Abstract
Introduction
Testicular torsion is a real emergency condition which requires prompt diagnosis and surgical management to prevent testicular loss. During the coronavirus (COVID-19) pandemic, an increased avoidance of the emergency departments for non-COVID-19 illnesses has been reported in the medical literature.
Objective
The aim of this study was to investigate whether the COVID-19 pandemic caused increased number of orchiectomies in pediatric patients presenting with acute testicular torsion compared to pre-COVID-19 period.
Study design
A total number of 119 pediatric patients who underwent surgery for acute testicular torsion from January 2019 to December 2020 were enrolled in retrospective multi-center study from six institutions in Croatia. The patients were divided in two groups. The first group (pre-COVID-19) consisted of the patients who underwent surgery before COVID-19 pandemic (n = 68), while the second group (COVID-19) consisted of the patients who underwent surgery during the COVID-19 pandemic (n = 51). Main outcomes of the study were orchiectomy rates and time from onset of the symptoms to emergency department presentation.
Results
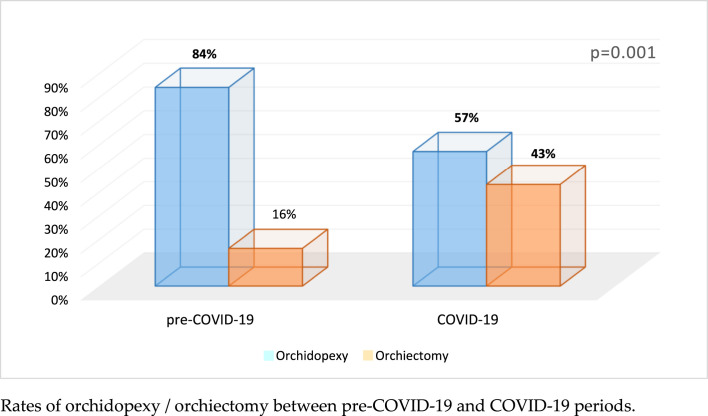
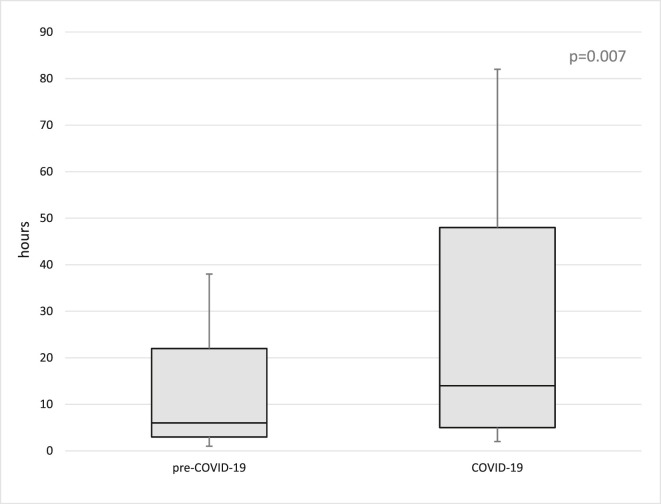
During the COVID-19 pandemic period 43.1% (22/51) of the patients underwent orchiectomy while orchiectomy was performed in 16.2% (11/68) of the patients from the pre-COVID group (p = 0.001). Median time from onset of the symptoms to emergency department presentation during COVID-19 pandemic and pre-COVID-19 periods was 14h (IQR 5, 48) and 6h (IQR 3, 22) (p = 0.007), respectively. A higher proportion of patients waited over 24 h to present to emergency department during the COVID-19 pandemic compared to the pre-COVID-19 period (47% vs 8.8%, p = 0.007).
Conclusion
During COVID-19 pandemic a significantly higher rates of orchiectomies and increase in delayed presentations for testicular torsion was found. More patient education during pandemic in regards to management of emergency conditions such as testicular torsion is required.
Summary figure.
Rates of orchidopexy/orchiectomy between pre-COVID-19 and COVID-19 periods.
Keywords: Testicular torsion, Acute scrotum, COVID-19, Pandemic, Urologic emergencies, Children
Introduction
Testicular torsion is a common pediatric emergency which occurs when the testicle rotates around its axis leading to an impaired blood supply and possible irreversible changes and a complete loss of testis [1]. An incidence of testicular torsion is 4.5 in 100,000 males up to 25 years of age [2]. Testicular torsion can occur at any age but usually occurs in newborns and young males who are in puberty or adolescence, between the ages of 13 and 16 years [3]. Testicular torsion is most often presented by sudden onset of pain, swelling and redness of the affected side of the scrotum. The testis is hard and often positioned higher than normal or at an unusual angle [[1], [2], [3]]. In rare cases testicular torsion may have unusual presentation and lower abdominal pain can be the only presenting symptom [[3], [4], [5]]. Also an unusual variant of testicular torsion can occur in the setting of cryptorchidism, with testicular torsion in inguinal canal [3,6].
Prompt diagnosis and surgical management with scrotal exploration and detorsion are important to prevent testicular loss. The likelihood of testicular salvage is time-dependent. Many studies reported that a testicle torsed for longer than six to 8 h is outside the timeframe for survival [[1], [2], [3], [4]]. A recent systematic review of the literature showed that testicular survival time, in the case of testicular torsion, can be much longer than six to 8 h as previously believed. Survival percentages are significant even past 24 h of torsion [7]. Additionally, time from onset of symptoms to the operating room is an independent predictor of testicular survival [1,2,7].
During the coronavirus (COVID-19) pandemic, an increased avoidance of the emergency departments for non-COVID-19 illnesses has been reported in the medical literature [[8], [9], [10], [11], [12]]. Pediatric patients do not commonly experience medical conditions with a high risk of mortality but delay in diagnosis can lead to a significant increase in morbidity, prolonged hospitalization, increased financial expense and mortality [12]. For example, during the first wave of a COVID-19 pandemic, a significantly higher rate of perforated appendicitis was recorded in children, compared to the same period one year before pandemic (39% vs. 13%) [11].
Stay-at-home orders and a fear from corona virus infection during COVID-19 pandemic may also contribute to delays in presentation of patients with testicular torsion to emergency departments and may significantly increase a number of testicular loss. The aim of this multicenter retrospective study was to investigate whether the COVID-19 pandemic caused increased number of orchiectomies in pediatric patients presenting with acute testicular torsion. Our hypothesis was that delays in presentation to the emergency department, as well as the rates of orchiectomy, were increased during the COVID-19 pandemic period.
Patients and methods
Patients
A total of 119 pediatric patients who underwent emergency scrotal exploration for acute testicular torsion and met the inclusion criteria, between January 2019 and December 2020, were enrolled in the study. The patients were divided in two groups. The first group (pre-COVID-19) consisted of the patients who underwent surgery before COVID-19 pandemic, January 1st, 2019 to March 10th, 2020. The second group (COVID-19) consisted of the patients who underwent surgery during the COVID-19 pandemic, March 11th, 2020 to December 31st, 2020. The pandemic cohort was determined based on the World Health Organization declaration of a pandemic on March 11th, 2020.
Inclusion criteria were pediatric patients aged one month to 17 years who underwent emergent surgery due to an acute testicular torsion at the included centers. Exclusion criteria were neonatal torsions (age <1 month), patients older than 17 years of age, patients in whom testicular torsion during scrotal exploration has not been confirmed, patients operated in other than included centers and patients who underwent manual detorsion of the testis.
The study was carried out in Croatia as a multicenter retrospective study. Six centers participated in the study: the Department of Pediatric Surgery at University Hospital of Split (n = 50), the Department of Pediatric Surgery at University Hospital of Zagreb (n = 22), the Department of Pediatric Surgery at University Hospital of Rijeka (n = 19), the Department of Pediatric Surgery at University Hospital of Osijek (n = 17), the Department of Pediatric Surgery at General Hospital Šibenik (n = 7) and the Department of Pediatric Surgery at General Hospital Zadar (n = 4). The study protocol was approved by the Ethics Review Board of each center included in study.
Outcome measurements
The primary outcome of the study was orchiectomy rate. The secondary outcome was time from onset of the symptoms to emergency department presentation.
Study protocol
For each patient; medical history, demographic data (age, weight, height, body mass index), dwelling, distance from the hospital, side of torsion, duration of symptoms, presenting symptoms, preoperative ultrasound, intraoperative findings (degree of torsion) and outcomes of treatment (detorsion and fixation or orchiectomy) and recurrences were recorded in the study protocol.
Surgery and follow-up
The surgery was performed in the emergency settings after a clinical examination and ultrasound examination of the scrotum, which depended on the judgment of the operating surgeon. Description of the surgical procedure and algorithm of treatment are available in our previously published study [2]. Postoperatively, the patients received pain medication and were observed in department of pediatric surgery at the included centers. The patients were followed up postoperatively for detection of late complications.
Statistical analysis
The SPSS 24.0 software (IBM Corp, Armonk, NY) was used to analyze the data. Median and interquartile range (IQR) or mean and standard deviation (SD) were used for quantitative or an ordinal variables. To describe a distribution of a categorical variables absolute and relative frequencies were used. The significance of differences in quantitative variables between the study groups was assessed by the t-test for independent samples, or by its alternative - nonparametric test (Mann–Whitney U test). The chi-square test was used to assess differences in distribution of categorical data. When the frequency of events in a certain cell was low, Fisher exact test was used instead. All the tests were two-sided and the significance level of 0.05 was used.
Results
During study period, a total number of 119 patients underwent surgery because of acute testicular torsion. During the selected pre-COVID-19 and the COVID-19 pandemic periods 68 and 51 patients with acute testicular torsion were identified, respectively. Demographic and baseline characteristics of the patients from both groups are presented in Table 1 . The two groups did not differ significantly in regards to age, height, weight, laterality of torsion, travel distance and clinical presentation.
Table 1.
Demographic and preoperative clinical characteristics of the patients.
| Group I |
Group II |
P | |
|---|---|---|---|
| pre-COVID-19 (n = 68) | COVID-19 (n = 51) | ||
| Age (years) median (IQR) | 14 (13, 16) | 15 (14, 16) | 0.133a |
| Height (cm) median (IQR) | 170 (162.5, 179) | 175 (165, 183) | 0.089a |
| Weight (kg) median (IQR) | 55.5 (48, 65) | 60 (45, 70) | 0.222a |
| BMI (kg/m2) median (IQR) | 20.4 (18.7, 23) | 21.1 (18.9, 23.6) | 0.329a |
| Laterality, n (%) | |||
| Left | 33 (48.5) | 16 (31.4) | 0.059b |
| Right | 35 (51.5) | 35 (68.6) | |
| Travel distance (km) median (IQR) | 18 (4, 53) | 19 (5, 45) | 0.659a |
| Clinical presentation, n (%) | |||
| Pain | 67 (98.5) | 50 (98) | 0.677b |
| Swelling | 54 (79.4) | 45 (88.2) | |
| Redness | 18 (26.5) | 22 (43.1) | |
| Hard testicle | 47 (69.1) | 35 (68.6) | |
| Transverse lie | 46 (67.6) | 33 (64.7) | |
IQR – Interquartile range.
Mann-Whitney U-test.
Chi square test.
In selected study period statistically significant difference in regards to primary outcome of the study (rate of orchiectomy) was found. During the COVID-19 pandemic period 43.1% (22/51) of the patients underwent orchiectomy while orchiectomy was performed in 16.2% (11/68) of patients from the pre-COVID group (p = 0.001) Figure Summary figure (Table 2 ).
Table 2.
Intraoperative findings and treatment outcomes of the patients.
| Group I |
Group II |
P | |
|---|---|---|---|
| pre-COVID-19 (n = 68) | COVID-19 (n = 51) | ||
| Degree of torsion (°) median (IQR) | 360 (360, 720) | 360 (360, 720) | 0.238a |
| Duration of symptoms (h) median (IQR) | 6 (3, 22) | 14 (5, 48) | 0.007a |
| Duration of symptoms 12–24 h n (%) | 7 (10.3) | 5 (9.8) | 0.929b |
| Duration of symptoms >24 h n (%) | 16 (8.8) | 24 (47.0) | 0.007b |
| Orchiectomy rate, n (%) | 11 (16.2) | 22 (43.1) | 0.001b |
| Orchiopexy rate, n (%) | 57 (83.8) | 29 (56.9) | |
| Delay seeking help, n (%) | 23 (38.2) | 29 (56.9) | 0.012b |
IQR – Interquartile range.
Mann–Whitney U-test.
Chi-square test.
In regards to secondary outcome of the study during the COVID-19 pandemic period time from onset of the symptoms to emergency department presentation was 14 h (IQR 5, 48) while in the pre-COVID-19 cohort of the patients time to presentation to emergency department was significantly shorter, 6 h (IQR 3, 22) (p = 0.007) (Fig. 1 , Table 2). A higher proportion of patients waited over 24 h to present to emergency department during the COVID-19 pandemic compared to the pre-COVID-19 period was found, 47% vs 8.8%, p = 0.007 (Table 2). There was no significant difference in the time between presentation to emergency room and taking to operating room between two investigated periods. Moreover it was slightly shorter in COVID-19 pandemic period – 68 min (IQR, 40, 74 min) compared to pre-COVID-19 – 75 min (45, 80 min) (P = 0.155).
Fig. 1.
Time from onset of the symptoms to emergency department presentation between pre-COVID-19 and COVID-19 periods.
Out of total number of the patients included in study 56.9% of patients from the COVID-19 pandemic group indicated a delay in seeking care compared with 38.2% of the pre-COVID-19 group (p = 0.007). The most common reason in COVID-19 pandemic cohort was fear of COVID-19 virus infection while in pre-COVID-19 cohort were symptoms starting during the night and patients delaying telling parents about the symptoms.
Table 3 shows comparison of the main outcomes between the centers enrolled in study. Between pre-COVID-19 and COVID-19 cohorts, in all centers increased percentage of orchiectomies (except in one center) and longer mean time from onset of the symptoms to emergency department presentation was found.
Table 3.
Comparison of the main outcomes between the centers enrolled in study.
| Center | Characteristic |
Group I |
Group II |
P |
|---|---|---|---|---|
| n (%) or mean ± SD | pre-COVID-19 | COVID-19 | ||
| University Hospital of Split | Orchidopexy | 23 (79) | 11 (52) | 0.043a |
| Orchiectomy | 6 (21) | 10 (48) | ||
| Duration of symptoms (h) | 19.1 ± 15.0 | 37.0 ± 45.9 | 0.041b | |
| University Hospital of Zagreb | Orchidopexy | 12 (86) | 6 (75) | 0.601c |
| Orchiectomy | 2 (14) | 2 (25) | ||
| Duration of symptoms (h) | 10.7 ± 10.9 | 13.3 ± 18.1 | 0.787b | |
| University Hospital of Rijeka | Orchidopexy | 9 (100) | 5 (50) | 0.032c |
| Orchiectomy | 0 (0) | 5 (50) | ||
| Duration of symptoms (h) | 5.7 ± 7.0 | 40.6 ± 50.4 | 0.028b | |
| University Hospital of Osijek | Orchidopexy | 8 (80) | 7 (100) | 0.485c |
| Orchiectomy | 2 (20) | 0 (0) | ||
| Duration of symptoms (h) | 13.4 ± 14.5 | 27.5 ± 33.9 | 0.047b | |
| Šibenik General Hospital | Orchidopexy | 4 (100) | 0 (0) | 0.028c |
| Orchiectomy | 0 (0) | 3 (100) | ||
| Duration of symptoms (h) | 3.2 ± 0.9 | 48 ± 24.9 | 0.001b | |
| Zadar General Hospital | Orchidopexy | 1 (50) | 0 (0) | >0.999c |
| Orchiectomy | 1 (50) | 2 (100) | ||
| Duration of symptoms (h) | 17 ± 18.3 | 19.5 ± 0.7 | 0.432b |
SD – Standard deviation.
Chi square test.
t-test for independent samples.
Fisher exact test.
Discussion
The results of this study clearly demonstrated significantly higher number of orchiectomies during the COVID-19 pandemic compared with pre-COVID-19 period. Also, significantly longer time from the onset of symptoms to emergency department presentation was recorded during the COVID-19 pandemic. Both outcomes are very likely an indirect effect of the COVID-19 pandemic. Patients in the COVID-19 pandemic group were significantly more likely to endorse a delay in seeking emergency medical care compared to pre-COVID-19 group, which also supports COVID-19 leading to indirect delays in professional medical care.
During the COVID-19 pandemic in most of the centers elective surgical procedures were canceled. Surgical procedures were limited only for the care of urgent surgical or trauma patients. These efforts to minimize unnecessary traffic through the healthcare facility resulted in a significant reduction in emergency department patient encounters [12,13]. Significant increases in delayed care for different medical emergencies, including pediatric surgical emergencies, during the COVID-19 pandemic period has been noted by the medical community and published in several reports [[8], [9], [10], [11], [12], [13]].
Several recent studies of acute appendicitis during COVID-19 pandemic clearly showed that staying at home due to public health safety orders negatively impacted children who developed appendicitis. During the COVID-19 pandemic increased rate of perforated appendicitis in pediatric patients, compared to pre-COVID-19 period, was reported in several published studies [11,[13], [14], [15]]. Also, the patients with perforated appendicitis had an increased rate of complications and length of hospital stay [13].
In the available literature, only two studies investigated whether the COVID-19 pandemic caused increased number of orchiectomies and delays in presentation to emergency department in pediatric patients suffering from acute testicular torsion. Contrary to our results Nelson et al. in their study found that time from onset of symptoms to emergency department presentation, ischemic times, and orchiectomy rates for testicular torsion at their center were not significantly different during the COVID-19 pandemic period compared to pre-COVID period [16]. Although in their town dramatic drop in urgent presentations for stroke, heart attack and cancer during the COVID-19 was noticed. They explained this finding with the fact that the nature of this condition, the severity and acuity of symptoms associated with testicular torsion and visible swelling, make this condition difficult to ignore [16]. Littman et al. in their study also did not found delay presentation to a medical facility or a higher rate of orchiectomy during the COVID-19 pandemic [17]. We are of the opinion that this results are due exclusively to the small number of patients with testicular torsion in COVID-19 pandemic (n = 17 and n = 21), as well as the fact that patients from only one center were included in the study. Six centers with a significantly higher number of patients (n = 119) participated in our study. Furthermore, both studies collected patients with testicular torsion in COVID-19 group from only March through May of 2020 while our study continued by the end of the year. Comparing the patients from each center separately, clearly showed that no significant difference between the groups in some of the centers was recorded, mostly in the centers with small sample size while in centers with larger number of patients' included significant difference was found.
Baseline rate of orchiectomies for testicular torsion is already high and varies between 20 and 35% [1]. The rate of orchiectomies in a large study from USA was 34% while in our previous study was 28% [2,18]. Regardless to the pandemic, some children have delayed presentation to the emergency departments for acute testicular torsion. Recent study reported that 13% of children with torsion may delay informing their parents, mostly due to shame and fear. Also the children with autism spectrum disorders are at higher risk of delayed presentation [19]. As we know that most of the testicles would be saved if surgery is performed within 6–8 h from the onset of symptoms we can conclude that there are two essential time frames, where valuable time tends to get lost. The first one is the duration of the symptoms, until the child indicates the problem and manages to present to the emergency room while the second one is the time the pediatric surgeon or emergency care physician needs to make the accurate diagnosis and initiate the treatment [[1], [2], [3], [4]]. During the COVID-19 pandemic many patients delayed to present to emergency departments because of the fear of corona infection in the hospital, which further extended the already short time we have to save the testicle. Also, we reported the time from presentation to emergency room to taking to operating room was not significantly different between the groups. Our in-house time (for diagnostic procedures and preparation of the patient) was 68–75 min, which is excellent if we compare it to the literature. The in-hospital delay reported by Johnston et al. was 2 h and 24 min for the patients under 14-years of age, and 2 h and 35 min for the patients older than 14-years of age [20].
This is the first multi-center and long-term study in pediatric patients which clearly showed influence of COVID-19 pandemic on acute testicular torsion. Although we clearly demonstrated increased number of orchiectomies and significantly longer time to presentation to the emergency departments this study has several limitations. Retrospective character is the main limitation of this study, although we have implemented multiple plausibility checks and cross validations in our data collection tool. Further studies or meta-analysis are needed to analyze the same parameters on a larger sample. Also a contemporary prospective control cohort would have improved our findings, but in this moment we cannot plan that because we do not know whether the pandemic will continue.
Conclusion
During COVID-19 pandemic a significantly higher rates of orchiectomies and increase in delayed presentations for testicular torsion was found. More patient education during pandemic in regards to management of emergency conditions such as testicular torsion is required.
Ethical approval
The study protocol was approved by the Ethics Review Board of each center included in study (references: Split – 2181-147-01/06/M.S.-20-02; Zagreb – 02/21AG; Rijeka – 2170-29-02/1-2-2; Osijek – R2-3563/2021; Šibenik – 01-498/1-4 and Zadar 02-759/21-3/21).
Funding
None declared.
Conflicts of interest
None declared.
References
- 1.Zvizdic Z., Aganovic A., Milisic E., Jonuzi A., Zvizdic D., Vranic S. Duration of symptoms is the only predictor of testicular salvage following testicular torsion in children: a case-control study. Am J Emerg Med. 2021;41:197–200. doi: 10.1016/j.ajem.2020.11.023. [DOI] [PubMed] [Google Scholar]
- 2.Pogorelić Z., Mustapić K., Jukić M., Todorić J., Mrklić I., Meštrović J. Management of acute scrotum in children: a 25-year single center experience on 558 pediatric patients. Can J Urol. 2016;23(6):8594–8601. [PubMed] [Google Scholar]
- 3.Pogorelic Z., Neumann C., Jukic M. An unusual presentation of testicular torsion in children: a single - centre retrospective study. Can J Urol. 2019;26(6):10026–10032. [PubMed] [Google Scholar]
- 4.Pogorelić Z., Mrklić I., Jurić I. Do not forget to include testicular torsion in differential diagnosis of lower acute abdominal pain in young males. J Pediatr Urol. 2013;9(6):1161–1165. doi: 10.1016/j.jpurol.2013.04.018. [DOI] [PubMed] [Google Scholar]
- 5.Vasconcelos-Castro S., Soares-Oliveira M. Abdominal pain in teenagers: beware of testicular torsion. J Pediatr Surg. 2020;55(9):1933–1935. doi: 10.1016/j.jpedsurg.2019.08.014. [DOI] [PubMed] [Google Scholar]
- 6.Pogorelić Z., Mrklić I., Jurić I., Biočić M., Furlan D. Testicular torsion in the inguinal canal in children. J Pediatr Urol. 2013;9(6):793–797. doi: 10.1016/j.jpurol.2012.10.013. [DOI] [PubMed] [Google Scholar]
- 7.Mellick L.B., Sinex J.E., Gibson R.W., Mears K. A systematic review of testicle survival time after a torsion event. Pediatr Emerg Care. 2019;35(12):821–825. doi: 10.1097/PEC.0000000000001287. [DOI] [PubMed] [Google Scholar]
- 8.Mehanathan P.B., Edwards A.A., Athisayamani, Robinson T. Experience of a surgeon at the emergency department during COVID-19 pandemic. Ann Med Surg (Lond) 2020;60:245–248. doi: 10.1016/j.amsu.2020.10.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.D'Urbano F., Fabbri N., Koleva Radica M., Rossin E., Carcoforo P. Emergency surgery in COVID-19 outbreak: has anything changed? Single center experience. World J Clin Cases. 2020;8(17):3691–3696. doi: 10.12998/wjcc.v8.i17.3691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lange S.J., Ritchey M.D., Goodman A.B., Dias T., Twentyman E., Fuld J. Potential indirect effects of the COVID-19 pandemic on use of emergency departments for acute life-threatening conditions - United States, January-May 2020. Am J Transplant. 2020;20(9):2612–2617. doi: 10.1111/ajt.16239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Place R., Lee J., Howell J. Rate of pediatric appendiceal perforation at a Children's hospital during the COVID-19 pandemic compared with the previous year. JAMA Netw Open. 2020;3(12) doi: 10.1001/jamanetworkopen.2020.27948. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lazzerini M., Barbi E., Apicella A., Marchetti F., Cardinale F., Trobia G. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc Health. 2020;4(5):e10–e11. doi: 10.1016/S2352-4642(20)30108-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Finkelstein P., Picado O., Muddasani K., Wodnicki H., Mesko T., Unger S. A retrospective analysis of the trends in acute appendicitis during the COVID-19 pandemic. J Laparoendosc Adv Surg Tech. 2021;31(3):243–246. doi: 10.1089/lap.2020.0749. [DOI] [PubMed] [Google Scholar]
- 14.Gerall C.D., DeFazio J.R., Kahan A.M., Fan W., Fallon E.M., Middlesworth W. Delayed presentation and sub-optimal outcomes of pediatric patients with acute appendicitis during the COVID-19 pandemic. J Pediatr Surg. 2020;S0022–3468(20):30756–30759. doi: 10.1016/j.jpedsurg.2020.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Velayos M., Muñoz-Serrano A.J., Estefanía-Fernández K., Sarmiento Caldas M.C., Moratilla Lapeña L., López-Santamaría M. Influence of the coronavirus 2 (SARS-Cov-2) pandemic on acute appendicitis. An Pediatr. 2020;93(2):118–122. doi: 10.1016/j.anpede.2020.04.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Nelson C.P., Kurtz M.P., Logvinenko T., Venna A., McNamara E.R. Timing and outcomes of testicular torsion during the COVID-19 crisis. J Pediatr Urol. 2020;16(6) doi: 10.1016/j.jpurol.2020.10.021. 841.e1-841.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Littman A.R., Janssen K.M., Tong L., Wu H., Wang M.D., Blum E. Did COVID-19 affect time to presentation in the setting of pediatric testicular torsion? Pediatr Emerg Care. 2021;37(2):123–125. doi: 10.1097/PEC.0000000000002333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mansbach J.M., Forbes P., Peters C. Testicular torsion and risk factors for orchiectomy. Arch Pediatr Adolesc Med. 2005;159(12):1167–1171. doi: 10.1001/archpedi.159.12.1167. [DOI] [PubMed] [Google Scholar]
- 19.Bayne C.E., Villanueva J., Davis T.D., Pohl H.G., Rushton H.G. Factors associated with delayed presentation and misdiagnosis of testicular torsion: a case-control study. J Pediatr. 2017;186:200–204. doi: 10.1016/j.jpeds.2017.03.037. [DOI] [PubMed] [Google Scholar]
- 20.Johnston J.W., Larsen P., El-Haddawi F.H., Fancourt M.W., Farrant G.J., Gilkison W.T. Time delays in presentation and treatment of acute scrotal pain in a provincial hospital. ANZ J Surg. 2015;85(5):330–333. doi: 10.1111/ans.12601. [DOI] [PubMed] [Google Scholar]