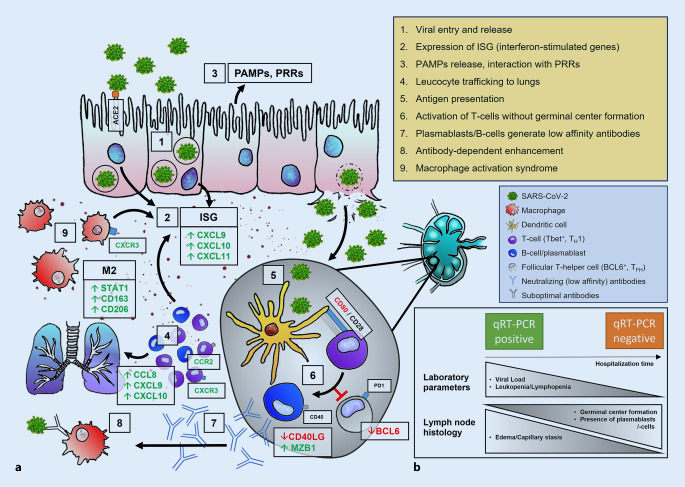
Fig. 1.
Immunopathology of SARS-CoV‑2 infection. a 1. Viral entry via ACE2, transcription of viral proteins and assembly, release of daughter virions. 2. Up-/dysregulation of ISG, cytokines, and chemokines. 3. Activation of PRRs by PAMPs. 4. Leukocyte trafficking into the lungs resulting in lymphopenia. 5. Antigen presentation in lymph nodes; activation of T cells (purple; e.g., by CTLA4/CD28) in a TH1 (Tbet+)-predominant milieu. 6. Inhibition of BCL6+ TFH cells (gray) disrupts germinal center formation, resulting in the activation of extrafollicular B blasts and, thus, an increase in plasmablasts (blue). 7. Release of specific (low-affinity) antibodies (blue) against SARS-CoV‑2. 8. Antibody-dependent enhancement. 9. Macrophage activation syndrome with predominance of an M2 phenotype including HLH and cytokine storm. b Temporal evolution of laboratory parameters and histology in COVID-19 lymph nodes. Short hospitalization time: high viral load, severe lymphopenia, absence of germinal centers accompanied by severe edema/capillary stasis and plasmablast accumulation. Longer hospitalization time: lower viral load, regressing lymphopenia, incipient (delayed) germinal center formation. ACE2 angiotensin-converting enzyme 2, HLH hemophagocytic lymphohistiocytosis, ISG interferon-stimulated gene, PAMPs pathogen-associated molecular patterns, PRRs pattern recognition receptors, RT-PCR reverse transcriptase polymerase chain reaction; green upregulated proteins, red downregulated proteins