Abstract
We present operative, postoperative, oncologic and functional outcomes of genital tract sparing robot-assisted laparoscopic radical cystectomy, bilateral extended pelvic lymph node (LN) dissection and intracorporeal Studer pouch construction on five female patients with bladder cancer. One of the cases had concomitant nephroureterectomy performed due to a non-functioning kidney. Median patient age, mean operation time, median estimated blood loss and mean duration of hospital stay were 59 (39–78), 462 ± 25, 400 (50–970), 8.8 ± 2.5, respectively. Pathologic stages were pTis (n=1), pT1 (n=1), pT3 (n=1), pT4a (n=1) and pT4b (n=1). Mean LN yield was 32.4 ± 8.9. Positive surgical margins were detected in 2 patients with pT4 diseases. Only minor complications developed that were resolved with medical treatment. Two patients had no, 1 patient had mild, and 2 patients had moderate daytime incontinence. One patient had good, 3 patients had fair, and 1 had poor night-time incontinence. This complex robotic surgery can be performed safely with acceptable short-term surgical, oncological and functional outcomes.
Keywords: female robotic cystectomy, genital tract preservation, intracorporeal Studer pouch, paravaginal nerve sparing, bladder cancer
Introduction
Gynecologic-tract sparing radical cystectomy (RC) in female patients with bladder cancer has attracted attention. Although an increasing number of publications exists in the literature related to robot-assisted laparoscopic radical cystectomy (RARC) in females, to date, very few authors have described gynecologic-tract sparing RARC.1–5 Herein, we report surgical, oncologic and functional outcomes of five cases where we performed gynecologic-tract sparing RARC with intracorporeal Studer pouch reconstruction.
Materials and Methods
This study was conducted in accordance with the declaration of Helsinki. Informed consent to participate in the study prior to the study commencement was obtained from the patients. Patients also gave consent to have their data published. Following internal review board approval of Koç University, five female patients with muscle invasive urothelial carcinoma in the bladder were included. The selection criteria for the technique were patients’ choice and tumors located except bladder neck or tumors with no suspicion of uterine infiltration. Radiologic work-up revealed no systemic metastasis but a non-functioning kidney in one patient. Gynecologic-tract sparing RARC with bilateral extended pelvic lymph node (LN) dissection and intracorporeal Studer pouch reconstruction was performed in all patients (Figure 1). Additionally, a concomitant right robotic nephroureterectomy was performed in one patient. In the present case series, all patients underwent genitalia preserving RARC preserving the uterus, fallopian tubes, ovaries and vagina.
Figure 1.
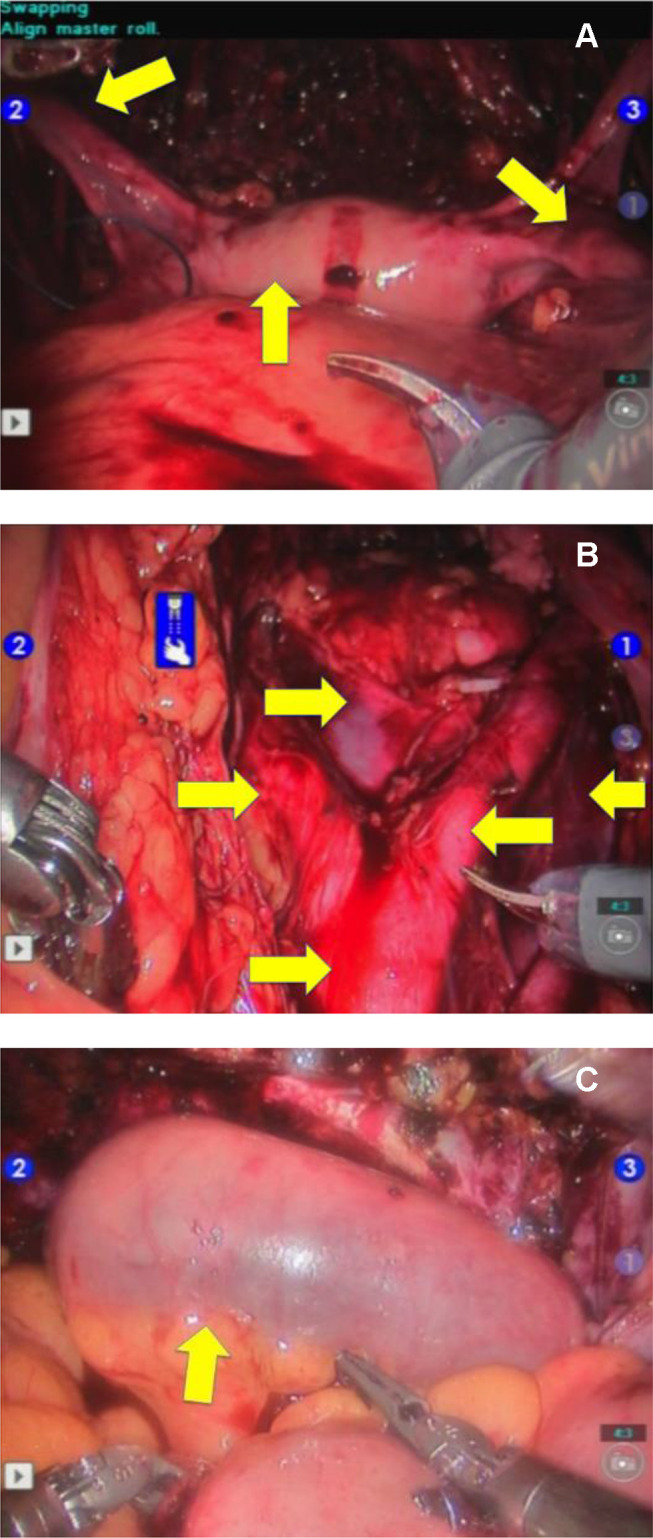
Steps of the operation. (A) Completed robot-assisted laparoscopic radical cystectomy with preservation of uterus and ovaries (arrows). (B) Appearance of extended pelvic lymph node dissection. Arrows: abdominal aorta and associated major vasculature. (C) Appearance of completed intracorporeal Studer pouch distended with sterile saline solution (arrow).
Results
Patients’ characteristics, operative-postoperative parameters, pathologic parameters, complications and functional outcomes are presented in Table 1. Only minor complications developed that were resolved with medical treatment. Post-renal kidney failure developed in patient-3 during postoperative 31–90 days with grade-II hydronephrosis during ultrasound decreased urine output and increased serum creatinine. Bilateral double-J stents were inserted via flexible ureterorenoscopy. During follow-up, urine output increased and serum creatinine dropped down to normal limits. Double-J stents were removed after 3 months (Table 1). None of our patients needed clean intermittent catheterization during follow-up.
Table 1.
Patient Characteristics Including Demographics, Operative-Postoperative Parameters, Pathologic Parameters, Complications and Functional Outcomes
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | |
|---|---|---|---|---|---|
| Patient age: (years) | 57 | 59 | 63 | 78 | 39 |
| BMI: (kg/m2) | 40 | 26 | 35 | 24 | 24 |
| ASA Score: | 3 | 2 | 2 | 3 | 1 |
| Previous abdominal surgery history: | None | Appendectomy, Cesarean section |
Laparoscopic cholecystectomy | Appendectomy | Abdominoplasty |
| Co-morbid diseases: | Hypertension | None | Hypertension | Hypertension | None |
| Smoking history: | 1 package/day (40 years) |
None | None | 1 package/day (20 years) |
None |
| Presence of any type of preoperative urinary incontinence: | None | None | None | Urgency incontinence | None |
| Premenopausal/Postmenopausal state: | Postmenopausal | Postmenopausal | Postmenopausal | Postmenopausal | Premenopausal |
| Bilateral NVB-sparing: | Yes | Yes | Yes | Yes | Yes |
| Anomalies detected during surgery: | None | None | None | Severe intra-peritoneal adhesions | Tumor infiltration into pelvic bone |
| Estimated blood loss: (mL) | 800 | 150 | 400 | 950 | 50 |
| Bilateral extended lymph node dissection: | Yes | Yes | Yes | Yes | Yes |
| Lymph node yield: n | 39 | 30 | 30 | 43 | 20 |
| Urinary diversion: | Intracorporeal | Intracorporeal | Intracorporeal | Intracorporeal | Intracorporeal |
| Urinary diversion type: | Studer | Studer | Studer | Studer | Studer |
| Concomitant robotic surgery: | Right radical nephroureterectomy | None | None | None | None |
| Operative time: (min) | 440 + 130 (nephroureterectomy time including patient re-positioning and robot de-docking and re-docking) |
370 | 480 | 540 | 480 |
| Overall (hours): | 9.5 | 6.2 | 8 | 9 | 8 |
| Radical cystectomy: | 150 min | 110 min | 150 min | 170 | 190 |
| Bilateral extended lymph node dissection: | 110 min | 90 min | 130 min | 210 | 120 |
| Intracorporeal Studer pouch reconstruction: | 180 min | 170 min | 200 min | 160 | 170 |
| Pathologic stage (pT): | pT3 | pTis | pT1 | pT4a | pT4b |
| Number of metastatic lymph nodes: n | 5 | 0 | 0 | 2 | 0 |
| Surgical margins: | Negative | Negative | Negative | Positive | Positive |
| Time to liquid diet: (days) | 1 | 2 | 2 | 3 | 2 |
| Time to regular diet: (days) | 6 | 3 | 3 | 7 | 3 |
| Time to ambulation: (days) | 1 | 3 | 2 | 3 | 1 |
| Abdominal drain removal time: (days) | 6 | 7 | 7 | 8 | 8 |
| Length of hospital stay: (days) | 6 | 8 | 8 | 13 | 9 |
| Follow-up: (months) | 24 | 10 | 7 | 26 | 7 |
| Complications due to modified Clavien Classification: | |||||
| 0–30 day (Peri-operative period) | |||||
| Minor complication (Grade 1 and 2): n | 1: UTI | 2: Abdominal pain and UTI | None | Abdominal pain and UTI | Abdominal pain |
| Major complication (Grade 3–5): n | None | None | None | None | None |
| 31–90 day period | |||||
| Minor complication (Grade 1 and 2): n | None | None | None | None | None |
| Major complication (Grade 3–5): n | None | None | Post-renal kidney failure | None | None |
| Postoperative readmission rates | |||||
| 0–30 day (Peri-operative period) | |||||
| Due to minor complications: n | None | None | None | None | None |
| Due to major complications: n | None | None | None | None | None |
| 31–90 day period | |||||
| Due to minor complications: n | None | None | None | None | None |
| Due to major complications: n | None | None | Bilateral double J stents were inserted | None | None |
| Postoperative urinary continence evaluation: | |||||
|
Day-time incontinence: (None/Mild/Moderate/Severe) |
Moderate (urge incontinence) |
Mild (urge incontinence) |
None | Moderate (urge incontinence) |
None |
|
Night-time incontinence: (Good/Fair/Poor) |
Fair | Fair | Fair | Poor | Good |
| Current sexual function: | Sexually inactive | Sexually inactive | Sexually inactive | Sexually inactive | Sexually inactive |
Notes: Complications were graded according to modified-Clavien system. Day-time urinary incontinence was measured as none (0–1 security pad/day), mild (1–2 pads/day), moderate (3 pads/day) and severe (>3 pads/day) described by Lantz et al. Night-time urinary incontinence was measured as good (dry with no protection), fair (dry with one awakening) and poor (wet, leakage and incontinence during sleep) described by Kulkarni et al.4
Abbreviations: BMI, body mass index; ASA, American Society of Anesthesiologists; NVB, neurovascular bundle; UTI, urinary tract infection.
Discussion
In the literature, a limited number of publications exist related to female cystectomy with preservation of the internal genital organs. Salem et al reported the pathological findings of gynecologic organs obtained in female RC (n=250) performed for urothelial carcinoma.3 Malignancy was identified in 1 uterus and 11 vagina specimens, including invasive urothelial carcinoma, all of which were clearly identified intraoperatively. They concluded that preservation of internal genitalia should be considered in selected cases after careful preoperative assessment.6 In a larger study from Egypt, pathological findings of gynecologic organs obtained at female RC (n=609) were reported and gynecologic organ involvement was detected in 2.6% of the cases. No primary genital cancers were identified. Gynecologic organ involvement was significantly more frequent in high-grade tumors and in transitional cell cancer type. Although statistically not significant, posterior wall tumors were more frequently associated with genital involvement compared to other sites. They also concluded that routine removal of uninvolved gynecologic organs during RC in women was not mandatory.7 Therefore, preservation of the internal genital organs without any clinical suspicion of involvement during female RC seems to be safe. Additionally, Bai et al published a retrospective propensity score-matched study including 135 females who underwent RC. Among 51 reproductive organ sparing RC; operative time was shorter, bowel recovery was quicker, the incidence of complications and estimated blood loss was lower than only RC group (n=84).8
Roshdy et al published their 7 years of genitalia sparing open cystectomy experience in 24 female patients. Pathological examination revealed only one locally advanced disease which could not detected by preoperative imaging studies in their study. In their 48 months of follow-up period, the overall survival rate was 91.6%. Day time and night urinary continence rates were 95.4% and 90.2%, respectively.3 Ali-El-Dein et al reported the outcomes of 15 female cases who underwent genitalia sparing open RC with orthotopic neobladder reconstruction. They included patients with clinical stage T2bN0M0 or less disease, unifocal tumors away from the trigone, sexually active young women and without any clinical suspicion of the involvement of internal genitalia by tumor. During a mean follow-up of 70±21 months, no recurrence was detected in the retained genital organs. Among women eligible for functional evaluation, daytime and nighttime continence were achieved in 13/13 (100%) and 12/13 (92%), respectively. Chronic urinary retention was not noted. The urodynamic parameters were comparable in the available patients with and without genital preservation. Sexual function was detected as significantly better in these patients than in others without genital preservation.9 In their series, one of the patients underwent RARC. In a review, genitalia sparing RC was found to have additional functional benefits in carefully selected patients.10
In a large open series, Jentzmik et al reported the results of 241 women with organ-confined bladder cancer underwent radical cystectomy with subsequent urinary diversion including 50 (20.7%) with ureterocutaneostomy, 70 (29.0%) with ileal conduit, and 121 (50.2%) with ileal neobladder recon-struction. Daytime and nighttime urinary continence were reported by 82.4 and 76.5%, respectively, after a median follow-up of 6.1 years. These rates were higher than our series. In our series, the median follow-up time was shorter. With longer follow-up times, higher continence rates are expected.11.
Currently, the number of centers performing genital sparing RARC is very limited. In 2004, Menon et al described RARC with preservation of urethra, uterus, vagina, and both ovaries in 2 female patients. Urinary reconstruction was performed extracorporeally.2 Hosseini et al stated that in cases when a vaginal-sparing dissection is planned and no suspicion of tumor invasion towards the uterus exists, the uterus can be dissected separately.1 Tuderti et al performed 11 genital sparing RARC. Daytime and nighttime urinary incontinence were 90.9% and 86.4%, respectively. In the first year follow-up, 72.7% of the females were sexually active. During a median 28 months of follow-up, no recurrences were detected.5 Hussein et al described a detailed step-by- step approach of another robot-assisted intracorporeal orthotopic, ileal neobladder which that followed the general principles of a “W”-configuration (Hautmann’s) orthotopic neobladder. Among 5 patients, they reported no pT3/4 patients or surgical margin positivity.12 In our experience, operation times were acceptable in all cases. Surgical margin was positive in two patients with pT4a and pT4b diseases and sufficient LN yields were obtained in all cases. We had only few minor early postoperative complications. One of the patients who experienced post-renal failure between postoperative 31–90 days was treated with bilateral double-J stent insertion. Regarding functional outcomes, although all patients were sexually not active, they had promising daytime and night-time urinary continence. Although our surgical experience currently includes only five patients, we have shown that genitalia sparing RARC with intracorporeal Studer pouch reconstruction is a safe and feasible minimally invasive procedure with acceptable short-term oncologic and functional outcomes.
Conclusion
An increasing number of publications exist in the literature related to robot-assisted laparoscopic radical cystectomy (RARC) in females, and, to date, very few authors have described gynecologic-tract sparing RARC. Although our surgical experience currently includes only five patients, we have shown that genitalia sparing RARC with intracorporeal Studer pouch reconstruction is a safe and feasible minimally invasive procedure with acceptable short-term oncologic and functional outcomes in carefully selected patients.
Funding Statement
There is no funding to report.
Disclosure
The authors reported no conflicts of interest for this work.
References
- 1.Hosseini A, Adding C, Nilsson A, Jonsson MN, Wiklund NP. Robotic cystectomy: surgical technique. BJU Int. 2011;108(6 Pt 2):962–968. doi: 10.1111/j.1464-410X.2011.10566.x [DOI] [PubMed] [Google Scholar]
- 2.Menon M, Hemal AK, Tewari A, et al. Robot-assisted radical cystectomy and urinary diversion in female patients: technique with preservation of the uterus and vagina. J Am Coll Surg. 2004;198(3):386–393. doi: 10.1016/j.jamcollsurg.2003.11.010 [DOI] [PubMed] [Google Scholar]
- 3.Roshdy S, Senbel A, Khater A, et al. Genital sparing cystectomy for female bladder cancer and its functional outcome; a seven years’ experience with 24 cases. Indian J Surg Oncol. 2016;7(3):307–311. doi: 10.1007/s13193-015-0462-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kulkarni JN, Rizvi SJ, Acharya UP, Kumar KS, Tiwari P. Gynecologic-tract sparing extra peritoneal retrograde radical cystectomy with neobladder. Int Braz J Urol. 2008;34(2):180–187;discussion 187–190. doi: 10.1590/S1677-55382008000200008 [DOI] [PubMed] [Google Scholar]
- 5.Tuderti G, Mastroianni R, Flammia S, et al. Sex-sparing robot-assisted radical cystectomy with intracorporeal padua ileal neobladder in female: surgical technique, perioperative, oncologic and functional outcomes. J Clin Med. 2020;9(2):2. doi: 10.3390/jcm9020577 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Salem H, El-Mazny A. A clinicopathologic study of gynecologic organ involvement at radical cystectomy for bladder cancer. Int J Gynaecol Obstet. 2011;115(2):188–190. doi: 10.1016/j.ijgo.2011.05.026 [DOI] [PubMed] [Google Scholar]
- 7.Ali-El-Dein B, Abdel-Latif M, Mosbah A, et al. Secondary malignant involvement of gynecologic organs in radical cystectomy specimens in women: is it mandatory to remove these organs routinely? J Urol. 2004;172(3):885–887. doi: 10.1097/01.ju.0000133986.29257.bf [DOI] [PubMed] [Google Scholar]
- 8.Bai S, Yao Z, Zhu X, et al. The feasibility and safety of reproductive organ preserving radical cystectomy for elderly female patients with muscle-invasive bladder cancer: a retrospective propensity score-matched study. Urology. 2019;125:138–145. doi: 10.1016/j.urology.2018.09.035 [DOI] [PubMed] [Google Scholar]
- 9.Ali-El-Dein B, Mosbah A, Osman Y, et al. Preservation of the internal genital organs during radical cystectomy in selected women with bladder cancer: a report on 15 cases with long term follow-up. Eur J Surg Oncol. 2013;39(4):358–364. doi: 10.1016/j.ejso.2013.02.004 [DOI] [PubMed] [Google Scholar]
- 10.Niver BE, Daneshmand S, Satkunasivam R. Female reproductive organ-sparing radical cystectomy: contemporary indications, techniques and outcomes. Curr Opin Urol. 2015;25(2):105–110. doi: 10.1097/MOU.0000000000000146 [DOI] [PubMed] [Google Scholar]
- 11.Jentzmik F, Schrader AJ, de Petriconi R, et al. The ileal neobladder in female patients with bladder cancer: long-term clinical, functional, and oncological outcome. World J Urol. 2012;30(6):733–739. doi: 10.1007/s00345-012-0837-x [DOI] [PubMed] [Google Scholar]
- 12.Hussein AA, Ahmed YE, Kozlowski JD, et al. Robot-assisted approach to ‘W’-configuration urinary diversion: a step-by-step technique. BJU Int. 2017;120(1):152–157. doi: 10.1111/bju.13824 [DOI] [PubMed] [Google Scholar]


