Figure 1: Pathogenesis of calcific aortic valve disease (CAVD).
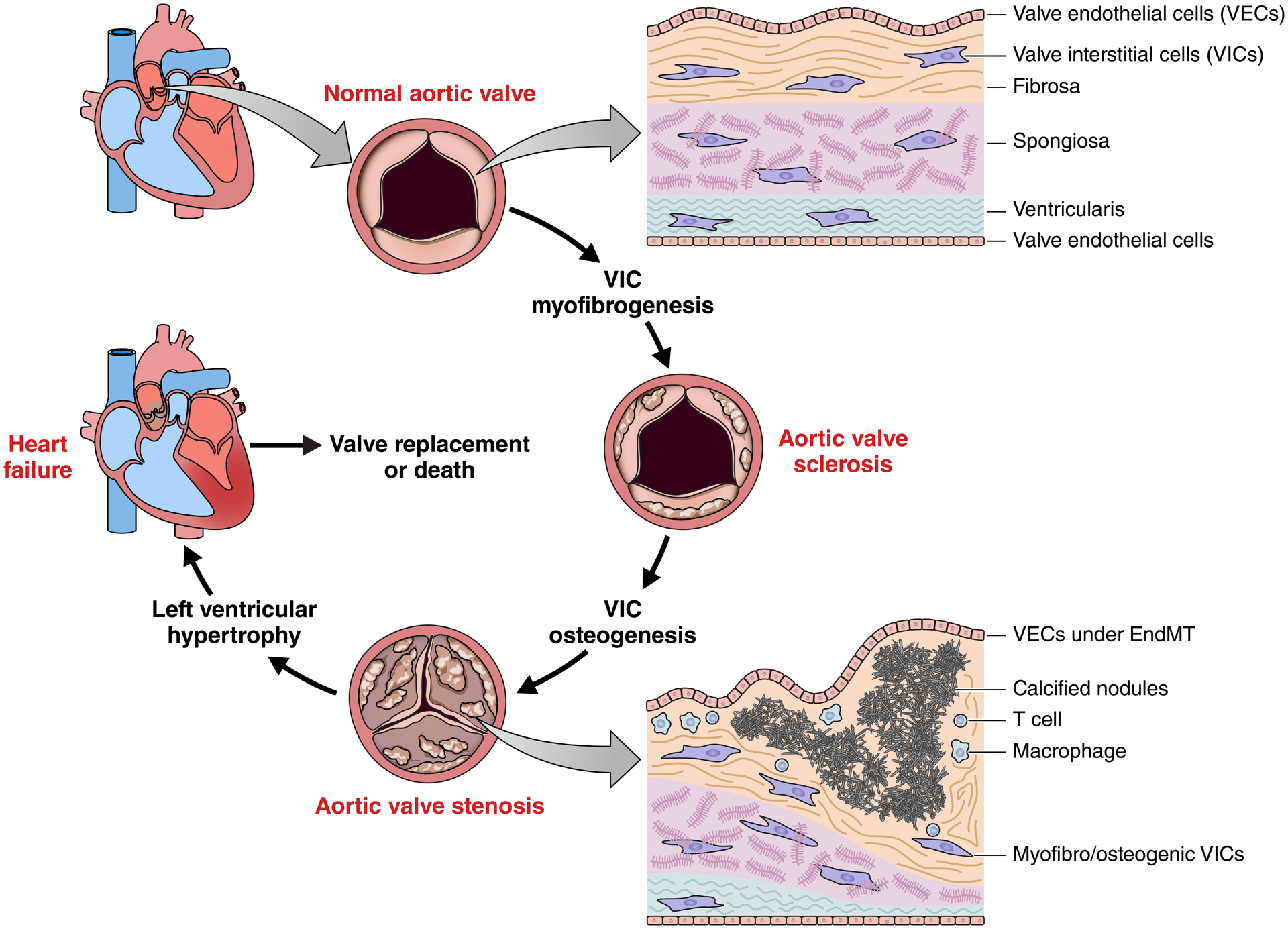
The aortic valve sits between the left ventricle and ascending aorta, and enables efficient pumping of blood in the systemic circulation. Valve leaflets are ~1mm thick, lined with valve endothelial cells (VECs), and composed of three layers with distinct extracellular matrix composition, structure, and biomechanics. During disease initiation and progression, resident valve interstitial cells (VICs) undergo myofibrogenesis, resulting in sclerotic thickening of the aortic valve. Osteogenic differentiation of VICs leads to calcification and mineralization of valvular tissues and eventual impairment of leaflet opening/closure (stenosis). The left ventricle hypertrophies as a result of this increased resistance, leading towards heart failure. Surgical/transcatheter replacement of the aortic valve is currently the only therapeutic strategy and untreated aortic stenosis suffers from very high mortality rates.
