in this article.
REFERENCES
- 1.Kalange JT, Thomas RG. Indirect bonding: a comprehensive review of the literature. Semin Orthod. 2007;13(1):3–10. [Google Scholar]
- 2.Vianna VF, Mucha JN. Vertical accessories positioning in orthodontics fixed appliances. Dental Press J Orthod. 2006;11(4):66–75. [Google Scholar]
- 3.Gange P. The evolution of bonding in orthodontics. Am J Orthod Dentofacial Orthop. 2015;147(4):56–63. doi: 10.1016/j.ajodo.2015.01.011. [DOI] [PubMed] [Google Scholar]
- 4.Yildirim K. Saglam-Aydinatay. Comparative assessment of treatment efficacy and adverse effects during nonextraction orthodontic treatment of Class I malocclusion patients with direct and indirect bonding: a parallel randomized clinical trial. Am J Orthod Dentofac Orthop. 2018;154:26–34. doi: 10.1016/j.ajodo.2017.12.009. [DOI] [PubMed] [Google Scholar]
- 5.Botsford KP, Frazier MC, Ghoneima AAM, Utreja A, Bhamidipalli SS, Stewart KT. Precision of the virtual occlusal record. Angle Orthod. In press. [DOI] [PMC free article] [PubMed]
- 6.Israel M, Kusnoto B, Evans CA, Begole E. A comparison of traditional and computer-aided bracket placement methods. Angle Orthod. 2011;81(5):828–835. doi: 10.2319/072110-425.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Camardella LT, Rothier EKC, Vilella OV, Ongkosuwito EM, Breuning KH. Virtual setup: application in orthodontic practice. J Orofac Orthop. 2016;77(6):409–419. doi: 10.1007/s00056-016-0048-y. [DOI] [PubMed] [Google Scholar]
- 8.Müller-Hartwich R, Jost-Brinkmann PG, Schubert K. Precision of implementing virtual setups for orthodontic treatment using CAD/CAM-fabricated custom archwires. J Orofac Orthop. 2016;77(1):1–8. doi: 10.1007/s00056-015-0001-5. [DOI] [PubMed] [Google Scholar]
- 9.Sachdeva R. SureSmile technology in a patient-centered practice. J Clin Orthod. 2001;35(4):245–253. [PubMed] [Google Scholar]
- 10.Sachdeva RCL. A review of suresmile®: efficiency and effectiveness—sprinkled with a dose of self-reflection. Columns Current Issue—Orthodontic Practice US. 2017 Available at: https://www.orthopracticeus.com/columns/review-suresmile-efficiency-effectiveness-sprinkled-dose-self-reflection Accessed September 26, 2018.
- 11.Graf S, Cornelis MA, Hauber Gameiro G, Cattaneo PM. Computer-aided design and manufacture of hyrax devices: can we really go digital? Am J Orthod Dentofac Orthop. 2017;152(6):870–874. doi: 10.1016/j.ajodo.2017.06.016. [DOI] [PubMed] [Google Scholar]
- 12.Larson BE, Vaubel CJ, Grunheid T. Effectiveness of computer-assisted orthodontic treatment technology to achieve predicted outcomes. Angle Orthod. 2013;83(4):557–562. doi: 10.2319/080612-635.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alford TJ, Roberts WE, Hartsfield JK, Eckert GJ, Snyder RJ. Clinical outcomes for patients finished with the SureSmile method compared with conventional fixed orthodontic therapy. Angle Orthod. 2011. pp. 383–388. [DOI] [PMC free article] [PubMed]
- 14.Son KH, Park JW, Lee DK, Kim KD, Baek SH. New virtual orthodontic treatment system for indirect bonding using the stereolithographic technique. Korean J Orthod. 2011;4181(2)(3):138–146. [Google Scholar]
- 15.Brown M, Koroluk L, Ko C, Zhang K, Chen M, Nguyen T. Effectiveness and efficiency of a CAD/CAM orthodontic bracket system. Am J Orthod Dentofac Orthop. 2015;148(6):1067–1074. doi: 10.1016/j.ajodo.2015.07.029. [DOI] [PubMed] [Google Scholar]
- 16.El-Timamy AM, El-Sharaby FA, Eid FH, Mostafa YA. Three-dimensional imaging for indirect-direct bonding. Am J Orthod Dentofac Orthop. 2016;149(6):928–931. doi: 10.1016/j.ajodo.2015.12.009. [DOI] [PubMed] [Google Scholar]
- 17.Joiner M. In-house precision bracket placement with the indirect bonding technique. Am J Orthod Dentofac Orthop. 2010;137(6):850–854. doi: 10.1016/j.ajodo.2009.04.023. [DOI] [PubMed] [Google Scholar]
- 18.Aksakalli S, Demir A. Indirect bonding: a literature review. Eur J Gen Dent. 2012;1(1):6. [Google Scholar]
- 19.Horton HMI, Miller JR, Gaillard PR, Larson BE. Technique comparison for efficient orthodontic tooth measurements using digital models. Angle Orthod. 2010;80(2):254–261. doi: 10.2319/041709-219.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Armstrong D, Shen G, Petocz P, Darendeliler MA. A comparison of accuracy in bracket positioning between two techniques—localizing the center of the clinical crown and measuring the distance from the incisal edge. Eur J Orthod. 2007;29(5):430–436. doi: 10.1093/ejo/cjm037. [DOI] [PubMed] [Google Scholar]
- 21.Casko JS, Vaden JL, Kokich VG, et al. Objective grading system for dental casts and panoramic radiographs. American Board of Orthodontics. Am Board Orthod. 1998;114(5):1–22. doi: 10.1016/s0889-5406(98)70179-9. [DOI] [PubMed] [Google Scholar]
- 22.Castilla AE, Crowe JJ, Moses JR, Wang M, Ferracane JL, Covell DA. Measurement and comparison of bracket transfer accuracy of five indirect bonding techniques. Angle Orthod. 2014;84(4):607–614. doi: 10.2319/070113-484.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Koo BC, Chung CH, Vanarsdall RL. Comparison of the accuracy of bracket placement between direct and indirect bonding techniques. Am J Orthod Dentofacial Orthop. 1999;116(3):346–351. doi: 10.1016/s0889-5406(99)70248-9. [DOI] [PubMed] [Google Scholar]
- 24.Kim J, Chun YS, Kim M. Accuracy of bracket positions with a CAD/CAM indirect bonding system in posterior teeth with different cusp heights. Am J Orthod Dentofacial Orthop. 2018;153(2):298–307. doi: 10.1016/j.ajodo.2017.06.017. [DOI] [PubMed] [Google Scholar]
- 25.De Oliveira NS, Rossouw E, Lages EMB, Macari S, Pretti H. Influence of clinical experience on accuracy of virtual orthodontic attachment bonding in comparison with the direct procedure. Angle Orthod. 2019. pp. 1–8. [DOI] [PMC free article] [PubMed]
- 26.Nigoumi AEL. Assessing the accuracy of indirect bonding with 3D scanning technology. J Clin Orthod. 2009;30950(11)(10):613–619. [PubMed] [Google Scholar]
- 27.Mayhew MJ. Computer-aided bracket placement for indirect bonding. J Clin Orthod. 2005. pp. 653–660. [PubMed]
- 28.Garino F, Garino GB. Computer-aided interactive indirect bonding. Progr Orthod. 2005;6(2):214–223. [PubMed] [Google Scholar]